Remark
| 1) Why was this study conducted? |
| The definitive control of the vascular injury represents a surgical challenge, especially if the patient is hemodynamically unstable. This article proposes the management of peripheral vascular trauma following damage control surgery principles. |
| 2) What were the most relevant results of the study? |
| The surgical approaches according to the anatomical injured region should be selected. We propose two novel approaches to access the axillary and popliteal zones. The priority should be to reestablish limb perfusion via primary repair or damage control techniques (vascular shunt or endovascular approach). All permanent or temporary vascular procedures should be followed by a definitive repair within the first 8 hours. |
| 3) What do these results contribute? |
| A prompt and early intervention is required to improve outcomes and avoid complications. When facing hemodynamically unstable patients, control of hemorrhage becomes paramount, followed by reestablishing limb perfusion via primary repair or damage control techniques, if required and indicated. |
Introduction
Vascular injuries of the extremities are uncommon in civilian trauma. With a prevalence of 2% in blunt trauma and 4% in penetrating, their management remains a surgical and clinical challenge given the need for prompt hemorrhage control. A delay in intervention can lead to a patient´s exsanguination or can be associated with ischemic complications threatening the patient’s life and/or the viability of the limb. These types of injuries are typically prone to external compression in the prehospital care setting. Nevertheless, achieving definitive control of the vascular injury represents a surgical challenge, especially if the patient is hemodynamically unstable. This article proposes the management of peripheral vascular trauma following damage control surgery principles.
This article is a consensus that synthesizes the experience earned during the past 30 years in trauma critical care management of the severely injured patient from the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia which is made up of experts from the University Hospital del Valle "Evaristo García", the University Hospital Fundación Valle del Lili, the Universidad del Valle and Universidad Icesi, the Asociación Colombiana de Cirugía, the Pan-American Trauma Society and the collaboration of international specialists of the United States of America, Europe, Japan, South Africa, and Latin America.
Epidemiology
Peripheral vascular trauma is more prevalent in the military than in civilian trauma 1-3. Falls from great heights, work-related accidents, and motorcycle crashes are common causes of vascular injury in blunt trauma 2-4. Penetrating trauma by gunshot or stab wounds prevails in developing countries such as Latin-America 5. A 30-year review study conducted by Mattox et al found 5,760 patients with vascular injuries with an overall prevalence of 19% involving the lower extremities and 14% involving the upper. The most common injured vessel of the lower extremity was the femoral artery in 45% , the femoral vein in 25% and the popliteal artery in 14%. Meanwhile, vascular injuries of the upper extremities involved the brachial artery in 52% and the radial or cubital artery in 30% 6,7. These results did not vary much from those reported previously in North America, Europe or Latin-America 8-12. Complete or partial transection of the vessel was the predominant type of injury 12.
The Prospective Observational Vascular Injury Treatment (PROOVIT) registry collected information on 542 vascular trauma patients, in which 241 presented with peripheral vascular injuries. They reported conservative management in 47% (66/141) of the lower extremity injuries and 33% (30/92) in the uppers. An initial open surgical approach was performed in 51% (72/141) in the lower extremity injuries and 71% (65/92) in the uppers. The primary repair rate was 78% (56/72) in the lower extremity vascular injuries and 78% (51/65) in the uppers. Prehospital tourniquet placement was used in 20% (47/233) of all peripheral vascular injury cases and prophylactic fasciotomy was performed in 33 and decompressive fasciotomy in 19 12. Similarly, D’Alessio et al reported a series of 56 patients from Milan, Italy, in which 75% of peripheral vascular trauma had associated orthopedic and/or neurological injuries. The open surgical approach was performed in 85%, while the remaining 15% underwent an endovascular repair with an overall limb preservation rate of 90.4%. Inferior limb amputation was required in 5 cases, three patients had prosthetic graft infection, two patients suffered graft rejection and the overall post-operative mortality was 5.7% 13.
Initial Approach
All efforts must be directed towards stabilizing the patient. Advanced Trauma Life Support - ATLS guidelines, the ABCDE mnemonic and damage control resuscitation principles should be followed and applied vigorously 14. Peripheral vascular trauma can be diagnosed in the initial evaluation if the presence of hard signs of injury are present or suspected in cases where soft signs exist (Table 1). Additionally, perfusion of the extremity distal to the injury site must be assessed and associated orthopedic, muscular and neurologic involvement must be ruled out. In cases where the patient is hemodynamically unstable, an emergency surgical approach is necessary. Otherwise, patients who are hemodynamically stable should undergo an ankle-brachial index and Doppler examination in the Trauma Bay. If positive, then a computed tomographic angiography (CT-Angio) to better delineate the injury 15.
Table 1 Hard and Soft Signs of Peripheral Vascular Injury
| Hard Signs | Soft Signs |
|---|---|
| ⏺ Pulsatile Bleeding | ⏺ Non-Pulsatile Bleeding |
| ⏺ Expanding/ Pulsatile Hematoma | ⏺ Non-expanding/Non-Pulsatile |
| ⏺ Loss of Distal Pulses | ⏺ Hematoma |
| ⏺ Bruit/Thrill | ⏺ Diminished Pulse |
| ⏺ History of (massive) Arterial Bleeding/Hypotension | |
| ⏺ Previously Applied Tourniquet | |
| ⏺ Neurologic Deficit | |
| ⏺ Wound in Proximity to Named Vessel |
The American Association for the Surgery of Trauma (AAST) has developed a grading scale for peripheral vascular injuries (Table 2) 16.
Table 2 American Association for the Surgery of Trauma (AAST) Classification of Peripheral Vascular Trauma. AAST Peripheral Vascular Trauma Classification
| Grade | Description |
|---|---|
| I | Digital Artery/Vein, Palmar Artery/Vein, Deep Palmar Artery/Vein, Pedis Dorsalis Artery, Plantar Artery/Vein |
| II | Cephalic/Basilic Vein, Saphenous Vein, Radial Artery, Cubital Artery |
| III | Axilary Vein, Deep/Superficial Femoral Vein, Popliteal Vein, Brachial Artery, Anterior Tibial Artery, Posterior Tibial Artery, Peroneal Artery, Tibio-Peroneal Trunck |
| IV | Deep/Superficial Femoral Artery, Popliteal Artery |
| V | Axillary Artery, Common Femoral Artery |
Surgical Approach
Step 1: Attention should be directed towards identifying all immediate life-threatening injuries following the ABCDE approach of ATLS. Both femoral arterial and venous lines should be placed immediately for blood pressure monitoring and intravenous access. In hemodynamically unstable patients, damage control resuscitation via activation of the institution’s massive transfusion protocol should be initiated 17.
Step 2: Prompt identification of all hard and/or soft vascular injury signs. Orthopedic, muscular and/or soft tissue associated injuries should be considered. Temporary bleeding control maneuvers should be performed which include: wound packing, direct manual pressure or tourniquet placement 18. If the patient remains hemodynamically unstable despite initial resuscitation efforts, the placement of a Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) should be considered and placed as an adjuvant 19,20. The patient should then be transferred to the operating/hybrid room immediately.
Step 3: The surgical approach depends on the anatomical region:
For axillary artery injuries, the patient must be placed in the supine position with the injured extremity taped to the forehead, exposing the axillary fossa. The access to the axillary artery can be achieved through an inverted “S” shaped incision starting at the pectoralis major muscle curving in the axillary fossa and ending in the arm between the bicep and tricep muscles. This incision prevents future scar retraction and functional limitation of the shoulder joint (Figure 1).
The brachial artery lies in the bicipital groove that extends from the axillary fossa to the center of the ante-cubital fossa. It´s bifurcation can be approached by an “S” incision starting from the medial border of the arm, crossing through the ante-cubital fossa and ending in the lateral border of the proximal forearm.
The radial and ulnar arteries are accessed via direct vertical incisions.
The femoral artery is accessed via a vertical incision over the sartorius muscle before identifying a palpable pulse or ultrasound guidance in a pulseless artery.
The popliteal artery can be accessed via a posterior “S” shaped incision starting in the postero-medial region of the thigh, crossing parallel in the mid popliteal fossa and ending vertically in the postero-lateral region of the leg. After skin incision, the subcutaneous tissue is dissected down the midline until the popliteal vessels are exposed. Be aware of both the tibial and peroneal nerves that are in the vicinity (Figure 2).
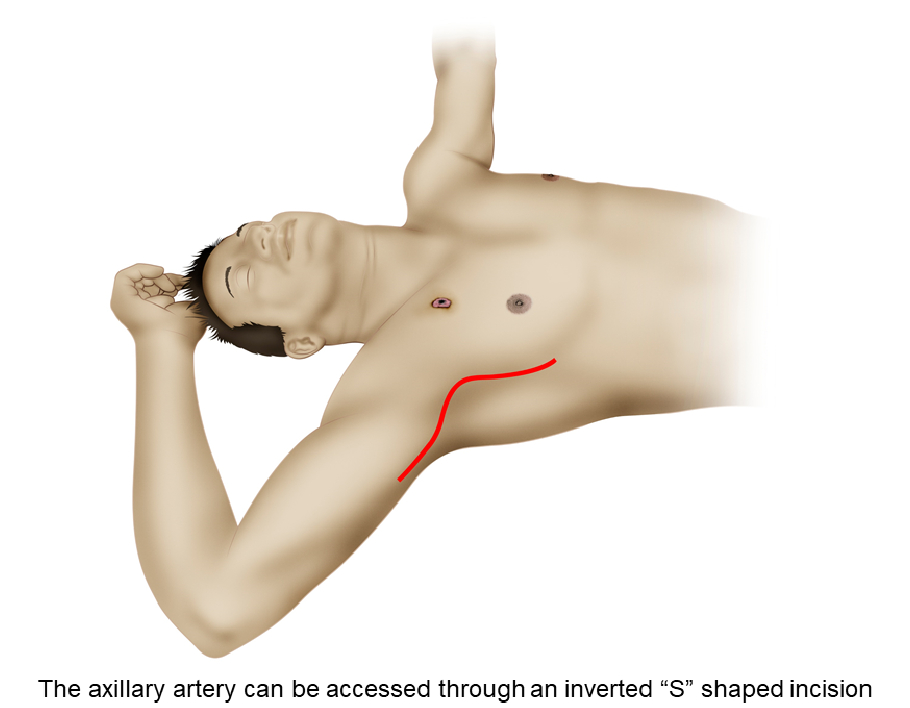
Figure 1 Surgical approach to the axillary artery. The axillary artery can be accessed through an inverted “S” shaped incision starting at the pectoralis major muscle, curving in the axillary fossa and ending in the arm between the bicep and tricep muscles. This incision prevents future scar retraction and functional limitation of the shoulder joint.
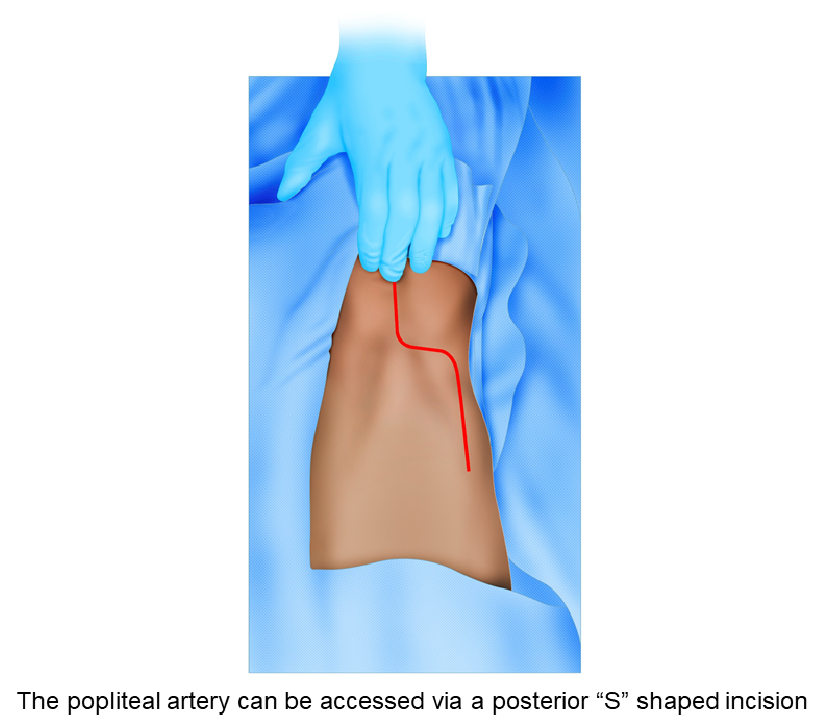
Figure 2 Surgical approach to the popliteal artery. The popliteal artery can be accessed via a posterior “S” shaped incision starting in the posteromedial region of the thigh, crossing parallel in the mid popliteal fossa and ending vertically in the postero-lateral region of the leg. Afterward, subcutaneous tissue should be dissected down the midline until the popliteal vessels are exposed, carefully not injuring the tibial and/or peroneal nerves.
Step 4: Both proximal and distal control of the injury should be performed. Perform thrombectomy/embolectomy of the injured vessel routinely before definitive repair.
Step 5: Primary vascular repair is indicated if the patient is hemodynamically stable. Nevertheless, if the injured vessel requires partial resection, a primary repair can still be performed, only if the anastomosis is not under excessive tension. If the tension is excessive, an interposition graft with an autologous vein or synthetic graft can be performed. In cases of an isolated radial or cubital arterial injury and a patent palmar arch, the vessel can be ligated.
In complex vascular injuries, the persistence of hemodynamic instability or prolonged ischemia, a vascular shunt should be placed initially after proximal and distal control of the injury is obtained. The purpose of the shunt is to reperfuse the limb and limit the ischemic damage.
In cases where venous injuries cannot be primarily repaired, then the vessel should be ligated. Prophylactic fasciotomies are indicated in patients with compartment hypertension and/or impending compartment syndrome.
An endovascular approach can be performed in hemodynamically stable patients. Options include stent placement and/or thrombo-embolectomy of the injured vessel. Long-term patency rates are equivalent to those managed by open repair for proximal arterial injuries of the extremities 21,22.
Step 6: All permanent or temporary vascular procedures should have soft tissue coverage; all significant unstable fractures should be stabilized, and the wound should be packed or have a negative pressure dressing placed. All major vascular procedures should be managed postoperatively in the intensive care unit (ICU) for correction of the lethal diamond 23, serial vascular pulse checks and active clinical bedside surveillance of signs developing compartmental syndrome in cases where prophylactic fasciotomies were not performed.
Step 7: All shunted patients must return to the operating room within the first 8 hours to perform the definitive repair of the injury.
Complications
Complications include compartment syndrome, reperfusion injury and limb amputation. The amputation rate of upper extremity vascular injuries is around 1%. However, ligating the brachial artery has an amputation risk of 18 to 55%. Lower extremity vascular injuries have an overall amputation rate of 11%. Injuries of the popliteal or femoral arteries have an amputation risk of 28 to 37%, increasing up to 70% when there is a delay in presentation 24-28.
Conclusion
Peripheral vascular trauma becomes a surgical challenge for a well-trained surgeon aiming to preserve the function and perfusion of the extremity. A prompt and early intervention is required to improve outcomes and avoid complications. When facing hemodynamically unstable patients, control of hemorrhage becomes paramount, followed by reestablishing limb perfusion via primary repair or damage control techniques, if required and indicated.











 text in
text in 



