Remark
| 1) Why was this study conducted? |
| This article aims to present a proposal for the management of splenic trauma in severely injured patients. |
| 2) What were the most relevant results of the study? |
| It is our recommendation that both damage control principles and emerging endovascular technologies should be applied to achieve splenic salvage when possible. However, if surgical bleeding persists a splenectomy may be required as a definitive lifesaving maneuver. |
| 3) What do these results contribute? |
| The spleen should be salvage when it will be possible. Splenectomy should not be the first option. |
Introduction
The spleen is one of the most commonly injured organs in blunt abdominal trauma but in penetrating trauma the incidence reaches only 7 to 9%. The overall mortality of a splenic injury becomes significant when the diagnosis is delayed 1-4. Over the past couple of decades, the optimal management of a splenic injury has undergone significant transformation and nowadays it has evolved to a preferred non-operative approach even in severely injured cases 5. This approach seeks to preserve the spleen using strategies such as strict clinical observation and angio-embolization. However, the management strategy of hemodynamically unstable trauma patients with splenic injuries remains controversial 6.
The Trauma and Emergency Surgery Group (CTE) of Cali, Colombia is made up of experts from the University Hospital Fundación Valle del Lili, the University Hospital del Valle "Evaristo García", the Universidad del Valle and Universidad Icesi, the Asociación Colombiana de Cirugía, the Pan-American Trauma Society and international specialists of the United States, Europe, Japan, South Africa, and Latin America. Through a collaborative effort, we have been able to summarize a group consensus that condenses the experience obtained during the past 30 years in the management of trauma, general surgery and critical care. The aim of this article is to delineate the experience obtained by our group in the surgical management of splenic trauma in severely injured patients by proposing a management strategy that includes basic principles of damage control surgery.
Epidemiology
The spleen is one of the most commonly injured solid organs of the abdominal cavity. Between 2014 and 2016, Coccollini et al. reviewed a total of 124 patients with splenic injuries and the most prevalent mechanism of injury was blunt trauma secondary to automotive traffic accidents, followed by falls. The median Injury Severity Score (ISS) was 27 (IQR: 5-75) and half of these patients had a positive extended focused assessment with sonography for trauma (E-FAST) during initial evaluation. Seventy-two percent of the patients had mild to moderate splenic injuries (AAST Grade I-III) and 28.2% had severe injuries (AAST Grade IV-V). Non-operative management was performed in 53% (66) of the cases and 47% (58) required damage control surgery, of these 49 underwent splenectomy and 9 required open abdominal packing. The overall mortality rate was 10.5% 7. Teuben et al., performed a systematic literature review that included 608 patients with penetrating splenic trauma, in which the most prevalent mechanism of injury was gunshot wounds. Non-operative management was carried out in 14-33% of the cases and the overall mortality rate was 6-14% 8.
Initial approach and diagnosis
Initial management must be directed towards the stabilization of the patient according to the Advanced Trauma Life Support (ATLS) guidelines which include the ABC’s strategy. Both common femoral vein and artery lines should be placed. The choice between immediate surgical exploration or further extended imaging studies depends on the hemodynamic status of the patient. If the patient is hemodynamically stable or a transient responder a computed tomography angiogram (CTA) should be performed to determine if non-operative management is feasible and if angioembolization is required 6,9. However, patients with persistent hemodynamic instability (sustained systolic blood pressure ≤70 mmHg) should be immediately transferred to the operating room for an exploratory laparotomy. During the initial laparotomy, immediate control of hemorrhage should be achieved by abdomen packing and the anesthesia staff should be given enough time to complete the ongoing damage control resuscitation, via prior activation of the institution’s massive transfusion protocol. Only then, the magnitude and the anatomical involvement of the spleen should be quantified following the American Association for the Surgery of Trauma (AAST) classification (Table 1).
Table 1 AAST classification of splenic injuries 10
| Grade | Type | Description of injury |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| II | Laceration | Capsular tear, <1 cm parenchymal depth |
| Hematoma | Subcapsular, 10%-50% surface area Intraparenchymal, <5 cm in diameter | |
| III | Laceration | Capsular tear, 1-3 cm parenchymal depth that does not involve a trabecular vessel |
| Hematoma | Subcapsular, >50% surface area or expanding Ruptured subcapsular or parenchymal hematoma Intraparenchymal hematoma, > 5 cm or expanding | |
| IV | Laceration | >3 cm parenchymal depth or involving trabecular vessels |
| Laceration | Laceration involving segmental or hilar vessels producing major devascularization (> 25% of spleen) | |
| V | Laceration | Completely shattered spleen |
| Vascular | Hilar vascular injury with devascularized spleen |
In 2017, the World Society of Emergency Surgery (WSES) updated their guidelines for the diagnosis and management of splenic trauma, which includes the AAST Grade classification and the hemodynamic status of the patient (Table 2).
Table 2 WSES Splenic Trauma Classification 5
| WSES Class | AAST | Hemodynamic Status | |
|---|---|---|---|
| Minor | WSES I | I | Stable |
| Moderate | WSES II | III | Stable |
| Severe | WSES III | IV-V | Stable |
| WSES IV | I-V | Unstable |
Rationale
Despite advances in trauma critical care, the optimal surgical management strategy of splenic trauma remains controversial. We propose a surgical management that takes into account damage control principles and the use of tools such as computed tomography angiogram, angioembolization and strict clinical monitoring.
Computed Tomography Angiogram
We propose that if the patient arrives hemodynamic unstable but is a transient responder a computed tomography angiogram should be performed to determine the extent of the injury and the presence of any other associated injuries. Depending on the computed tomography angiogram findings, the patient can undergo either non-operative management or an open approach 11-13. Computed tomography angiogram has a reported sensitivity of 96% and specificity of 100% for the diagnosis of splenic injuries. For these reasons, the computed tomography angiogram prevents in 54% of cases, any unnecessary surgical interventions 6,14.
Angioembolization
Endovascular control by angiography has been reported as an important factor in obtaining splenic salvage and the subsequent reduction in mortality rates from these injuries 15,16. Moreover, some meta-analysis has proven that non-operative management with angioembolization is associated with higher rates of survival and the reduction of treatment failure rates in patients with AAST Grade IV-V injuries 6,17.
Damage Control Surgery
Splenic packing is the most important surgical management tool that a surgeon possesses to achieve active surgical hemorrhage control in the severely injured trauma patient. If surgical bleeding persists, then reinforcement of the packing should be performed, and the patient should undergo angiography for embolization. If this option is not readily available, then immediate splenectomy should be performed 10. Splenorraphy, partial splenectomy and surgical meshes have not proven any real advantage or efficacy in achieving true splenic salvage 6. As a result, it is our recommendation that both principles of damage control resuscitation and damage control surgery should be combined with emerging endovascular technologies to achieve hemorrhage control and ultimately splenic salvage, when possible.
Surgical Approach
Based on our experience we propose a new algorithm for the management of splenic trauma:
STEP 1: Attention should be directed towards identifying all immediate life-threatening injuries following the ABC mnemonic of ATLS. Both a common femoral vein and artery lines are placed for intravenous access, blood pressure monitoring and the initiation of an aggressive damage control resuscitation.
STEP 2: All patients that arrive with hemodynamic instability (sustained systolic blood pressure ≤70 mmHg) or non-transient responders should have their common femoral arterial line changed over a guidewire to a femoral sheath, followed by placement of a Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in Zone 1. This procedure should be performed in the emergency room. The REBOA becomes an important resuscitative tool that ultimately prevents hemodynamic collapse while at the same time maintains coronary and cerebral perfusion. Additionally, the institution’s massive transfusion protocol should be activated. If the patient is hemodynamically stable or a transient responder, a computed tomography angiogram should be performed to determine the extent of the damage and the presence of any other associated injuries. According to the findings, the patient can undergo either non-operative management or an open approach.
STEP 3: The hemodynamically unstable patient or the non-transient responder should be transferred immediately to the operating room for emergency exploratory laparotomy. If you are not trained or do not have a REBOA available at your institution, then we recommend aortic cross-clamping as soon as possible 18.
STEP 4: During the exploratory laparotomy, the trauma surgeon should initially control all sources of ongoing surgical bleeding and bowel contamination. As soon as these are achieved, the magnitude of the splenic injury should be determined according to the AAST classification (Table 1):
○ AAST Grade I/II/III: These injuries require prompt splenic packing. Once bleeding control has been achieved, damage control surgery should be completed (Figure 1).
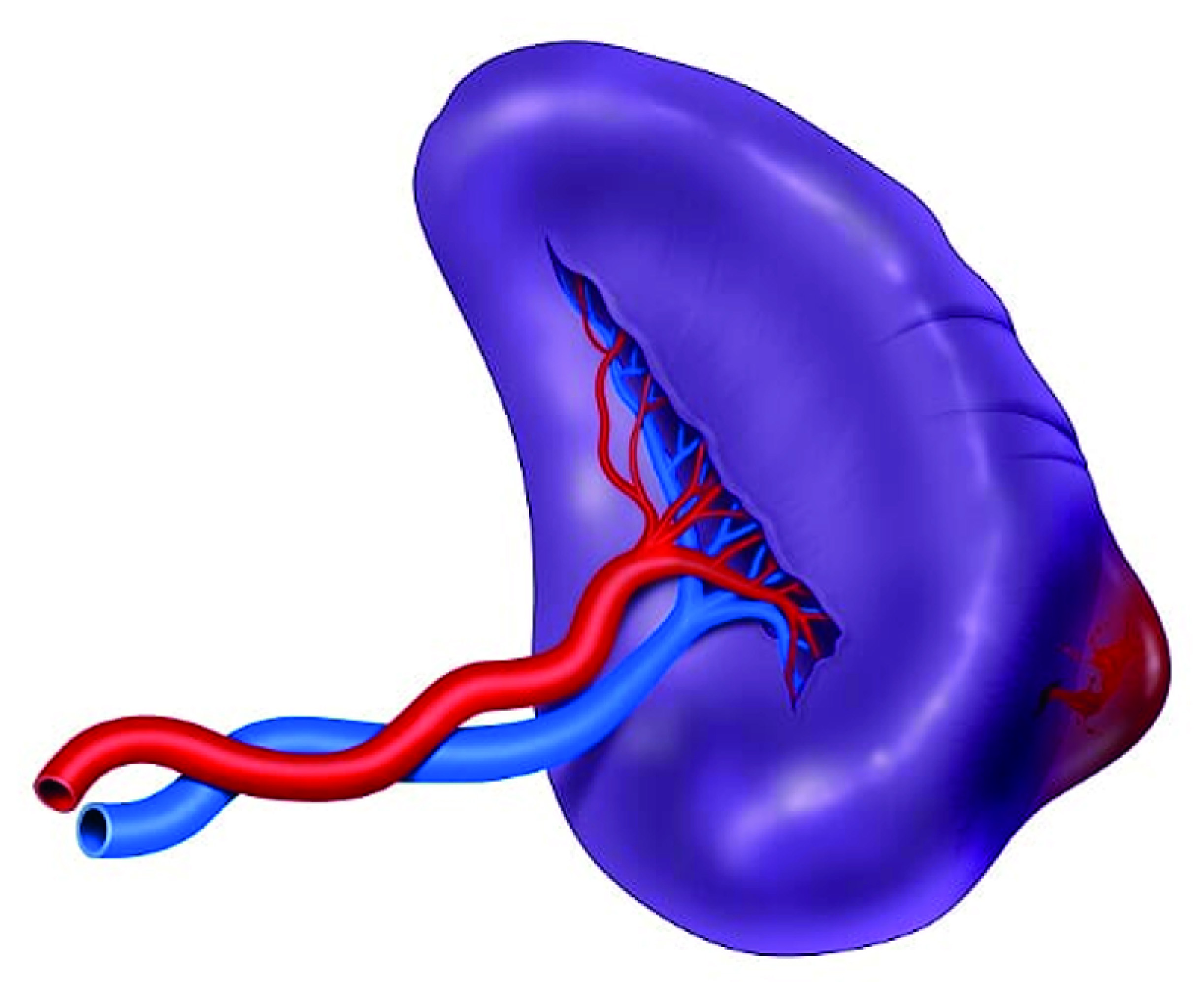
Figure 1 AAST Grade II Splenic Injury. Subcapsular splenic hematoma. These injuries require an early splenic packing. Once bleeding has been controlled, damage control surgery should be completed and the subsequent need for angiography with embolization should be assessed.
○ AAST Grade IV: These injuries also require prompt splenic packing. If hemorrhage control is achieved, damage control surgery should be completed. However, if the hemorrhage persists and the patient remains hemodynamically unstable, then a splenectomy should be considered (Figure 2).
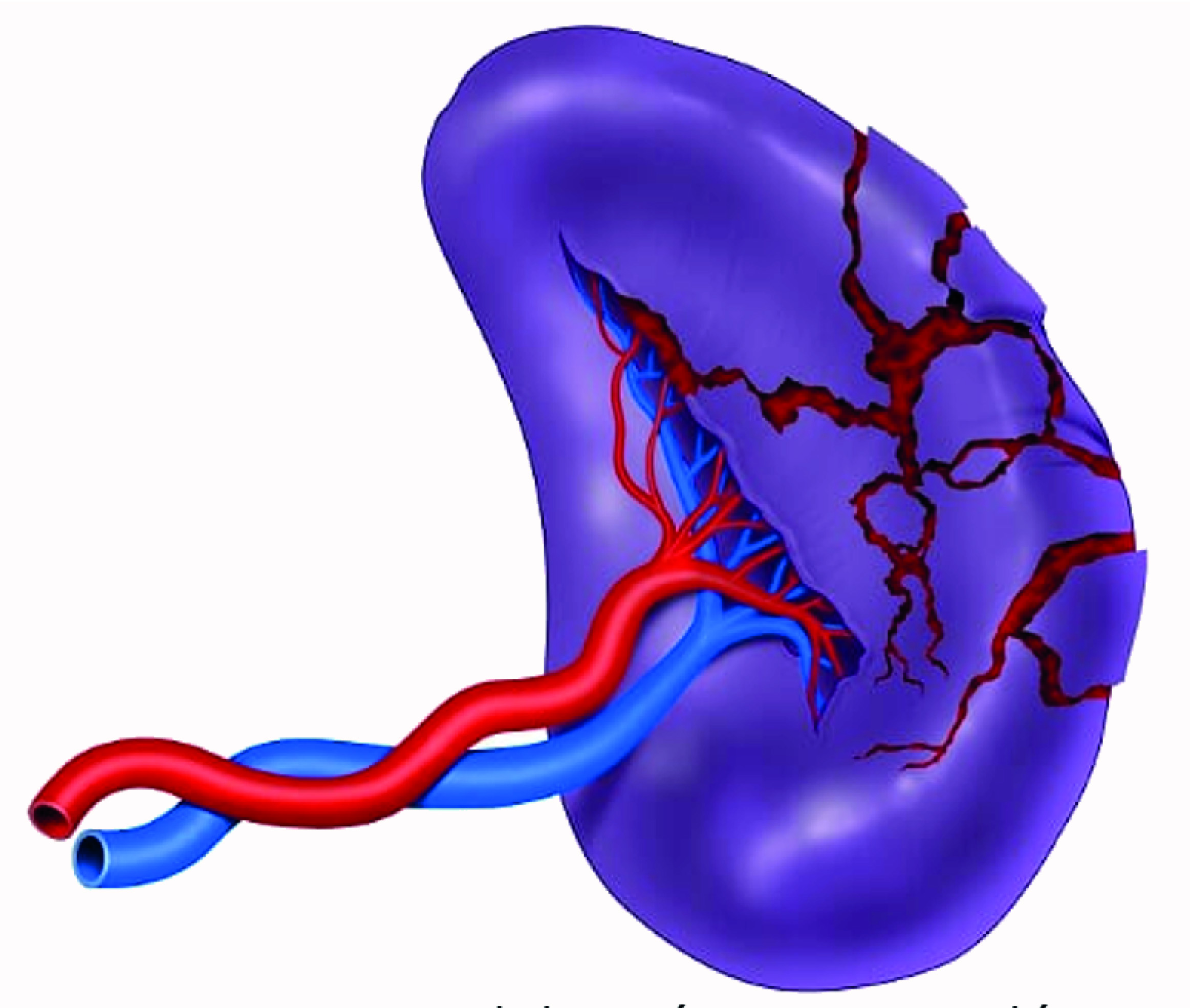
Figure 2 AAST Grade IV Splenic Injury. Massive parenchymal laceration without vascular involvement. These injuries also require prompt splenic packing. If hemorrhage control is achieved, damage control surgery should be completed, followed by angiography with embolization of any ongoing arterial bleeding. However, if the hemorrhage persists and the patient remains hemodynamically unstable, then a splenectomy should be considered.
○ AAST Grade V: Splenic injuries with complete destruction and/or devascularization require a splenectomy for hemorrhage control followed by damage control surgery (Figure 3).
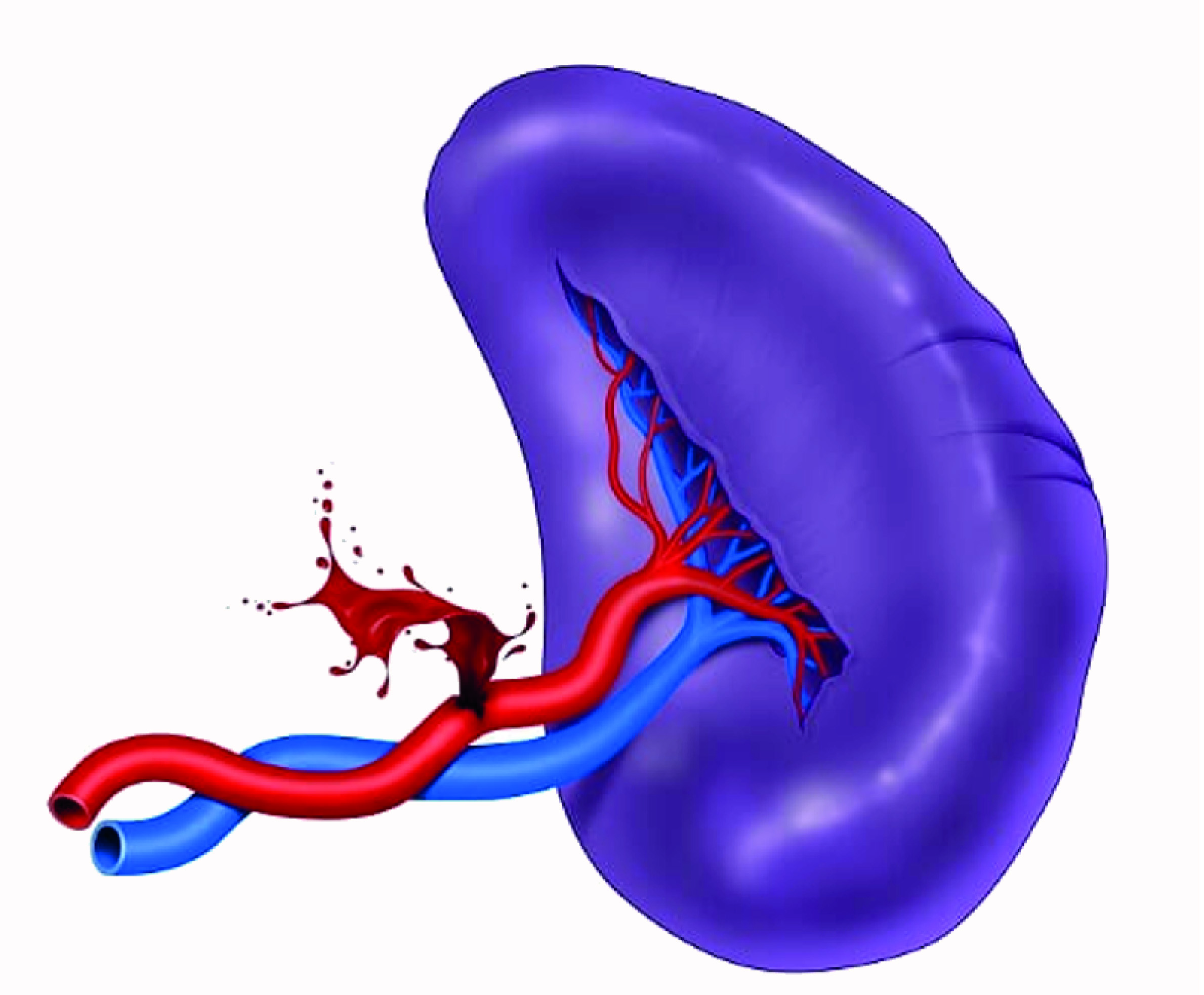
Figure 3 AAST Grade V Splenic Injury. Splenic artery involvement. Splenic injuries with complete destruction and/or devascularization require a splenectomy for hemorrhage control followed by damage control surgery.
STEP 5: Damage control surgery should be completed. Following splenic packing, the patient is left with an open abdomen and a negative pressure dressing is placed. Then, angiography with embolization of any ongoing arterial bleeding should follow. Subsequently, the patient should be transferred to the intensive care unit for correction of the lethal diamond.
STEP 6: If there is any suspicion of persistent bleeding a second angiogram with possible embolization should be considered. However, if the suspicion is associated with hemodynamic instability, the patient should be transferred immediately to the operating room for reintervention via exploratory laparotomy. In cases where the splenectomy has already been performed, selective hemostasis should follow and the abdomen should be re-packed and left open with a negative pressure dressing. The patient should then be transferred back to the ICU for completion of damage control resuscitation.
STEP 7: Within 24 to 72 hours of aggressive hemostatic resuscitation in the intensive care unit, the patient should be taken back to the operating room for packing removal, abdominal washout and definitive abdominal wall closure. However, if splenic hemorrhage persists during this reintervention, packing should be reinstated and Step 5 repeated.
Complications
Non-operative management is the gold standard for hemodynamically stable blunt splenic trauma patients with a reported rate of therapeutic failure between 4-15% 19-22. The main complication is persistent bleeding which entails higher transfusion requirements and morbidity rates 23-25.
Patients suffering from penetrating splenic trauma often have other associated intra-abdominal injuries which can involve the pancreas, colon and diaphragm. Angioembolization in penetrating splenic trauma has an overall success rate of 73 to 100% 26-28. It is well established in the literature that as the degree of splenic injury increases also does the requirement of an open surgical management 29. According to the AAST classification, Grade I injuries require open surgical management in 33% of the cases and Grade V injuries in 84%. The most dreadful post-operative complication of splenectomized patients is the development of an overwhelming post-splenectomy infection, which is caused by encapsulated organisms such as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis. To avoid this complication, all patients who undergo splenectomy should receive a pre-established post-operative institutional vaccination protocol 6,30-32.
Conclusion
The optimal management of splenic trauma in the severely injured patient is controversial. It is our recommendation that both principles of damage control resuscitation and damage control surgery should be combined with emerging endovascular technologies to achieve splenic salvage, when possible. However, if surgical bleeding persists a splenectomy should be considered as a definitive lifesaving maneuver.











 text in
text in 



