Remark
| 1) Why was this study conducted? |
| Thoracic trauma with the involvement of the great vessels is a surgical challenge due to the complex and restricted anatomy of these structures and its association with adjacent organ damage. The aim of this article is to delineate the experience obtained in the surgical management of thoracic vascular injuries via the creation of a practical algorithm that includes basic principles of damage control surgery. |
| 2) What were the most relevant results of the study? |
| Early application of a resuscitative median sternotomy together with a zone 1 resuscitative endovascular balloon occlusion of the aorta (REBOA) in hemodynamically unstable patients with thoracic outlet vascular injuries improves survival by providing rapid stabilization of central aortic pressure and serving as a bridge to hemorrhage control. Damage control surgery principles should also be implemented when indicated followed by definitive repair once the correction of the lethal diamond has been achieved. |
| 3) What do these results contribute? |
| We have developed an easy to follow six-step management algorithm that clearly illustrates the surgical care of patients with thoracic outlet vascular injuries. |
Introduction
Thoracic vascular trauma is associated with high mortality and is the second most common cause of death in patients with trauma following head injuries 1,2. Less than 25% of patients with a thoracic vascular injury arrive alive to the hospital and more than 50% die within the first 24 hours 3. Furthermore, thoracic trauma with the involvement of the great vessels is a surgical challenge due to the complex and restricted anatomy of these structures and its association with adjacent organ damage 4. This article aims to delineate the experience obtained by the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia, in the surgical management of thoracic vascular injuries via the creation of a practical algorithm that includes basic principles of damage control surgery.
Epidemiology
Friend et al., in a series of 75 patients with thoracic vascular trauma over 15 years at the Royal Perth Hospital in Australia, found that the most prevalent mechanism was blunt trauma from road traffic accidents. Also, the most commonly involved vascular structure was: the thoracic aorta in 39 cases, followed by the subclavian artery in 8 and the pulmonary artery in 3. The most frequently associated injuries were: hemothorax, skull fractures, rib fractures, pulmonary contusions and/or pelvic fractures, with an overall mortality rate of 43% 5. Mattox et al. reported one of the largest recorded series of vascular trauma of civilian origin, in which 576 patients with thoracic vascular trauma were seen between 1958-1988. In this study, the majority of the injured vessels included were: the descending thoracic aorta (89), the pulmonary artery (79), and the innominate artery (42) 6. The literature has also confirmed that injuries involving the thoracic aorta and/or pulmonary vessels have an extremely high mortality rate and most of them die at the scene 7.
A retrospective review of all patients suffering from thoracic vascular trauma at a level one regional trauma center in Cali, Colombia, was performed from December 2014 to December 2019. All patients with a thoracic vascular injury that required an aortic occlusion via placement of a Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) and a resuscitative median sternotomy were included. The study aimed to describe the vascular injuries that required REBOA placement.
The study was approved by the institutional ethics and review board committees. The decision to place a REBOA resided on the treating trauma surgeon and the most common indication was sustained hypotension (systolic blood pressure (SBP) <90 mmHg) that did not respond to initial resuscitation. Therefore, all REBOA catheters were placed in Zone 1 by a separate surgical team while another surgical team performed the resuscitative median sternotomy.
A total of 56 patients were treated by aortic occlusion via REBOA, of which 23 had chest trauma, 17 required a simultaneous resuscitative median sternotomy. The most common mechanism of injury was penetrating by gunshot wounds and none of the patients presented with cardiac arrest upon admission to the emergency room. All REBOA’s were placed in the operating room. The median systolic blood pressure pre-aortic occlusion was 50 mmHg. REBOA was positioned in Zone 1 initially and subsequently lowered to zone 3 when possible.. Resuscitative median sternotomy allowed for control of the source of bleeding without requiring any other additional incisions. Thoracic vascular injuries were found in 11patients and most of them were multiple: right subclavian artery in 4, the intercostal artery in 4, the pulmonary vein in 3, the innominate vein in 2, the aortic arch in 2, the subclavian vein in 2 and the descending aorta in 1. Twelve patients required thoracic damage control surgery. All patients underwent damage control resuscitation at a ratio of 1:1:1:1 (packed red blood cells, fresh frozen plasma, platelets, and cryoprecipitate). Two patients died in the operating room and the total number of deaths was five. None of the survivors had vascular complications or neurological sequelae (Table 1 and 2).
Table 1 Baseline characteristics of patients that required REBOA + resuscitative median sternotomy
| Variable | REBOA + Resuscitative Median Sternotomy (n= 17) | |
|---|---|---|
| General characteristics | Age, median (IQR) | 32 (22 - 35) |
| Male, n (%) | 15 | |
| Mechanism of injury | Penetrating, n (%) | 15 |
| Gunshot Wounds, n (%) | 9/15 | |
| Stab Wounds, n (%) | 6/15 | |
| Blunt, n (%) | 2 | |
| Injury severity | ISS, median (IQR) | 25 (25-50) |
| AIS-Chest, median (IQR) | 5 (4-5) | |
| AIS-Abdomen, median (IQR) | 5 (5-5) | |
| AIS-Pelvic/Extremity, median (IQR) | 3 (2-4) | |
| Vital signs | SBP, mm Hg, median (IQR) | 50 (42-64) |
| HR, bpm, median (IQR) | 110 (94-132) | |
| GCS, median (IQR) | 14 (8-15) | |
| Cardiac Arrest, n (%) | 0 | |
| Transfusion requirements | PRBC, 6h, median (IQR) | 5 (4-8) |
| FFP, 6 h, median (IQR) | 6 (4-6) | |
| Platelets, 6 h, median (IQR) | 6 (0-6) | |
| Cryoprecipitate, 6 h, median (IQR) | 6 (0-10) | |
| PRBC, 24 h, median (IQR) | 7 (5-10) | |
| FFP, 24 h, median (IQR) | 8 (5-11) | |
| Platelets, 24 h, median (IQR) | 6 (0-6) | |
| Cryoprecipitate, 24 h, median (IQR) | 10 (0-14) |
AIS: Abbreviated Injury Score; FFP: Fresh Frozen Plasma; GCS: Glasgow Coma Scale; HR: Heart Rate; IQR: Interquartile Range; ISS: Injury Severity Score; PRBC: Packed Red Blood Cells; SBP: Systolic Blood Pressure.
Table 2 Clinical characteristics of patients that required REBOA + resuscitative median sternotomy
| Variable | REBOA + Resuscitative Median Sternotomy (n = 17) | |
|---|---|---|
| Arterial access | Open technique, n (%) | 14 |
| Ultrasound-Guided, n (%) | 3 | |
| Systolic blood pressure | Pre-AO, mm Hg, median (IQR) | 50 (40 - 65) |
| 5 minutes AO, mm Hg, median (IQR) | 78 (64 - 85) | |
| Post-AO, mm Hg, median (IQR) | 97 (86 - 110) | |
| REBOA placement | Zone 1, n (%) | 13 |
| Zone 1 + Zone 3, n (%) | 4 | |
| Occlusion Time, min, median (IQR) | 41 (30 - 60) | |
| Additional surgical procedures | Exploratory Laparotomy, n (%) | 4 |
| Thoracic DCS, n (%) | 12 | |
| Abdominal DCS, n (%) | 3 | |
| Mortality | Intraoperative, n (%) | 2 |
| 72 h, n (%) | 4 | |
| Intrahospital, n (%) | 5 | |
| Length of stay | ICU, days, median (IQR) | 10 (6-20) |
| Hospital, days, median (IQR) | 18 (11-25) |
AO: Aortic Occlusion; DCS: Damage Control Surgery; ICU: Intensive Care Unit; IQR: Interquartile Range.
The Trauma and Emergency Surgery Group (CTE) has proposed to include REBOA in thoracic trauma management, even in cases of vascular injuries of the thoracic outlet 8. Despite the current paradigm that REBOA is contraindicated in chest trauma management 9. We are pioneers in reporting evidence on the feasibility, effectiveness and safety of REBOA in penetrating chest trauma, supporting results from animal models 10,11. We present the following surgical approach of thoracic outlet vascular injures using REBOA and surgical strategies for definitive control of vascular injury.
Initial approach
Initial management must be directed towards the stabilization of the patient according to the Advanced Trauma Life Support (ATLS) guidelines which include the essential ABCD’s. Damage control resuscitation is initiated, followed by a chest x-ray and an extended focused assessment with sonography for trauma (E-FAST). The choice between immediate surgical exploration or further extended imaging studies depends on the hemodynamic status of the patient. If the patient is hemodynamically stable or a transient responder, computed tomography should be performed to determine the extent of the thoracic vascular injury and any other significant associated injuries. However, patients with hemodynamic instability (sustained systolic blood pressure ≤70 mmHg) and/or associated active external bleeding, massive hemothorax, cardiac tamponade and/or surgical cervical/thoracoabdominal injuries should be transferred immediately to the operating room.
Surgical management
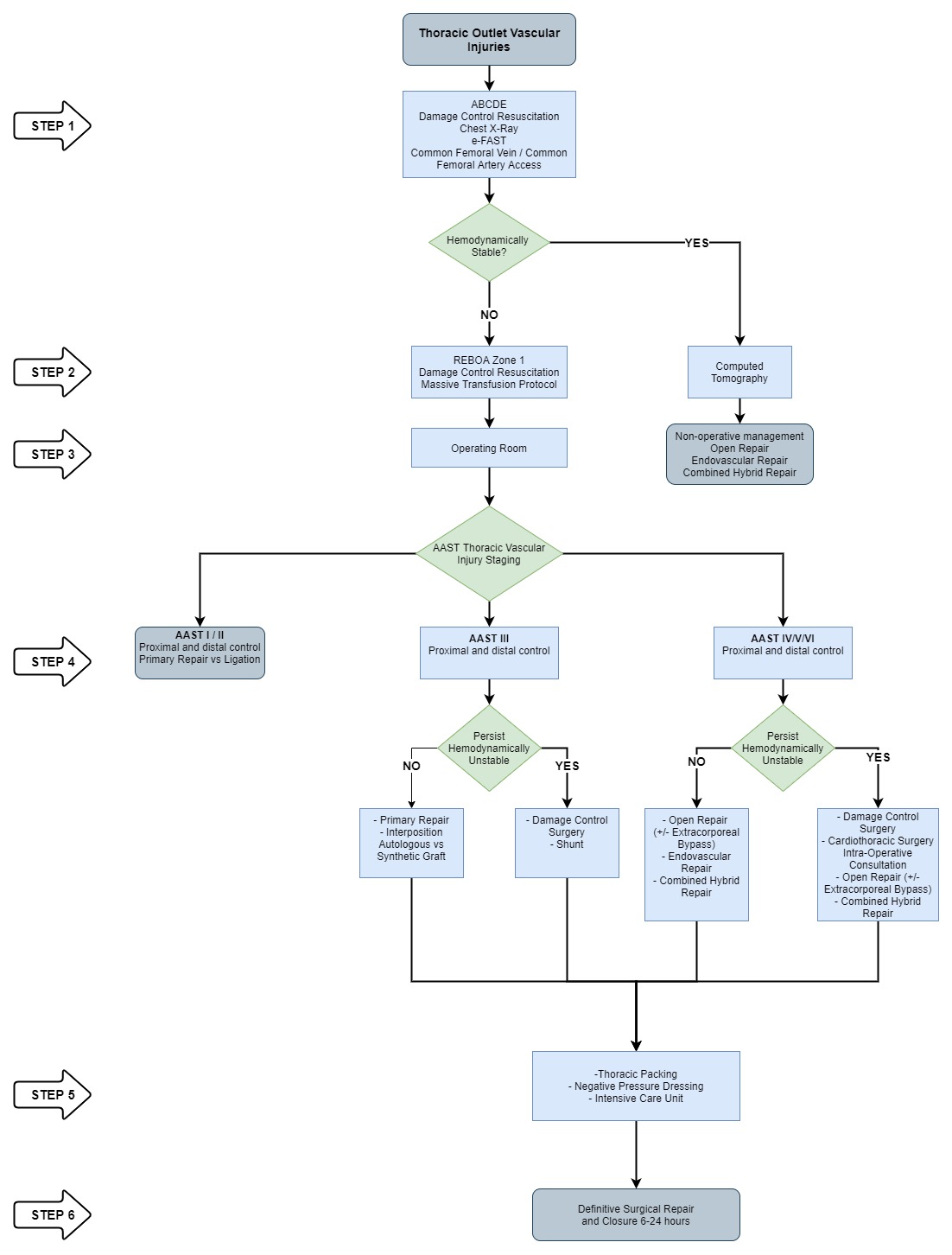
Based on our experience, we propose a new algorithm for the management of thoracic outlet vascular injuries:
● STEP 1: Attention should be directed towards identifying all immediate life-threatening injuries following the ABCDE mnemonic of ATLS (chest x-ray and E-FAST exam). Both a common femoral vein and artery lines are placed for intravenous access, blood pressure monitoring and the initiation of an aggressive damage control resuscitation.
● STEP 2: All patients with hemodynamic instability (sustained systolic blood pressure <70 mmHg) or non-transient responders should have their common femoral arterial line changed over a guidewire to a femoral sheath, followed by placement of a REBOA in Zone 1, which can be placed either in the operating or emergency room 12. The REBOA becomes an important resuscitative tool that ultimately prevents hemodynamic collapse while at the same time maintains coronary and cerebral perfusion in these hemodynamically unstable trauma patients (Figure 1). Additionally, the institution’s massive transfusion protocol should be activated. If the patient is hemodynamically stable or a transient responder, computed tomography should be performed to determine the extent of the damage and the presence of any other associated injuries. According to the findings on the computed tomography, the patient can undergo either non-operative management versus an open, endovascular and/or combined hybrid repair.
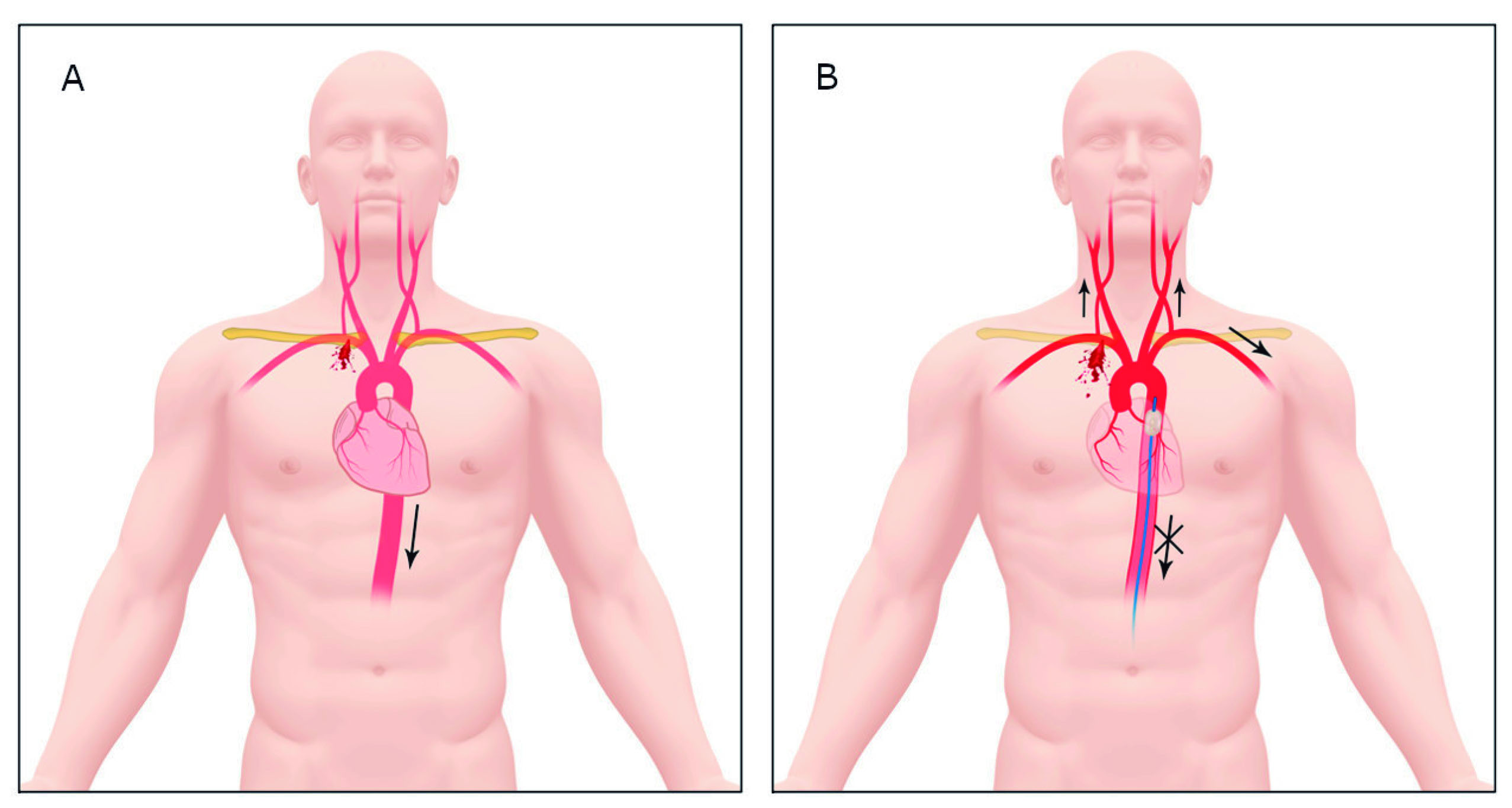
Figure 1 Blood flow redistribution following REBOA placement in Zone 1. A. Left Subclavian Artery Injury with subsequent cerebral, cardiac and systemic hypoperfusion. B. REBOA placement in Zone 1 and blood flow redistribution.
● STEP 3: The hemodynamically unstable patient or the non-transient responder should be transferred immediately to the operating room for chest exploration to obtain direct surgical control of the bleeding via a median sternotomy. Upon opening the chest, drainage of the mediastinal hematoma or massive hemothorax should follow and if cardiac tamponade is suspected, a pericardiotomy should be performed with the subsequent evacuation of the pericardial hematoma. Suppose you are not able or do not have a REBOA at your institution prior to opening the chest. In that case, we recommend aortic cross-clamping immediately by opening the left mediastinal pleura and identifying the descending thoracic aorta and positioning the vascular cross-clamp just inferior to the take-off of the left subclavian artery. As soon as this is achieved, the location and magnitude of the thoracic outlet vascular injury should be determined as soon as possible according to the AAST classification 13 (Table 3):
Table 3 AAST Classification of Thoracic Vascular Injuries
| Grade* | Description |
|---|---|
| I | Intercostal artery/vein |
| Internal mammary artery/vein | |
| Bronchial artery/vein | |
| Esophageal artery/vein | |
| Hemiazygous vein | |
| Unnamed artery/vein | |
| II | Azygos vein |
| Internal jugular vein | |
| Subclavian vein | |
| Innominate vein | |
| III | Carotid artery |
| Innominate artery | |
| Subclavian artery | |
| IV | Thoracic aorta, descending |
| Inferior vena cava (intrathoracic) | |
| Pulmonary artery, primary intraparenchymal branch | |
| Pulmonary vein, primary intraparenchymal branch | |
| V | Thoracic aorta, ascending and arch |
| Superior vena cava | |
| Pulmonary artery, main trunk | |
| Pulmonary vein, main trunk | |
| VI | Uncontained total transection of thoracic aorta or pulmonary hilum |
*Increase one grade for multiple grade III or IV injuries if more than 50% circumference; decrease one grade for grade IV injuries if less than 25% circumference.
● STEP 4:
○ AAST Grade I/II: Both proximal and distal control of the injured vessel should be obtained. These vessels can be ligated or primarily repaired with 3-0 vascular Prolene. Grade I injuries (Table 3) will require an anterolateral thoracotomy either right or left, according to the injury site. The intercostal vessels can be controlled directly via the placement of interrupted sutures that encircle the involved rib both proximally and distally. Grade II injuries will require a median sternotomy with a right or left cervical or supra-clavicular extension to gain access to the vessel. In cases of proximal subclavian vein injuries, transection of the sternocleidomastoid and/or omohyoid muscles at their clavicular insertion may be required for proximal control. The azygos vein at its insertion can be accessed via the same incision but any other portion of the vessel will require a right anterolateral thoracotomy. If these injuries cannot be repaired primarily, then suture ligation is recommended.
○ AAST Grade III: All Grade III vessel injuries will require both proximal and distal control via a median sternotomy with a right or left cervical or supra-clavicular extension. If the patient persists hemodynamically unstable, then damage control surgery principles should be implemented and a vascular shunt inserted may require cardiopulmonary bypass. Otherwise, if the patient is hemodynamically stable, primary repair of the vessel should follow when possible, and if not feasible, then an interposition graft with autologous vs. synthetic material should be performed.
Carotid Arteries: Injuries to the proximal common carotid arteries will require a median sternotomy with a cervical extension, but the mid to distal injuries will only require a corresponding cervical incision (Figure 2).
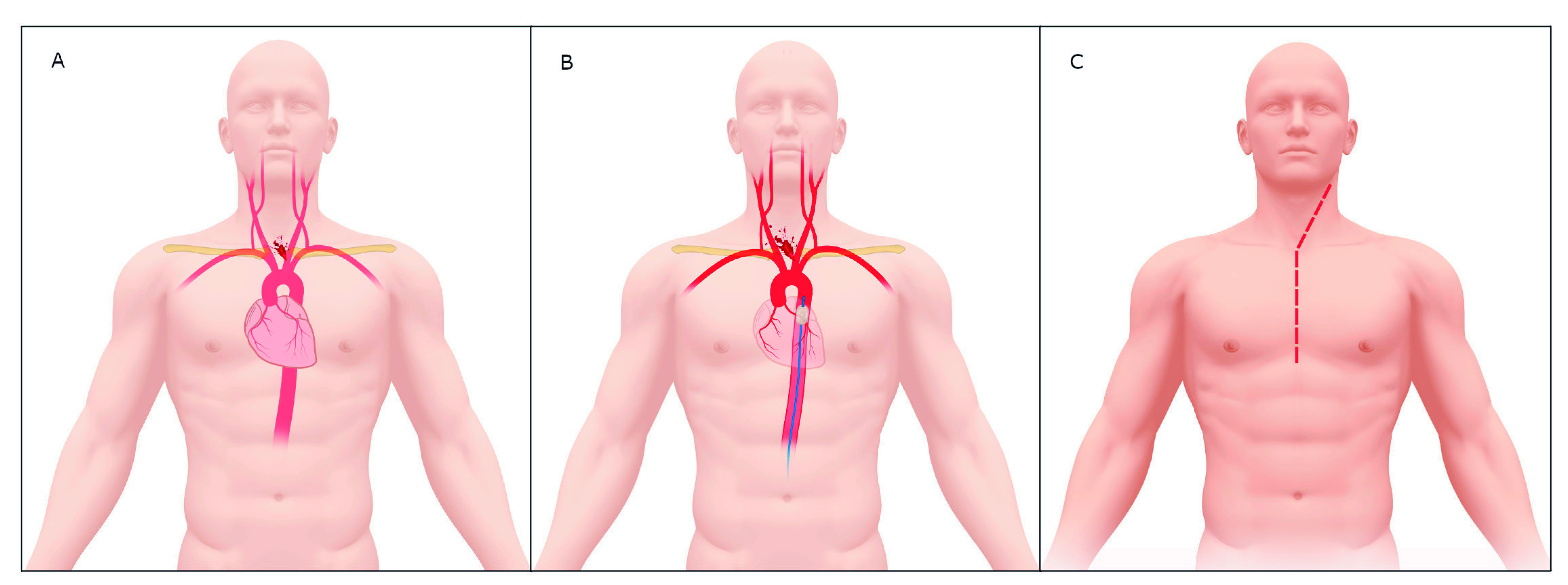
Figure 2 Left Carotid Artery Injury Management. A. Proximal Left Carotid Artery Injury. B. Proximal Left Carotid Artery Injury with REBOA in Zone 1. C. Median Sternotomy with Left Cervical Extension.
Subclavian Arteries: Subclavian vessel injuries in the post-scalenic portion should be approached via supra and infra-clavicular incisions without fracturing the clavicle and without the need of a median sternotomy. Distal control of the subclavian vessels can be achieved in these cases via the extension of the infra-clavicular incision into the adjacent deltopectoral groove (Figure 3). The left subclavian vessels will require more dissection on behalf of the surgeon to obtain both proximal and distal control as they are usually about 5 to 7 cm deep from the initial incision (Figure 4).
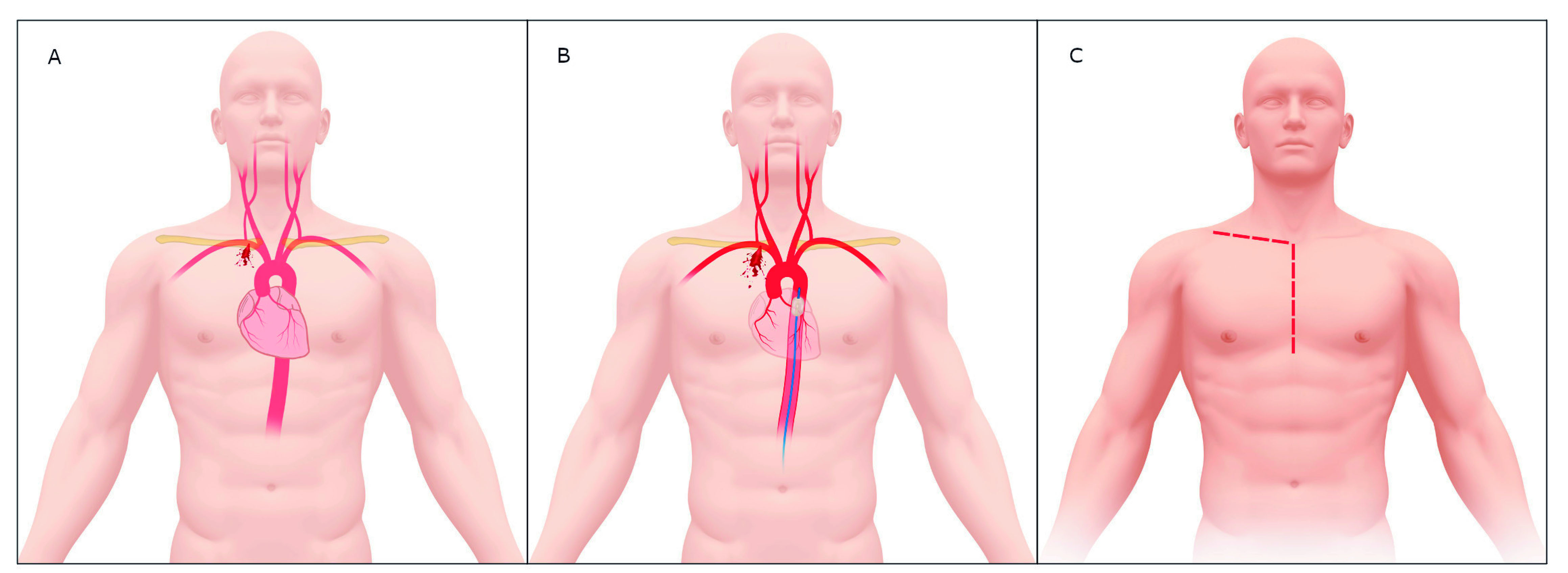
Figure 3 Proximal Right Subclavian Artery Injury Management. A. Proximal Right Subclavian Artery Injury. B. Proximal Right Subclavian Artery Injury with REBOA in Zone 1. C. Median Sternotomy with Supraclavicular Extension.
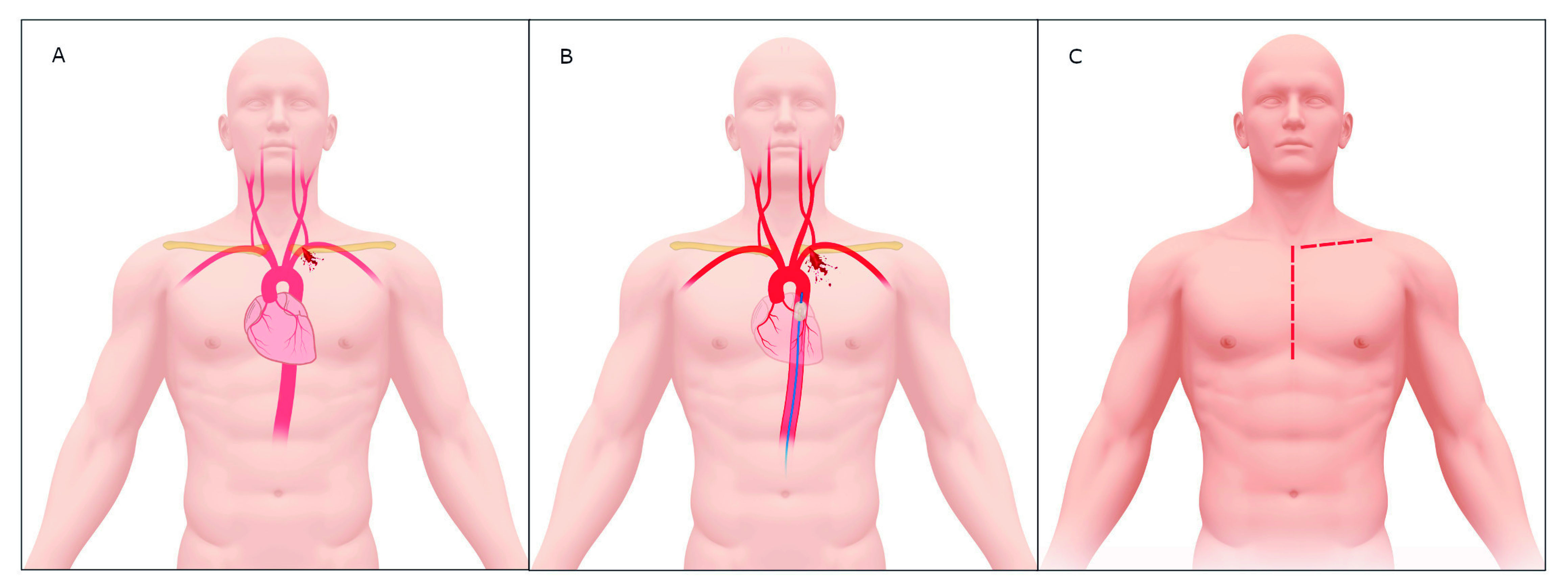
Figure 4 Proximal Left Subclavian Artery Injury Management. A. Proximal Left Subclavian Artery Injury. B. Proximal Left Subclavian Artery Injury with REBOA in Zone 1. C. Median Sternotomy with Supraclavicular Extension.
Innominate/Brachiocephalic Artery: This can also be accessed via the median sternotomy of the right cervical extension (Figure 5).
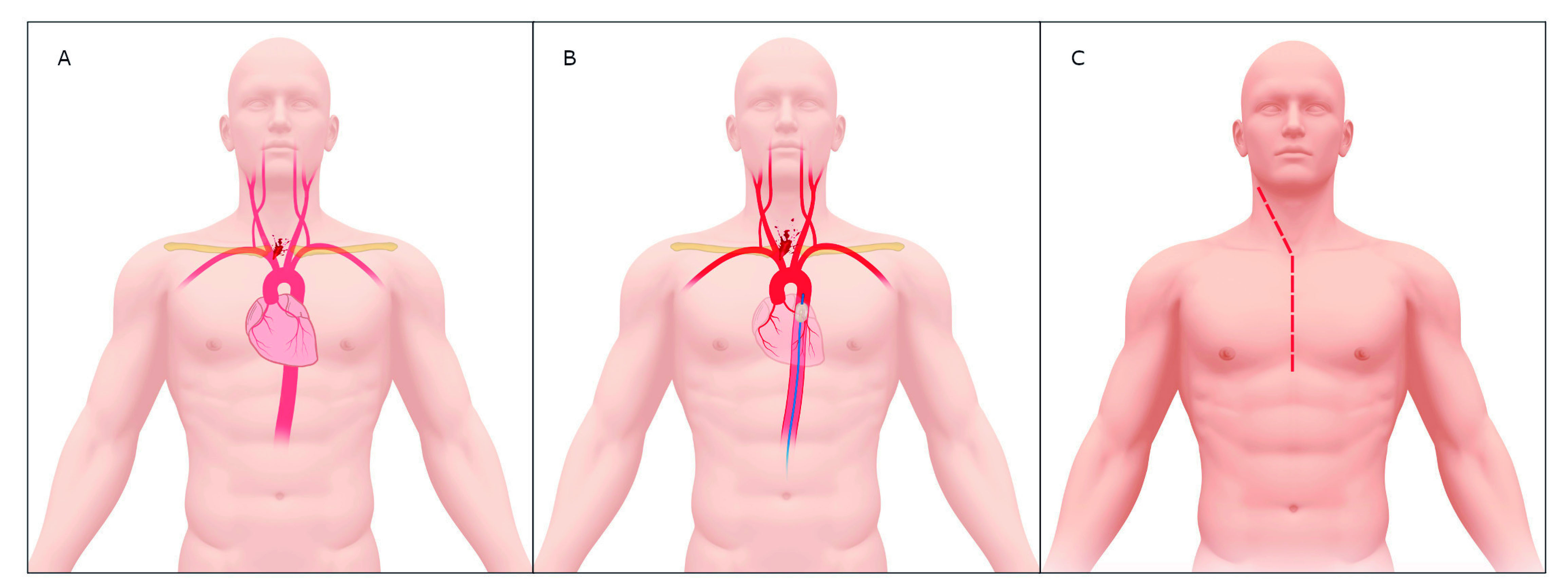
Figure 5 Innominate/Brachiocephalic Artery Injury Management. A. Innominate/Brachiocephalic Artery Injury. B. Innominate/Brachiocephalic Artery Injury with REBOA in Zone 1. C. Median Sternotomy with Right Cervical Extension
○ Grade IV/V/VI: This type of wound has a high mortality rate at the scene of the incident and the few that arrive alive to the operating room are usually from stab wounds to the upper mediastinal area, which have a common intra-operative finding of a large contained anterior mediastinal hematoma. These types of injuries require a multidisciplinary approach, including the attending trauma surgeon, a cardiovascular surgeon (since some of these patients may require extracorporeal bypass) and an interventional/vascular surgeon (when endovascular/hybrid repair is indicated). If the patient recovers hemodynamic stability, then a planned repair (open, endovascular or combined) based on imaging findings (computed tomography angiogram) should be performed. Unfortunately, most of these patients will persist hemodynamically unstable and require damage control surgery with intraoperative consultation with the cardiothoracic team (some patients will require cardiopulmonary bypass) for an open vs. combined hybrid repair.
Pulmonary Arteries: The intra-pericardial portion is ideally accessed via a median sternotomy where the left main pulmonary artery and its most proximal branches can be reached with minimal dissection. Whereas the right intra-pericardial pulmonary artery requires some dissection between the superior vena cava and the ascending aorta. Most cases can be repaired primarily with 3-0 Prolene but when not feasible, a pneumonectomy must be considered acknowledging the high mortality that this procedure entails (Figure 6).
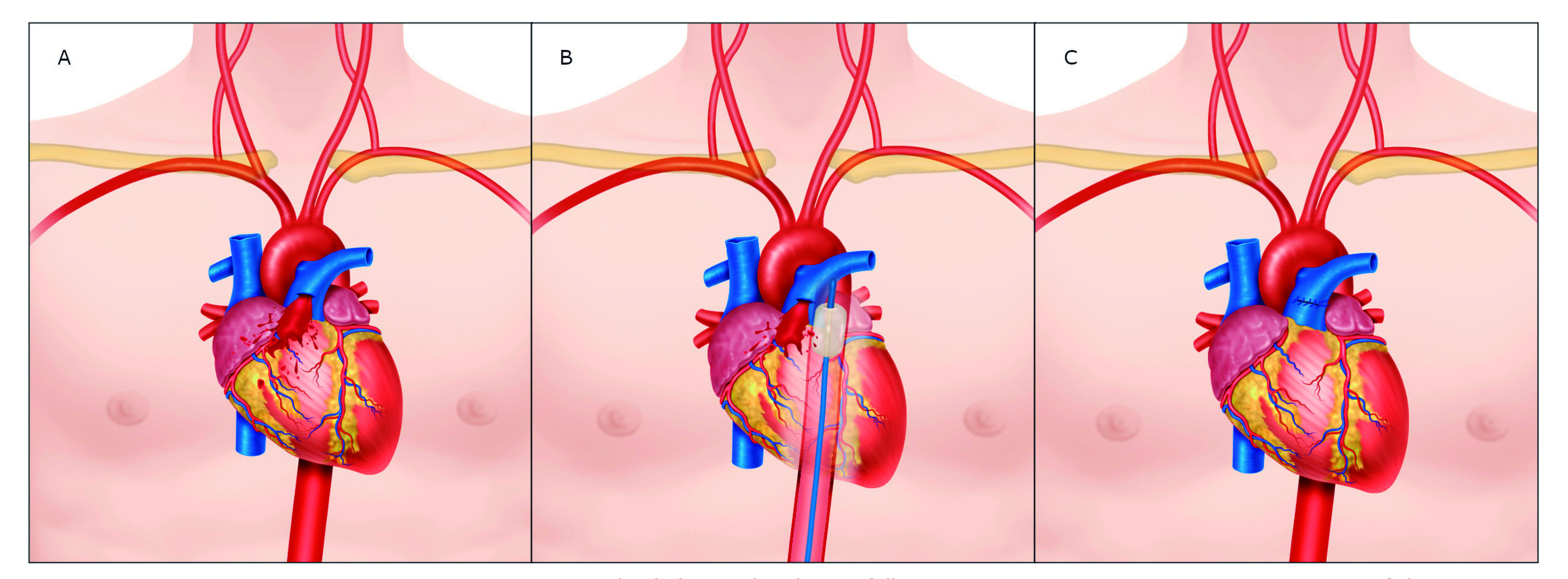
Figure 6 Proximal Pulmonary Artery Injury Management. A. Proximal Pulmonary Artery Injury. B. Proximal Pulmonary Artery Injury with REBOA in Zone 1. C. Primary Repair via Median Sternotomy
Descending Aorta: These injuries require prompt vascular control by direct digital pressure followed by the placement of two temporary 3-0 prolene parallel sutures (one on each side of the injury) which are then cross-crossed. This will permit visualization of the injury and allow for direct repair. If primary repair is considered suboptimal then placement of an endostent should be considered as reinforcement (Figure 7).
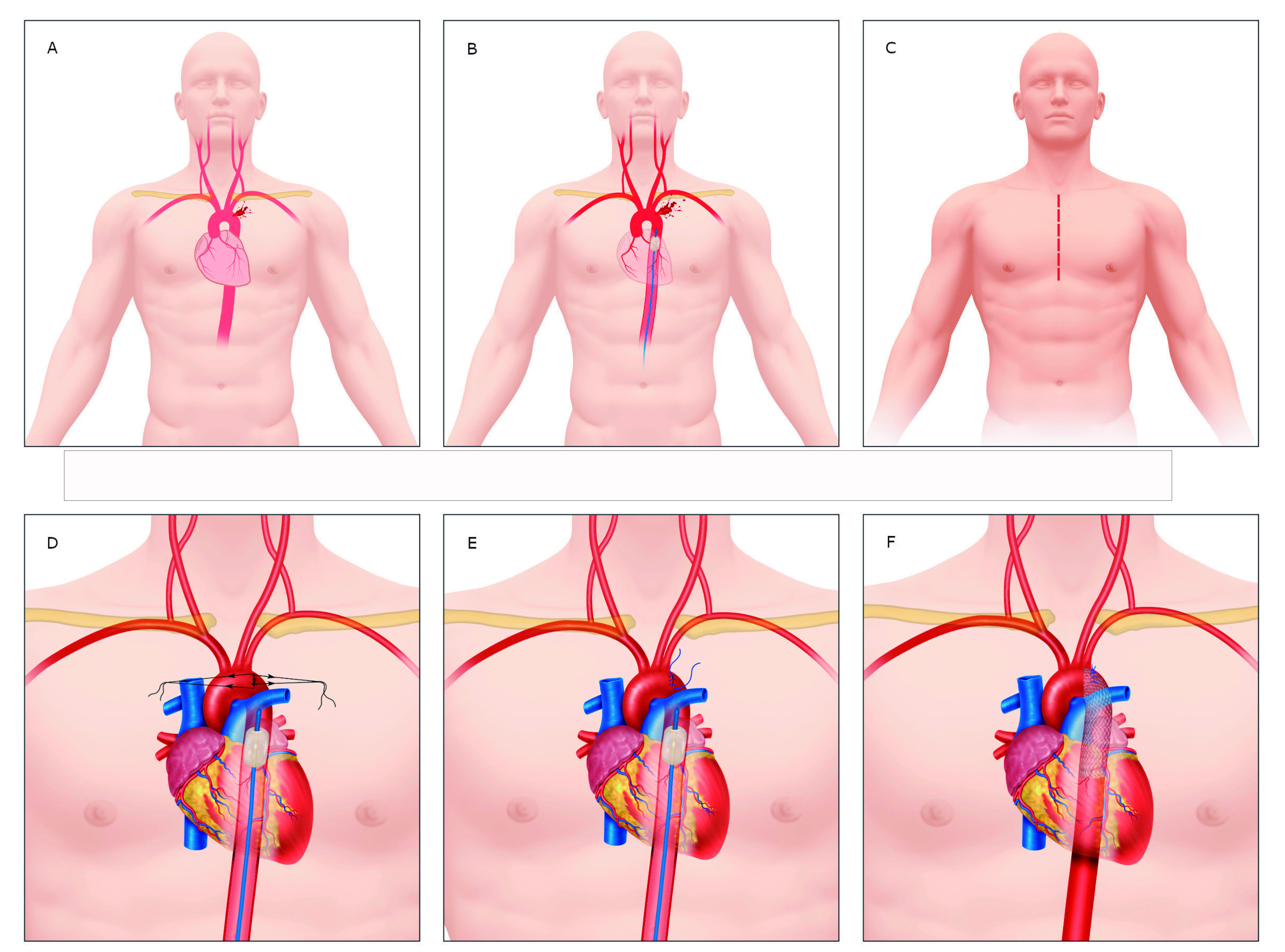
Figure 7 Descending Aortic Injury Management. A. Descending Aortic Injury. B. Descending Aortic Injury with REBOA in Zone 1. C. Median Sternotomy should be performed. D. Parallel Sutures Criss-Crossed. E. Primary Repair with REBOA in Zone 1. F. Primary Repair Plus Endostent Reinforcement.
Aortic Arch: The exposure of the injury may require ligation of the left innominate vein, remnant thymus tissue and prevention of a potential iatrogenic injury to the vagus nerve. These injuries require prompt vascular control by direct digital pressure followed by the placement of two temporary 3-0 prolene parallel sutures (one on each side of the injury), which are then cross-crossed (Figure 8).
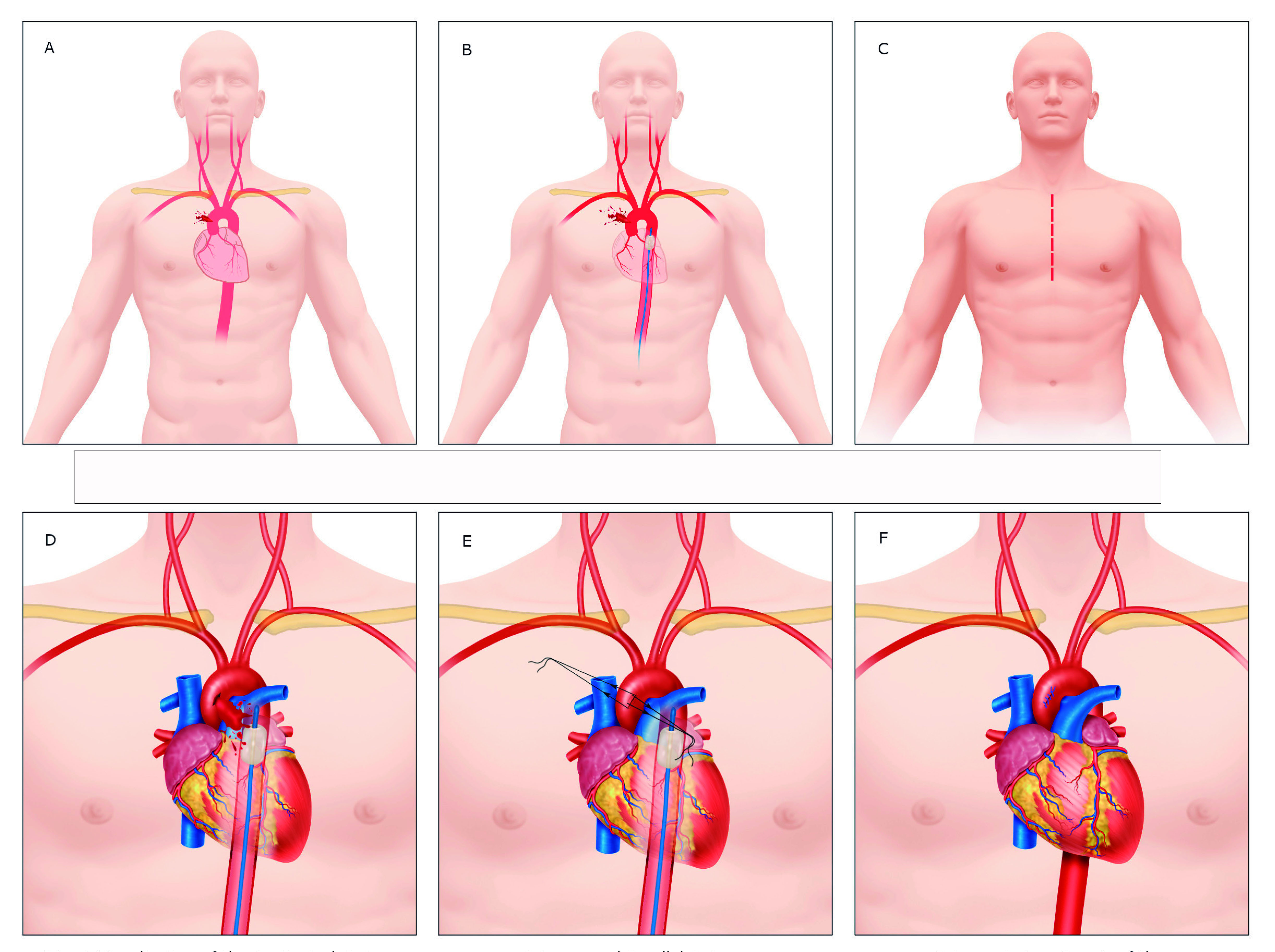
Figure 8 Aortic Arch Injury Management. A. Aortic Arch Injury. B. Aortic Arch Injury with REBOA in Zone 1. C. Median Sternotomy. D. Parallel Sutures Criss-Crossed. E. Primary Repair.
Pulmonary hilum: The exposure of the injury may require a median sternotomy and proximal control may be readily achieved with a Satinsky vascular clamp and ultimately require ligation of the hilum (Figure 9).
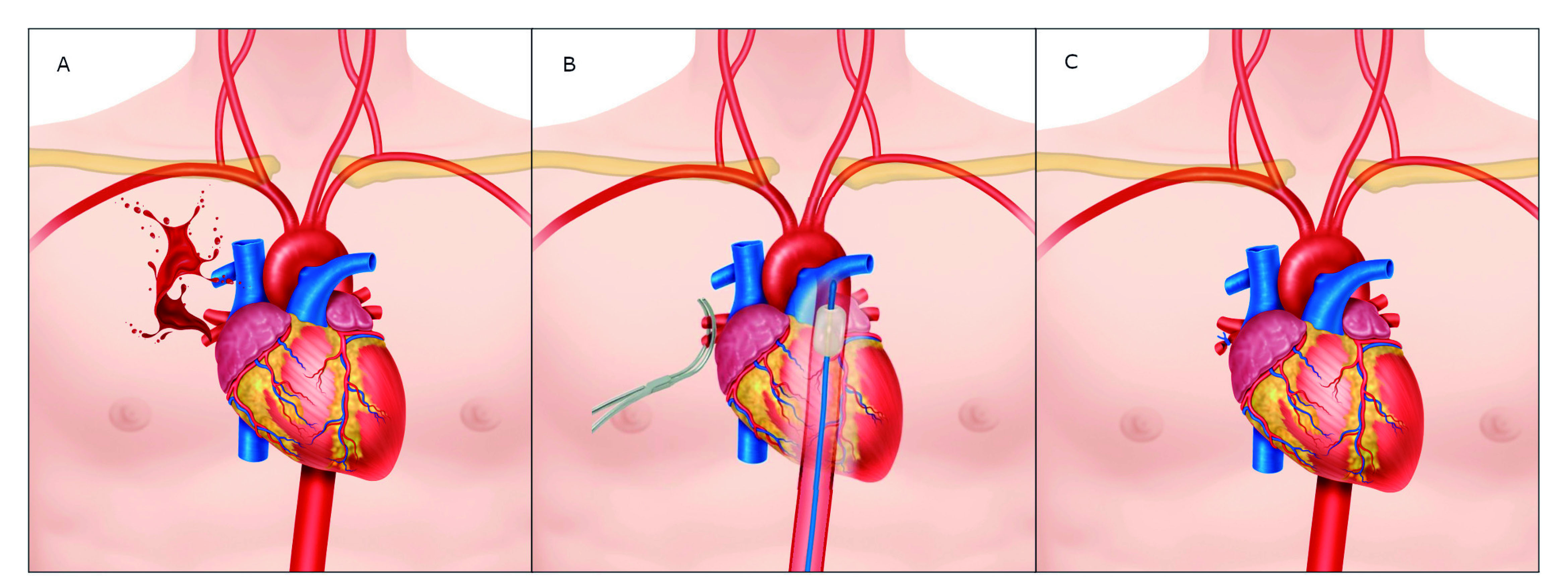
Figure 9 Pulmonary Hilum Injury Management. A. Pulmonary Hilum Injury. B. Control with Satinsky Clamp and REBOA in Zone 1. C. Pulmonary Hilum Ligation
● STEP 5: Once bleeding is controlled and temporary or permanent repair has been achieved, then the mediastinum should be packed and a negative dressing pressure should be applied, leaving the median sternotomy open. The patient should then be transferred to the intensive care unit for correction of the lethal diamond.
● STEP 6: Between 6 (especially in patients who required damage control surgery with a temporary shunt placement) and 24 hours post-initial damage control surgery procedure, the patient should be taken back to the operative room for definitive reconstruction mediastinal washout and sternal closure.
We have developed an easy to follow six-step management algorithm that clearly illustrates the surgical care of patients with thoracic outlet vascular injuries according to the AAST classification (Figure 10).
Discussion
A 23-year review study on the experience obtained from a total of 950 patients who underwent a resuscitative thoracotomy revealed an overall survival rate of 4% 14. Similarly, Rhee et al. conducted a multicenter study that included 4620 patients who also underwent a resuscitative thoracotomy and determined that the factors involved with successful clinical outcomes were: mechanism of injury, injury location and presence of vital signs upon arrival. They further concluded that patients who arrive with vital signs to the emergency room had a survival rate of 12%, while in the absence of vital signs upon arrival, the survival was only 1.2% 15. Although, a recent systematic review found that the overall survival rate increased to up to 21% for those arriving with vital signs 16. Furthermore, we have achieved an overall survival of 71% by combining the use of a median sternotomy with a REBOA in Zone 1 as a viable surgical substitute to the traditional resuscitative thoracotomy. We believe that this improvement in survival noted in our study is multifactorial and includes the fact that both procedures were performed soon after arrival and before any episode of cardiac arrest by two separate and simultaneous surgical teams without incurring any delay 8. This is the reason why endovascular or open aortic cross-clamping should be implemented in the initial management of hemodynamically unstable severely injured trauma patients 8.
Parra-Sanchez has built upon using a median sternotomy in hemodynamically unstable thoracic trauma patients by adding the prehospital concept of “scoop and run” to reassure an alive patient upon arrival to the hospital 17. Furthermore, O’Connor and Scalea reported a series of 36 patients with penetrating chest trauma with associated injuries of the great vessels in which 75% of the patients arrived hemodynamically unstable and were managed via a median sternotomy. All of these authors have recognized that a median sternotomy allows for prompt and appropriate access to the great vessels, the heart, bilateral pleural spaces and pulmonary hilum 18. On the other hand, the median sternotomy also has its own limitations, including the availability of equipment to perform the procedure and the expertise required by the treating surgeon. That is why over the years, the concept of an anterolateral thoracotomy has gained traction over that of a median sternotomy among surgeons because of its ease and minimal equipment required. However, it has its inherent risks, including the high risk of injury and/or blood contamination of the surgeon and the ancillary staff . For all these reasons, we recommend that a median sternotomy should be performed in most cases of thoracic outlet vascular injuries.
Conclusion
The early application of a resuscitative median sternotomy and a Zone 1 REBOA in hemodynamically unstable trauma patients with thoracic outlet vascular injuries improves survival by providing rapid stabilization of the central aortic pressure and serving as a bridge to hemorrhage control.











 text in
text in