Remark
| 1) Why was this study conducted? |
| This study was carried out to test the effect of an aquatic exercise routine on the stability of the elderly by two different methods: stabilometry and electromyography. |
| 2) What were the most relevant results of the study? |
| Both methods revealed immediate improvements in the postural stability of the elderly after the application of the routine aquatic protocol. |
| 3) What do these results contribute? |
| In the decision-making of physiatrists, physiotherapists and other related health personnel when prescribing therapies in the elderly population. They can give priority to those activities that involve aquatic exercises when it is necessary to improve the postural stability of this population in the rehabilitation processes. |
Introduction
As a result of better treatments to cure diseases and multiple other reasons, most people’s life expectancy has been extended to 60 years or more. The number of seniors will almost double in the coming years 1, and they will suffer from conditions such as balance disorders, which lead to musculoskeletal disorders (MSDs) and are generally degenerative. This situation poses serious problems for public health and the overall quality of life (2,3 because such medical conditions significantly increase the cost of rehabilitation processes if they are not timely prevented or treated 4.
Water exercises have proven to be effective and efficient to restore body functions in the short term 5,6 because the movements are slower and more predictable than on the ground, providing more significant sensory-motor feedback, balance, stability, and coordination, and facilitating postures such as a standing position 7. Nevertheless, few studies so far have examined the influence of water on postural stability, and most of them are anecdotal or biased due to a lack of standardized protocols to evaluate its impact on rehabilitation 8.
This study evaluates the postural stability of elderly individuals based on their muscle coactivation and baropodometric variables to assess the immediate and final effects of implementing a water exercise protocol.
In this study, two techniques were employed to assess postural stability. First, muscle coactivation (i.e., the simultaneous contraction of agonist and antagonist muscles) was measured using electromyography 9, and its role in maintaining articular stability was demonstrated 10. Second, a baropodometric platform was used to measure the area of stabilometric ellipse, mean plantar pressure, and weight distribution percentage on the footprint 11; therefore, it was proven that the second technique can be used for quantifying postural control 12,13.
Materials and Methods
Type of study
This was a prospective cohort pilot study conducted with a single group of elderly individuals. Participants were recruited from INDER Medellín, an active senior group. The protocol was followed in 12 one-hour sessions over four weeks, and it was finished when the subject abandoned or finished the study.
Population
None of the participants had been diagnosed with joint disorders in lower limbs such as arthrosis or arthritis, disc wounds with radiating pain to lower limbs from L3-S1, neuropathies, neurological disorders (ataxia or multiple sclerosis), cerebellar problems, epilepsy, vertigo, diabetes, peripheral venous insufficiency, severe kidney disease, urinary and/or anal incontinence, open wounds, or amputation of lower limbs. The subjects had to attend the twelve sessions to be included in this study even after being selected. Before their voluntary participation, they signed an informed consent approved by the Ethics Committee of Instituto Tecnológico Metropolitano, which observes the principles established in the Declaration of Helsinki (DoH), as recommended by the World Medical Association 14.
Exercise protocol
This exercise protocol was followed in a 1.63-meter-deep sports pool at Instituto Tecnológico Metropolitano. The water exercise routine for lower limbs was focused on postural stability and divided into 12 one-hour sessions over four weeks. In each of the four weeks, participants performed different exercises (at least fifteen repetitions after the respective warm-up exercises), as follows: (i) stretching to work on their joint mobility and flexibility; (ii) eccentric joint movements with bipedal standing to improve strength and proprioception; (iii) seated marching workout and stairs with unipedal standing to work on balance and proprioception; and (iv) exercises to identify the joint position (eyes open/closed) with unipedal and bipedal standing for coordination, speed, and functionality.
Signal acquisition
Surface electromyography was used to capture muscle coactivation signals, and a baropodometric platform recorded their plantar pressures. The signals were obtained while the participants were standing on both feet on the platform for 6 seconds before and after the water exercise protocol to calculate all the measurements and obtain 24 signals per subject.
Stability measured by muscle coactivation
The muscle coactivation percentage of the subjects’ self-reported dominant leg was calculated by means of surface electromyography (EMG) of the six muscle groups that are directly involved in the stability of lower limbs: tibialis anterior (TA), soleus (S), gastrocnemius medialis (GM), gastrocnemius lateralis (GL), vastus medialis (VM), and biceps femoris (FB) 15 (Figure 1A ).
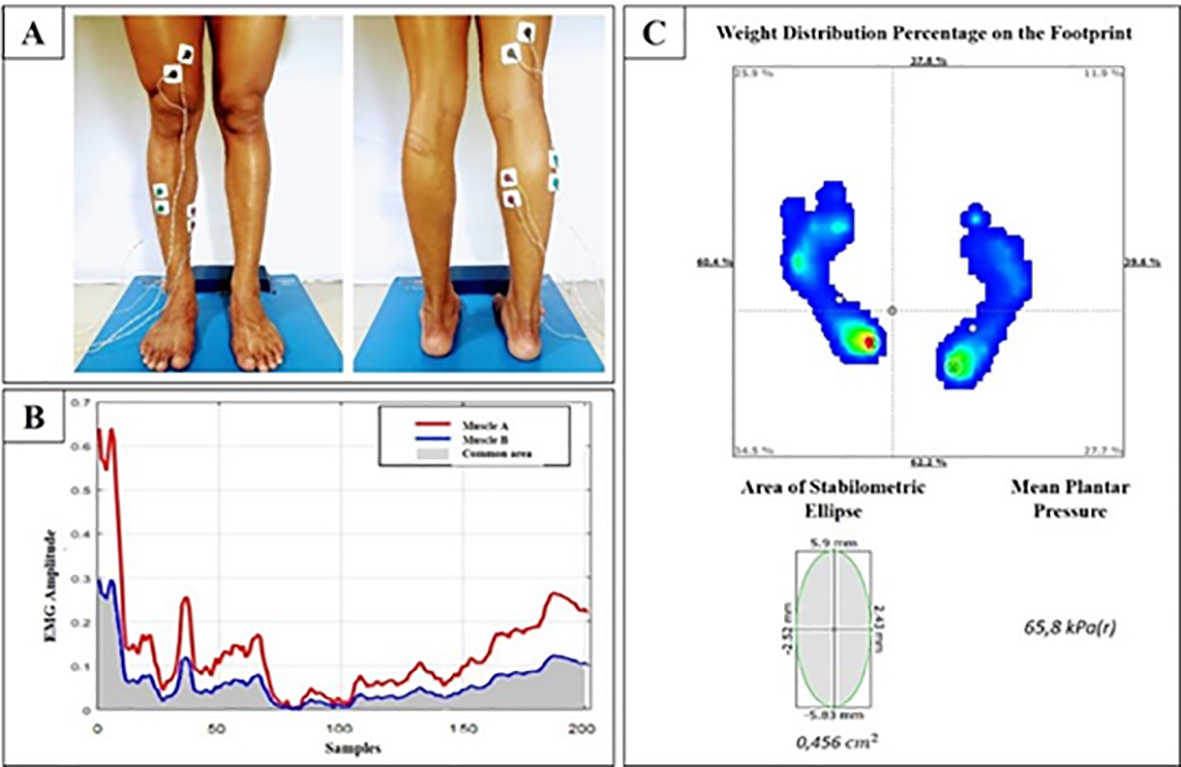
Figure 1 (A) Placement of the electrodes: front (TA, S, and FB muscles) and back (GM, GL, and VM muscles). (B) Area of the muscle coactivation percentage. (C) Baropodometric variables (weight distribution, area of the stabilometric ellipse, and mean plantar pressure).
The protocol of the SENIAM (Surface Electromyography for the Non-Invasive Assessment of Muscles) project was applied to place the electrodes 16. The signals were acquired with an ML138 differential amplifier connected to a PowerLab 16/35 polygraph manufactured by AD Instruments Inc. A 2-kHz sampling frequency was used, and the signal was preprocessed with LabChart Pro software implementing a 60-Hz notch filter and another passband with a cutoff frequency between 10 and 500 Hz.
Matlab was employed to calculate the coactivation percentage. The signals obtained from the muscles were filtered once again using a fifth-order digital Butterworth bandpass filter with cutoff frequencies between 10 and 300 Hz. The root mean square (RMS) of each resulting signal was calculated with a window of 250 samples and an overlapping of 50 samples. Finally, four muscle groups (VM/BF, T/S, T/GM, and T/GL) were created to be normalized using the following equation:
Where 𝑋𝑛 denotes the normalized signal; 𝑋, the original signal; and 𝑋𝑚𝑖𝑛 and 𝑋𝑚𝑎𝑥, the minimum and maximum values of the original signal, respectively. Afterward, the coactivation percentage between muscles was calculated using Equation 2 17.
where % COACT is the coactivation percentage between the agonist and antagonist muscles; A area, the area under the curve of the processed EMG signal of the A muscle; 𝐵 𝑎𝑟𝑒𝑎, the area under the curve of the processed EMG signal of the B muscle; and A & B common area, the region of activity shared by the A and B muscles (Figure 1B) 17. Note that, when this percentage approaches 100%, stability is low; and, when it tends to 0%, stability is high 18,19.
Stability measured by baropodometry
The pressure platform Ecowalk and its software EcoFoot 4.0 calculated the baropodometric variables in this study. Such measurement system comprises a 67-cm-long, 54-cm-wide portable platform equipped with 2,300 capacitive sensors. After the participants stood on the platform and maintained their standard anatomical position for 6 seconds, the following data were collected: area of stabilometric ellipse, mean plantar pressure, and weight distribution percentage (Figure 1C). Said distribution was calculated as the difference between the anterior and posterior distribution of weight; likewise, the lateral distribution resulted from subtracting 50% from the lateral distribution of the dominant foot because only one foot was measured. The variables mentioned above describe the stability of each participant 11,20.
Characterization of the captured data
The immediate and long-term effects of this exercise protocol were analyzed. The former were studied by comparing each variable before and after the exercise sessions; and the latter were established by comparing the measurements before the first routine and after the twelfth session. Additionally, the sessions that had a significant influence on the measured variables were examined in detail.
The data were statistically analyzed using SPSS software (version 24). The Kolmogorov- Smirnov test for normality was employed with a significance level of 0.05. Some of the data presented normality, however, a non-parametric test, Wilcoxon signed rank test were applied to all the variables to determine significant differences between the groups of variables mentioned above for each exercise protocol effect.
Results
Snowball sampling, a non-probability technique, was implemented to select, among 42 adults, only 20 participants. As a result, the sample was composed of 17 women and 3 men aged 62.5 ± 9.2. Their data were collected between August and December 2018 to measure the effectiveness of the aquatic exercise protocol in improving postural stability. Six participants abandoned the study after the ninth session for personal reasons or due to incompatibilities in their schedules. No accidents were reported during the implementation of the protocol. The immediate effects of the exercise protocol were analyzed by comparing each one of the measurements before and after every exercise session. In the final effect, the first session before performing the protocol was compared with the twelfth session after performing the exercises.
Immediate effect
Regarding stability by coactivation, only the values of T/GM exhibited a significant difference. The coactivation of the tibialis anterior decreased compared to that of the gastrocnemii (T/GM and T/GL), while the coactivation of VM/BF and T/S increased slightly; hence, only two of the four muscle pairs presented reduced coactivation (Table 1).
Table 1 Immediate effect of the exercise protocol.
| Variables | Measurement | Mean ± SD | Median | Kolmogorov-Smirnov Test | Wilcoxon signed rank test | ||
|---|---|---|---|---|---|---|---|
| P-value | Significance Level | Significant difference | |||||
| Muscle Coactivation | Vastus Medialis vs Biceps Femoris (%) | Before | 42.28 ± 23.12 | 42.95 | 0.004 | 614.0 | No |
| After | 42.68 ± 21.43 | 43.57 | 0.200 | ||||
| Tibialis anterior vs Soleus (%) | Before | 43.25 ± 22.78 | 42.28 | 0.005 | 510.0 | No | |
| After | 41.29 ± 24.46 | 42.95 | 0.002 | ||||
| Tibialis anterior vs Gastrocnemius Medialis (%) | Before | 44.07 ± 22.62 | 43.65 | 0.002 | 33.0 | Yes | |
| After | 39.29 ± 22.13 | 40.64 | 0.007 | ||||
| Tibialis anterior vs Gastrocnemius Lateralis (%) | Before | 44.19 ± 24.45 | 47.35 | 0.000 | 224.0 | No | |
| After | 41.39 ± 24.89 | 41.30 | 0.003 | ||||
| Stabilometry | Anteroposterior weight distribution (%) | Before | 27.15 ± 17.18 | 24.20 | 0.007 | 128.0 | No |
| After | 29.16 ± 17.31 | 27.60 | 0.044 | ||||
| Lateral weight distribution (%) | Before | 20.37 ± 13.83 | 18.10 | 0.001 | 218.0 | No | |
| After | 22.06 ± 15.23 | 19.90 | 0.000 | ||||
| Area of ellipse (cm2) | Before | 14.16 ± 27.40 | 3.99 | 0.000 | 21.0 | Yes | |
| After | 16.52 ± 22.79 | 8.40 | 0.000 | ||||
| Mean pressure (kPa) | Before | 22.71±12,07 | 19.25 | 0.000 | 12.0 | Yes | |
| After | 21.26±11.74 | 19.00 | 0.000 | ||||
When postural stability was determined by means of baropodometry, only the ellipse area and mean pressure exhibited significant differences, the latter being the only one that did not show an increase after the protocol was applied (Table 1). Additionally, more body weight was distributed on the right foot in 54% of the population, and on the hindfoot in 86% of them.
Final effect
The stability by coactivation of the VM/BF muscle pair was the only variable that decreased in the long term, although it showed no significant difference after the entire exercise protocol (Table 2).
Table 2 Final effect of the exercise protocol.
| Variables | Measurement | Mean ± SD | Median | Kolmogorov-Smirnov Test | Wilcoxon signed rank test | ||
|---|---|---|---|---|---|---|---|
| P-value | Significance Level | Significant difference | |||||
| Muscle Coactivation | Vastus Medialis vs Biceps Femoris (%) | Before | 43.84 ± 22.99 | 42.96 | 0.200 | 925.0 | No |
| After | 40.89 ± 20.05 | 34.13 | 0.123 | ||||
| Tibialis anterior vs Soleus (%) | Before | 44.89 ± 21.12 | 37.13 | 0.042 | 221.0 | No | |
| After | 35.14 ± 24.44 | 40.40 | 0.200 | ||||
| Tibialis anterior vs Gastrocnemius Medialis (%) | Before | 33.55 ± 19.34 | 30.71 | 0.156 | 433.0 | No | |
| After | 42.28 ± 22.39 | 36.11 | 0.052 | ||||
| Tibialis anterior vs Gastrocnemius Lateralis (%) | Before | 41.79 ± 29.03 | 41.71 | 0.015 | 975.0 | No | |
| After | 39.92 ± 25.36 | 41.10 | 0.200 | ||||
| Stabilometry | Anteroposterior weight distribution (%) | Before | 33.13 ± 20.24 | 24.3 | 0.030 | 221.0 | No |
| After | 25.94 ± 15.28 | 23.9 | 0.200 | ||||
| Lateral weight distribution [%] | Before | 27.53 ± 17.31 | 19.7 | 0.034 | 158.0 | No | |
| After | 19.60 ± 16.07 | 14.40 | 0.145 | ||||
| Area of ellipse (cm2) | Before | 3.60 ± 6.70 | 1.02 | 0.001 | 8.0 | Yes | |
| After | 19.18 ± 22.68 | 8.93 | 0.054 | ||||
| Mean pressure (kPa) | Before | 28.64 ± 7.37 | 19.85 | 0.200 | 221.0 | No | |
| After | 16.34 ± 9.47 | 12.90 | 0.138 | ||||
As in the case of the immediate effect measured by baropodometry, the area of the ellipse presented a significant difference. Nevertheless, the mean pressure did not, which was reflected in a decrease in all the variables, except for the area of the stabilometric ellipse (Table 2). Additionally, more body weight was distributed on the right foot in 57% of the population, and on the hindfoot in 79% of them.
Discussion
The slightly lower coactivation of most of the calf muscles that was found in this study may indicate an immediate improvement of the postural stability of the elderly after the water exercise protocol was applied. Such muscles are directly involved in the stability of lower limbs because they are located close to the ankle joint 21, closer than the VM/BF muscle pair in the thigh, which has no direct influence on the postural stability of lower limbs. Additionally, studies suggest that the coactivation of the T/S muscles decreases mainly after an exercise routine on the floor 22; therefore, water may produce changes in the activation of said group.
Nevertheless, there is no consensus in the field to compare the results of aquatic exercises with those of traditional balance therapy. Some evidence in related works shows there is no statistically significant difference between conventional therapy and hydrotherapy; therefore, regardless of the environment where therapy is performed, an improvement in postural stability can be achieved 23. Even using other measuring instruments (e.g., Berg Balance scale and the Timed Up and Go test), perceived stability has been reported to be lower when the task is performed in the water compared to on the ground 24,25.
The results of this study show an immediate increase in lateral and anteroposterior weight distribution, but a slight decrease in mean plantar pressure. This outcome may have expanded the area of the stabilometric ellipse, which is the variable most closely related to postural stability 26.
The final coactivation of the VM/BF muscle pair was reduced, which suggests a general improvement in postural stability. This decrease in coactivation only in the thigh muscles and not the calf could indicate that the final proprioception exercises in the protocol focus more on that area.
It has been shown that stabilometric parameters measured using pressure platforms provide valid information about postural stability 27. All the baropodometric variables in this study exhibited lower values in the long term, except for the stabilometric ellipse area, which is possibly due to the fact that a standard position was not established for participants to place their feet on the pressure platform and their base of support could affect said variable 28.
This study has two limitations: (a) the pool water temperature and the feet posture on the pressure platform were not standardized and (b) there was no control group. As a result, future work should consider factors such as water temperature (typical hydrotherapy pools are between 33.5° and 35.5° C) because this aspect determines the behavior of seniors’ bodies, as the heat transfer starts immediately after the initial immersion, affecting muscular behavior 29. Furthermore, the support base should be measured or normalized as an additional variable related to stability 30.
Conclusion
After the 12-session protocol was completed, the baropodometry and muscle coactivation showed improvements, which indicates that the water exercises considered in this work may have positive effects on postural stability. This protocol can be part of an optimal intervention strategy to prevent falls because it involves training to improve the strength and balance of patients with osteoarthritis, as claimed by Martínez-Amat et al. 31.











 text in
text in 



