Remark
| 1. What is the reason for this study? |
| There is no validated study for assessing sexual function in women with pelvic floor dysfunctions in Chile. |
| 2. What are the most important results of the study? |
| Psychometric analysis supported a three-factor structure: sexual response, female sexual problems, and male sexual problems, with a good, acceptable, and poor reliability, respectively. |
| 3. What do these results provide? |
| To make available a valid and reliable tool (Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12) for measuring the sexual dimension and problems in Chilean women with pelvic floor dysfunctions. |
Introduction
Pelvic floor dysfunctions (PFDs) affect one third of adult women1. International statistics show that 25-50% of women will suffer a pelvic floor dysfunction in their lives2. Although these pathologies are not lethal, their symptoms can alter daily life, including physical, social, and sexual functioning 3. Sexual function is an important quality of life indicator and is influenced by several physical, psychological, and social factors 2-4.
It has been proved that the more symptoms of a pelvic floor dysfunction a woman shows, the more problems she will have in her sexual response 5; therefore, gynecological care should include an analysis of sexual function that covers both the woman’s and her partner’s characteristics 6.
The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-31), created by Rogers et al., assesses the sexual function of women with pelvic floor dysfunctions 7, and was initially designed as a specific, reliable, valid, self-administered tool for sexually active women with pelvic organ prolapse (POP), urinary (UI), or fecal incontinence (FI). Items in this tool were developed by asking experts in sexual functioning and considering previously validated tools that had evaluated sexual functioning in general population. The tools used as standardization criteria when creating PISQ-31 were the Incontinence Impact Questionnaire (IIQ-7), which assesses the impact of incontinence on the user's social functioning; the Sexual History Form-12 (SHF-12), a non-specific questionnaire that evaluates sexual functioning, and other scales for assessing depression, somatization, anxiety, and hostility 7,8. The 31 questions evaluate three domains (behavioral/emotional, physical, and partner-related factors) by answering a Likert-type scale (0= always, and 4= never) - except for Question 5, whose score goes from 0 to 5 (0= no masturbation, and 5= always). Assessment comes from adding up the score for each question, and so, higher scores reflect a better sexual functioning 7.
Later, the same author and her team reduced the original questionnaire to 12 items (PISQ-12) 9, with a validated translation to Spanish in 2008 by Espuña et al 8. This questionnaire focuses in heterosexual women, sexually active and with a sexual partner, who suffer from genital prolapse and/or urinary incontinence 8), and covers three domains: sexual response (items 1-4, 12), female sexual problems (items 5-9), and male sexual problems (items 10-11) 8. Scores follow a Likert-type scale, where 0 is always and 4 is never, with this reversed for items assessing behaviors and emotions during sexual response (items 1-4), and then all scores are added up. The final score goes from 0 to 48, and the highest the score, the better sexual function, with answering 0 or 1 to any question being regarded as a faulty sexual response - that is, a female sexual dysfunction 2.
The psychometric analysis needed to assess the validity and reliability of PISQ-12 has yet to be done in Latin America and the Caribbean. Therefore, we propose to assess its psychometric properties for use in pelvic floor dysfunction patients of a hospital in the south of Chile.
Materials and method
Cross-sectional study of psychometrics in women getting treated by the Pelvic Floor Unit of a tertiary hospital in the south of Chile (June 2014 - May 2015). Inclusion criteria: be an 18 years old or older woman, with sexual activity in the last six months, suffer from UI or POP, and be a patient of the unit. Non-probability, convenience sampling.
Socio-demographic (age, marital status, education, employment) and health (weight and height, number of pregnancies, types of birth, history of urine leakage, POP stage, urinary infection) variables, being quantitative and qualitative variables, were included in the study. Variables covering the sexual function of women with pelvic floor dysfunction were assessed with PISQ-12, assessing the domains of emotional behavior, physical aspects, and partner-related factors. Recruiting was done by the unit’s healthcare team (medical specialists and midwives). Women were scheduled for a 45-minute semi-structured interview, made to coincide with their medical appointment, in a private room prepared for such purpose.
Univariate analysis of the quantitative (mean, standard deviation, minimum and maximum) and qualitative (absolute and percentage frequency) variables was done. In order to conduct the psychometric tests, items 1, 2, 3, and 4 of PISQ-12 had to be recodified by reversing their values, just as suggested by Rogers et al. 7 and Espuña et al. 8
Content validity was checked by experts with an ad hoc guideline, evaluating semantic equivalence, cultural congruence with Chilean population, and the relevance of its content, with 4 indicators in a Likert-type scale (from strongly agree to strongly disagree). Coincidence percentage and items with minimum and maximum scores were analyzed (Table 1).
Construct validity was assessed with a confirmatory factor analysis (CFA), evaluating the adjustment of its theoretical proposal to data. Due to the scale of the questionnaire, consisting of five alternatives, the weighted least square mean and variance adjusted (WLSMV) estimator was chosen for its evaluation, as it gives more precise estimates for ordinal data 10. To estimate the fit, the indexes used were the comparative fit index (CFI); the Tucker-Lewis index (TLI); the root mean square error of approximation (RMSEA), with a 90% confidence interval, and the standardized root mean-square residual (SRMR). For cut-off scores, CFI and TLI over 0.90 were considered acceptable, and good if over 0.95. In the case of RMSEA and SRMR, values under 0.06 were considered adequate 11-13.
The internal consistency of the identified factors was evaluated with Cronbach’s alpha, taking a value >0.7 as acceptable. Pearson correlation coefficient between each item and the corrected total was used to check the discriminating capacity of the items. McDonald’s omega was calculated as well, which is currently recommended, as it gives less biased estimates14.
Table 1 Average score of the indicators evaluated by experts.
| PISQ-12 instrument questions | Indicator Relevance* | Sufficiency Indicator † | Comprehension indicator ‡ | Indicator essentiality # |
|---|---|---|---|---|
| 1. How frequently do you feel sexual desire? This feelling may include wanting to have sex, planning tohave sex, feeling frustrated because of lack of sex, and so forth. | 4.0 | 4.0 | 3.6 | 3.6 |
| 2. Do you climax (have an orgasm) when having sexual intercourse with your partner? | 3.8 | 3.6 | 4.0 | |
| 3. Do you feel sexually excited (turned on) when having sexual activity with your partner? | 3.8 | 3.6 | 4.0 | |
| 4. How satisfied are you with the variety of sexual activities in your current sex life? | 3.8 | 2.8 | 3.8 | |
| 5. Do you feel pain during sexual intercourse? | 4.0 | 3.4 | 3.6 | 4.0 |
| 6. Are you urinary incontinence (urine leakage) during sexual activity? | 4.0 | 3.4 | 4.0 | |
| 7. Does fear of urinary incontinence (either stool or urine) restrict your sexual activity? | 4.0 | 3.6 | 4.0 | |
| 8. Do you avoid sexual intercourse because of bulging in the vagina (either the bladder, rectum, or vagina falling out)? | 4.0 | 3.2 | 3.0 | |
| 9. When you have sex with your partner, do you negative emotional reactions such as fear, disgust, shame, or guilt? | 4.0 | 3.6 | 3.4 | |
| 10. Does your partner have an erection problem that affects his sexual activity? | 4.0 | 3.8 | 3.2 | 3.0 |
| 11. Does your partner have a premature ejaculation problem that affects his sexual activity? | 4.0 | 3.4 | 3.6 | |
| 12. Compared with the orgasms you have had in the past, how intense are the orgasms you have had in the past 6 months? | 3.6 | 3.0 | 3.0 |
* Item is relevant to assessment of its sexual dimension.
† Items from the same domain are enough to assess it.
‡ Item can be easily understood by a Chilean user.
# Item must be included, as it is essential for its dimension of sexual function.
A fact sheet, informed consent, and the full protocol were evaluated and approved by the Ethics Committee of the Health Service of Concepción, accredited by the Ministry of Health of Chile. Its resolution is N°002954.30.08.2013.
Results
All women invited accepted to participate in the study. Population is 217, age 27-85 years (M= 53.4; SD= 9.7); height: 1.20-1.75 m (M= 1.6; SD= 0.07); weight (n= 216): 42-140 kg (M= 72.3; SD= 11.8), and BMI (n= 216): 21.8-49.7 (M= 29.7; SD= 4.3). Vaginal births were 0-10 (M= 1.84; SD=1.80), C-sections were 0-6 (M= 1.08; SD= 1.34), and instrumental deliveries were 0-1.
Eighty two percent have a steady partner, 44.2% have completed secondary education or participated in tertiary education, and around 63.1% do not generate their own income. 13.0% have had 5 or more pregnancies, 17.1% have had 3 or more C-sections, and 11.5% have had an instrumental delivery. 40.6% suffer from recurrent UI. 89.4% had a UI when admitted to the unit, and the most common POP stage is III (Table 2).
Table 2 Description of the study population’s biosociodemographic and gyneco-obstetrical characteristics.
| Variable | Category | N (%) |
|---|---|---|
| Civil status | Married and Cohabiting | 178 (82.0) |
| Single, Separated and Widow | 39 (18.0) | |
| Educational level | No studies | 3 (1.4) |
| Primary education | 79 (36.4) | |
| Secondary education | 97 (44.7) | |
| Higher Technical Education | 30 (13.8) | |
| University education | 8 (3.7) | |
| Occupation | Dependent worker | 54 (24.9) |
| Independent worker | 26 (12.0) | |
| Unemployed | 19 (8.8) | |
| Retired and Pensioner | 18 (13.0) | |
| Housework | 90 (41.5) | |
| Number of term pregnancies | 0 | 3 (1.4) |
| 1-4 | 186 (85.7) | |
| ≥5 | 28 (12.9) | |
| Number of vaginal deliveries | 0 | 69 (31.8) |
| 1-4 | 39 (61.3) | |
| ≥5 | 15 (6.9) | |
| Number of cesarean deliveries | 0 | 106 (48.9) |
| 1-4 | 107 (49.3) | |
| ≥5 | 4 (1.8) | |
| Presence of Instrumental deliveries | 25 (11.5) | |
| History of recurrent urinary tract infections | 88 (40.6) | |
| Diagnosis of admission to the Pelvic Floor Unit of the High Complexity Hospital * | Pelvic organ prolapse stage I | 19 (8.8) |
| Pelvic organ prolapse stage II | 25 (11.5) | |
| Pelvic organ prolapse stage III | 48 (22.1) | |
| Pelvic organ prolapse stage IV | 24 (11.1) | |
| Urinary incontinence | 194 (89.4) | |
| Fecal incontinence | 12 (5.5) |
*Women can be admitted to the unit with one or more diagnoses, so the percentage is based on all 217 women and does not add up to 100%, unlike the other variables.
Among the experts, there was one urogynecologist and four pelvic floor physiotherapists. Maximum score was 4 points, mainly in "Item is relevant to assessment of its sexual dimension", where 75% of its items showed such score. On the other hand, the minimum score was 2.8, only for "Item can be easily understood by a Chilean user", which contained question 4 of the tool (Table 1). Experts were also asked to give a general evaluation, using the following indicators: the tool includes all possible elements to evaluate the sexual function in women with pelvic floor dysfunction (mean: 2.8; min.: 2; max.: 4), the contents of the tool are clearly stated (mean: 3.4; min.: 2; max.: 4), and the tool is relevant to assessment of sexual function in Chilean women with pelvic floor dysfunction (mean: 3.6; min.: 3; max.: 4).
The next part is a confirmatory factor analysis (CFA) of PISQ-12, evaluating the fit indicators for the three-factor model proposed by Rogers et al. 9 (model A), which showed acceptable scores for CFI (0.949) and TLI (0.934), but could not reach the cut-off scores for RMSEA (0.126 (0.109-0.143)) and SRMR (0.078). By evaluating the modification indexes, the most important index was discovered to be the correlated error between items 6 and 7, with a standardized estimated parameter change (SEPC) of 0.470 (Table 3). Because of this, the analysis was repeated, taking into account the correlated errors between these items (model B), and the result was adequate for CFI and TLI, but RMSEA and SRMR still had to reach an acceptable level. After re-evaluating the modification indexes, the correlated errors between items 5 and 12 became relevant (SEPC= 0.252), so fit indicators were calculated for a model with these newly found errors (model C). Given the indicators did not significantly improve and there was the risk of overfitting, model B was finally chosen (Table 3). Figure 1 shows estimated parameters for model B.
Table 3 Comparison of fit indicators of the three-factor model and the three-factor model with correlated errors for PISQ-12 when applied to Chilean women.
| Model | CFI | TLI | RMSEA (90% CI) | SRMR |
|---|---|---|---|---|
| A. 3 factors | 0.949 | 0.934 | 0.126 (0.109-0.143) | 0.078 |
| B. 3 factors* | 0.968 | 0.957 | 0.101 (0.084-0.119) | 0.066 |
| C. 3 factors** | 0.974 | 0.965 | 0.092 (0.074-0.110) | 0.062 |
TLI: Tucker-Lewis index.
CFI: Comparative fit index.
RMSEA: Root mean square error of approximation.
CI: Confidence interval.
SRMR: Standardized root mean square residual.
* Model with correlated errors (items 6 and 7).
** Model with correlated errors (items 6 and 7, plus 5 and 12).
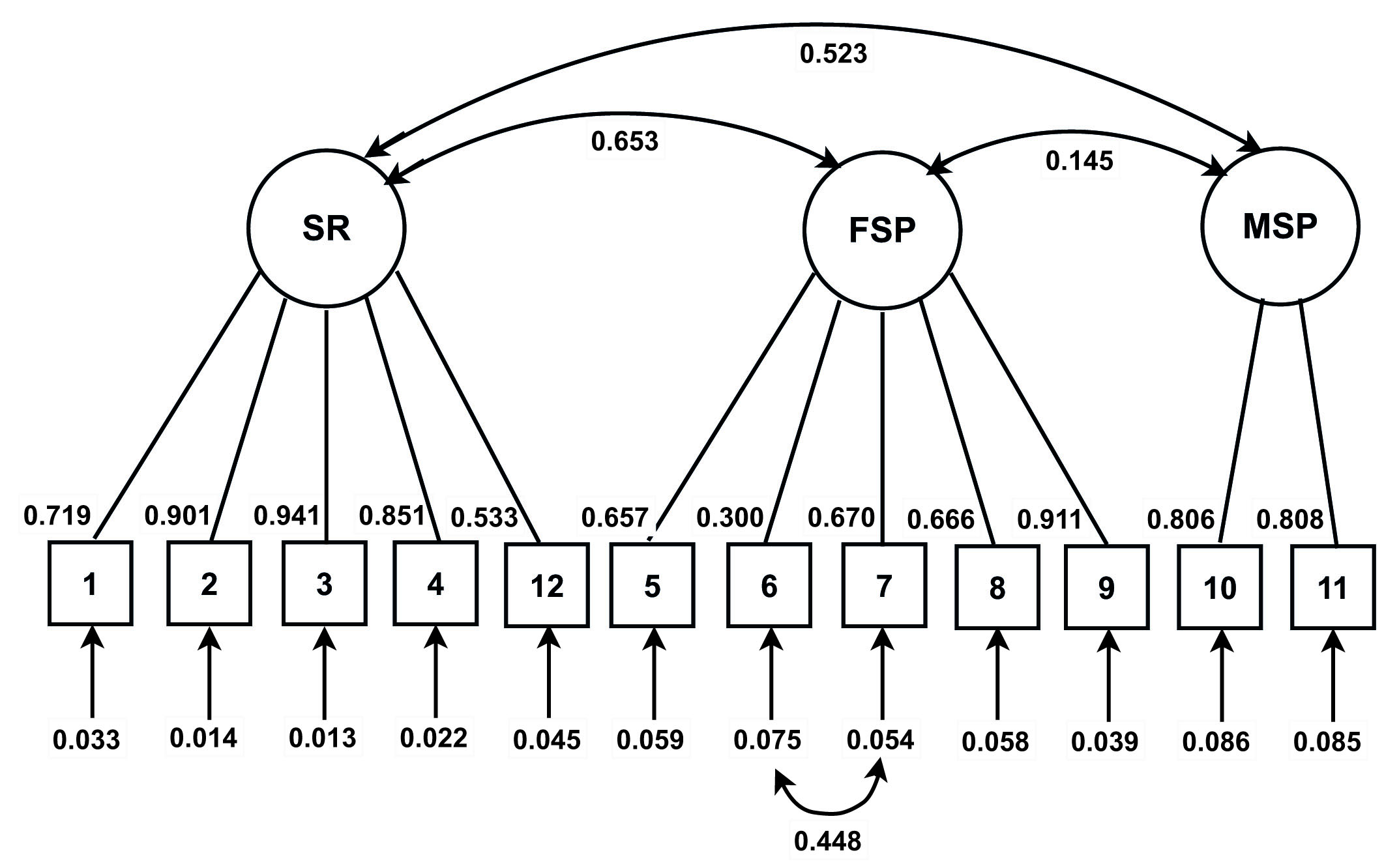
Figure 1 Three-factor model with correlated error between items 6 and 7 after a confirmatory factor analysis of PISQ-12, applied to Chilean women. SR: Sexual response; FSL: female sexual problems; MSP: male sexual problems.
Using Cronbach’s alpha, the most used coefficient for this purpose, the first factor showed good reliability (α= 0.856), the second was acceptable (α= 0.738), and the third showed poor results (α= 0.634). However, McDonald’s omega is being proposed nowadays, as it would give less biased estimates 14; in this case, all values for sexual response (ω= 0.897), female sexual problems (ω= 0.788), and male sexual problems (ω= 0.789) were adequate. Therefore, scores were calculated with this coefficient and then analyzed (Table 4).
Tabla 4 Descriptive analysis of the factors identified in the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). (N= 2,017)
| Factors | ω | M | DE | Mín | Máx | P25 | P50 | P75 | Asymmetry | Kurtosis |
|---|---|---|---|---|---|---|---|---|---|---|
| Sexual response | 0.897 | 10.31 | 5.34 | 0 | 20 | 6 | 10 | 15 | -0.27 | 2.06 |
| Female sexual problems | 0.788 | 10.82 | 5.52 | 0 | 20 | 7 | 11 | 15 | -0.12 | 2.20 |
| Male sexual problems | 0.789 | 6.49 | 2.18 | 0 | 8 | 5 | 8 | 8 | -1.30 | 3.73 |
Results show that sexual response and female sexual problems had a moderately symmetrical distribution (sexual response: P25: 6; P50: 10; P75: 15; asymmetry:-0.27, and female sexual problems: P25: 7; P50: 11; P75: 15; asymmetry: -0.12), while male sexual problems had a marked negative asymmetry (P25: 5; P50: 8, P75: 8; asymmetry: -1.30), and all three cases were noticeably leptokurtic (sexual response: 2.06; female sexual problems: 2.20, male sexual problems: 3.73), which shows highly homogeneous scores 12.
Correlation between sexual response and sexual problems was calculated. A better sexual response was associated with a lower perception of female sexual problems and a higher one of male sexual problems, with a medium effect size between both. In addition to this, although BMI did not have a significant relation to any factor, an association between older women and a better sexual response and less male sexual problems was found (Table 5).
Table 5 Spearman’s correlation among the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) factors, age, and BMI.
| Variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Sexual response | - | ||||
| Female sexual limitations | -0.46** | - | |||
| Male sexual limitations | 0.38** | 0.08 | - | ||
| Agen | -0.33** | -0.13 | -0.22* | - | |
| Body Mass Index (BMI) | -0.11 | -0.03 | -0.13 | -0.02 | - |
N=217; *: p<0.01; **: p<0.001
Moreover, sexual response is higher when there are fewer pregnancies and vaginal births, while sexual problems related to pelvic floor dysfunctions are not associated with pregnancy or number of births (Table 6).
Table 6 Spearman’s correlation among PISQ-12 factors and obstetrical characteristics.
| Variables | Sexual response | Female sexual problems | Male sexual problems |
|---|---|---|---|
| Number of pregnancies | -0.189** | -0.113 | -0.126 |
| Number of vaginal deliveries | -0.254*** | -0.102 | -0.185** |
| Number of cesarean deliveries | 0.157* | -0.032 | 0.116 |
| Presence of instrumentals deliveries | 0.026 | -0.089 | -0.057 |
N= 217; *: p <0.05; **: p <0.01; ***: p <0.001.
Lastly, a higher education is associated with a higher sexual response (rs= 0.36; p <0.001), female sexual problems (rs= 0.27; p= 0.001), and male sexual problems (rs= 0.19; p= 0.004).
Discussion
Population is mainly perimenopausal, highly educated -although with no income- and affected by UI. A psychometric analysis revealed three factors with a good and acceptable reliability, respectively: age, education, and number of pregnancies and births.
On the topic of content validity, the experts’ answers were highly homogeneous. Most coinciding percentages show a high degree of agreement 3,5 in whether the item was relevant, sufficient, understandable, and essential to the questionnaire or not.
Confirmatory factor analysis empirically supported the three-factor structure, the same as the two original articles 7,8.
When checking the three factors’ reliability, values ranged from α= 0.63 to α= 0.85, showing a changeable reliability that goes from “poor” to “good” 15. However, when using McDonald’s omega, values ranged from ω= 0.788 to ω= 0.897, which would mean that these values are an accurate measurement of the factors.
This study determined that older women had less score in the "Sexual response" dimension (rs= -0.35), for a moderate association. This result agrees with other two studies where older women with UI reported a higher prevalence of sexual dysfunctions17,18. In China, a study evaluated sexual function and quality of life in women with pelvic floor dysfunctions, and found that older women had a worse sexual function than younger women, as the first obtained lower scores in the general PISQ-12 and in its three factors 19. The impact of age on female sexual function was also assessed with the Female Sexual Function Index (FSFI), concluding that it is negatively correlated to sexual function 20). However, this tool has not been validated for its use in population with pelvic floor dysfunctions. In Poland, a study assessed sexual function in women with POP or only UI and its association with clinical and sociodemographic variables, finding that age was inversely correlated to users' sexual function in the general PISQ-12 and in two dimensions, "Emotional behavior" and "Partner-related factors" 21.
Women with a higher education level had higher scores in the “Sexual response” factor (rs= 0.36), which was also seen in studies in Turkey and Brazil 17,18,22. According to Cohen, the relation is moderate, as the value is around 0.3 16. In Chile, there is evidence of the relationship between a higher education level and higher levels of sexual satisfaction 23,24.
On the topic of OB-GYN history, a negative correlation between sexual response and number of pregnancies (rs= -0.19) and vaginal births (rs= -0.25), and a positive correlation between sexual function and number of C-sections (rs= 0.16) were found. However, it cannot be forgotten that the relation of these variables is weak (around 0.1) according to Cohen 16, unlike the moderate intensity of the relation between sexual function and number of pregnancies and vaginal births. The latter should be evaluated, since the changes in the pelvic floor produced by pregnancy, birth, and postpartum can condition the sexual response, either positively (with pelvic floor muscle training) or negatively (with no preparation for birth) 25.
There were two limitations in this study. First, although scientific literature suggests that psychometric studies should include 20 people per each item to obtain statistically significant results, this study could only include 18 per item; however, the results were deemed satisfactory, and they could be applied to a similar population. The second limitation was that, despite the small number of experts asked to review the tool, there was a high level of coincidence in the quality of the items included in PISQ-12.











 text in
text in 



