Remark
| 1) Why was this study conducted? |
| Pulmonary hypertension is a disease that generates functional limitations from mild to severe, these limitations are a consequence not only of cardiovascular-pulmonary but also muscular compromise. For this reason, a narrative review was carried out in which it was intended to establish the safety, evaluation and training strategies of the respiratory and limb muscles according to the existing literature. |
| 2) What were the most relevant results of the study? |
| According to the literature reviewed, limb and respiratory muscle training is safe and offers favorable results in aerobic capacity and health-related quality of life. The procedures must be correctly prescribed and it is recommended that they be part of a pulmonary rehabilitation program. |
| 3) What do these results contribute? |
| These results synthesize the evaluation tools and safe training of respiratory muscles and upper and lower extremities according to the existing literature. As well as, it promotes the referral of patients with pulmonary hypertension to pulmonary rehabilitation programs according to the inclusion criteria. |
Introduction
Pulmonary hypertension is defined as an increase in pulmonary artery pressure ≥25 mm Hg at rest 1. Pulmonary hypertension is a pathophysiological disorder that involves different clinical conditions; it can be a complication of most respiratory and cardiovascular disorders 2.
Patients with pulmonary hypertension present limited tolerance to exercise and aerobic capacity 3, which is reflected in the reduction in peak oxygen consumption (VO2peak), as well as in their functional performance evaluated with the six-minute walk test (6MWT) 4. This intolerance to exercise has traditionally been attributed to cardiac and respiratory dysfunction 5. However, as it happens in other chronic diseases 6, lower-limb and respiratory muscle alterations are also involved in patients with pulmonary hypertension 5,7,8.
Increasing evidence and recommendations from the American Thoracic Society and the European Respiratory Society suggest that physical exercise training is an efficient and safe strategy. The recommendation for light and moderate-intensity exercise is made within the framework of pulmonary rehabilitation. Its benefits have been previously described 9.
In diseases such as COPD, lower-limb muscle function, exercise tolerance, and quality of life improve following exercise training 10,11. Moreover, just as with COPD, pulmonary hypertension,it is necessary to promote evidence-based interventions with pulmonary hypertension. This narrative review focuses on the safety and efficacy of training the respiratory muscles and the muscles of the upper and lower extremities in patients with pulmonary hypertension.
Lower-limb muscle dysfunction
Lower-limb muscle weakness occurs in patients with pulmonary hypertension 5. This weakness is associated with dyspnea, angina, and syncope, inducing physical activity restriction. Furthermore, as the disease progresses, Health-related quality of life decreases, and functional limitations increase, causing alterations in physical health that restrict the social function of patients 12,13.
In COPD 14, there is a shift from type I fibers, which have a high mitochondrial intensity and oxidative capacity, to type II fibers, which are faster fibers with less resistance to fatigue and completely depend on anaerobic metabolism 15. It has been suggested that these changes also occur in pulmonary hypertension due to the finding that type IIx fibers displace type I fibers, which have an inverse correlation with the duration of the disease 16. Also, in pulmonary hypertension, the decrease in AKT and p70S6 with an increase in atrogin-1 has been identified as a relevant factor in muscle proteolysis with depression of networks that mediate hypertrophy. In addition to the phosphorylation of the ryanodine 1 receptor, which suggests the alteration of the sarcoplasmic reticulum directly involved in the production of Ca ++ 16. At a molecular level, there have also been identified a decrease in the extracellular signal-regulated kinase ERK, microRNA 126, and an increase in sprout-related EVH1 17.
The changes produced in the muscle may affect tropism, contractility, capillarity, and oxidative capacity. However, these alterations are not yet evident and defined 18. An increase in the expression of E3 ligases MAFbx/atrogin-1 and MURF-1 has been found, which are considered markers of activating the ubiquitin-proteasome pathway in muscles; causing reduction of transverse fibers and degradation of myofibrillar proteins 19.
Contractility is possibly altered by an increase in ryanodine receptor one phosphorylation, which alters the integration of muscle excitation-contraction 16. Likewise, mitochondrial density and its oxidative capacity 18 and reduced capillarity secondary to endothelial dysfunction are critical in the reduction in muscle performance present in patients with pulmonary hypertension, a situation that widely compromises their functionality and, therefore, their health-related quality of life.
Patients with pulmonary hypertension demonstrated a decreased type I/type II muscle fiber ratio and a smaller cross-sectional area of myofibres type I compared to healthy subjects 16. As well as an increase in RyR1 phosphorylation, which functions as a channel in which calcium is released from the sarcoplasmic reticulum towards the cytosol, in order to induce muscle contraction; hyperphosphorylation induces leakage, suggesting impaired sequestration 16. It has also been found that the increase in the expression of the MuRF1 protein is not only due to physical inactivity (as it happens in healthy subjects) but also as a consequence of the increase in pulmonary vascular resistance 20.
Lower-limb muscle atrophy leads to weakness, this increases the structural degradation of myofibrils and some proteins 21. All these structural changes cause functional alterations and consequently the compromise of the performance of daily activities associated with symptoms 22 and quality of life of patients 16 with respiratory and limb muscle damage 19. Consequently, muscle training emerges as a strategy to implement pulmonary rehabilitation programs. Physical exercise appears to be safe and effective, which is why there is a need to establish specialized programs for patients with pulmonary hypertension 23-25.
Patients with pulmonary hypertension are physically inactive, associated with a higher risk of hospitalization 26. Moreover, as physical inactivity may be one of the main drivers of lower-limb muscle weakness in patients with pulmonary hypertension, measuring physical activity levels seems of clinical importance 27,28. This also provides a clear rationale for why exercise-based interventions are effective in patients with pulmonary hypertension to increase muscle function and exercise tolerance and quality of life.
Respiratory muscle dysfunction
Patients with stage II-IV pulmonary hypertension reduce muscle strength compared to healthy individuals (25% less) 29. For being progressive, pulmonary hypertension results in a reduction in aerobic capacity and the strength of respiratory muscles 30. It has been identified that functional aerobic capacity is directly related to muscle strength in patients with pulmonary hypertension; diaphragmatic dysfunction has been reported in animal models and patients who suffer from exercise intolerance; in rats with pulmonary hypertension by the monocrotaline model, the contraction and the generation of the maximum tetanic force of the diaphragm were lower. The transverse fiber of the diaphragm was significantly smaller in pulmonary hypertension rats 31,32. In addition, histologically, there have been reported weakness and atrophy in the respiratory muscles of patients with pulmonary hypertension; a situation that strengthens the concept that this respiratory muscle dysfunction contributes to dyspnea and fatigue while exercising 33.
The maximum inspiratory and expiratory pressure values have been related to the distance in the 6-minutes walk test 8. Furthermore, pulmonary hypertension patients have been shown to experience hyperventilation both at rest and during exercise 34,35. Continuous muscle activity increases energy demand and reduces force-generating capacity; therefore, it is possible to infer that this direct relationship should promote the training of the respiratory muscles, and thus, indirectly, there will be an improvement in the aerobic capacity and in the functionality of the patients.
Evaluation
The evaluation of the patients should include a complete review of the medical history, including sociodemographic and clinical aspects such as dyspnea on exercise (36 and health-related quality of life 37. Furthermore, the evaluation of functional aerobic capacity has been included in various studies of patients with pulmonary hypertension 38,39. It is recommended that the same physical therapist perform the evaluations weekly.
Muscle evaluation involves instrumental strategies with mostly objective results; the alternatives are described in Figure 1. For the evaluation of the extremities, the arm ergometer, the 6-minute pegboard and ring test, and the one-repetition maximum have been used in the upper limbs. In lower limbs, the contractile leg fatigue, the one-maximum repetition and for deep analysis the quadriceps tomography and the biopsy for molecular tests. The evaluation of respiratory muscles is carried out mainly with a manovacuometer in which maximum inspiratory pressure and maximum expiratory pressure are obtained. Each of the tools described are described in detail below.
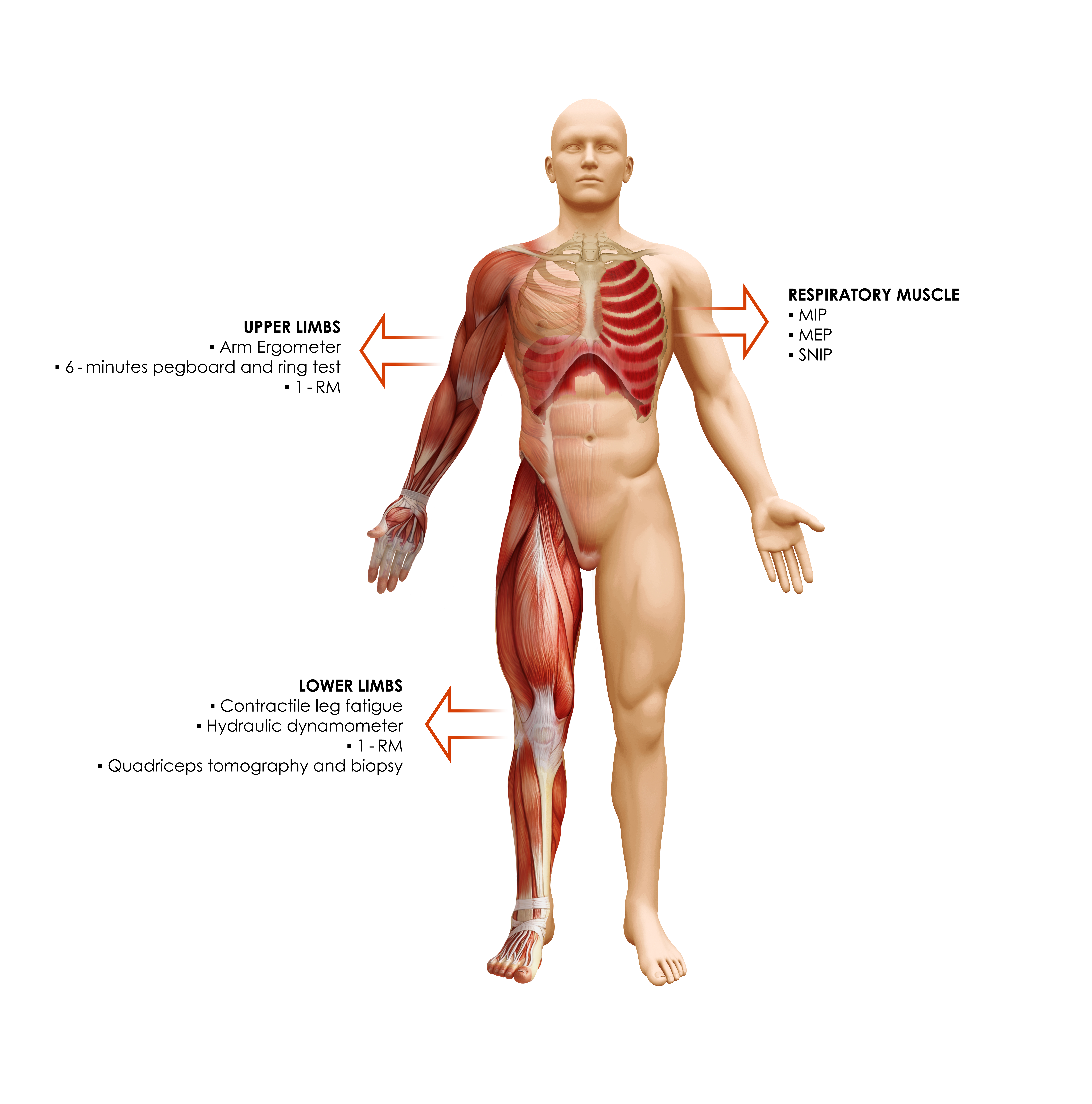
Figure 1 Muscular assessment is necessary to establish the goals of the intervention. Different instrumental strategies are included. The respiratory muscles are measured by pressure changes that allow identifying the inspiratory force generated by the diaphragm and the intercostals and the expiratory force by the abdominals; Its measurement is mainly carried out with a manovacuometer with which máximum inspiratory pressure and máximum expiratory pressure are measured. Regarding the evaluation of limb strength, the arm ergometer, the 6-minute pegboard and ring test and the one-repetition maximum are used in the upper limbs, and their assessment can be performed by muscle groups or by functional activities. In lower limbs, assessments focus mainly on quadriceps and triceps surae in which the contractile leg fatigue, the one-maximum repetition and for deep analysis, the quadriceps tomography and the biopsy for molecular tests have been applied. 1-RM: One-repetition máximum, MIP: Maximum Inspiratory Pressure, MEP: Maximum Expiratory Pressure, SNIP: Sniff nasal inspiratory pressure
Lower and upper-limb muscle function
For evaluating lower-limb strength, simple strategies such as one repetition maximum test are used, up to measurements that require specialized equipment such as computed tomography. The one-repetition maximum test is defined as the maximum weight that can be lifted with proper technique; in patients with COPD and other comorbidities, it is considered the gold standard in situations where laboratory tests cannot be performed. It is a well-tolerated and easily accessible test 40,41. The test consists of a warm-up with ten reps at a lightweight, followed by a 2-minutes rest period prior to the one-repetition maximum test. The initial weight is calculated according to the body weight and is progressively increased until reaching the maximum. A 60 second rest period is recommended between measurements 42,43.
Regarding specific assessments of lower-limb muscle strength, contractile leg fatigue after cycling has been used to assess nonvolitional and volitional strength in the quadriceps 44. During maximal voluntary contraction, patients sustain isometric force to the maximum possible for three seconds; signals are amplified and recorded in software 45.
Quadriceps function in pulmonary hypertension has also been assessed with hydraulic dynamometry 46; patients are positioned in hip flexion at 90°, knee flexion at 70°; the transducer is located approximately 10 cm above the medial malleolus. A maximum voluntary contraction is measured by making five attempts with a 1-minute pause between each attempt 47.
Assessment by computed tomography, especially in the quadriceps, has also been included. In addition, a muscle biopsy has been used from the non-dominant side to identify muscle capillarity and the enzymatic activity of the quadriceps 44. Nevertheless; These measurements are more related to research, and their clinical applicability is reduced significantly in countries with difficult access to diagnostic tools.
For upper limbs, in addition to the evaluation of a maximum repetition, the 6-minute pegboard and ring test has been used, in which the subjects must move rings ranging from 14 to 50 grams, as far as possible in 6 minutes, and the score was the number of rings moved during this time period.
Respiratory muscle function
Regarding the evaluation of respiratory musculature, the measurement of maximum inspiratory pressure and maximum expiratory pressure has been used in studies that include patients with pulmonary hypertension 29,48,49.
These evaluations are carried out with pressure devices that contain mouthpieces to make the measurements; the maximum inspiratory pressure maneuver is performed from a maximum expiration close to residual volume and the maximum expiratory pressure after a maximum inspiration. The maximum inspiratory pressure and maximum expiratory pressure values are calculated from the maximum sustained effort for one second; the tests are repeated until higher values are achieved with a difference of 10%; however, other authors consider performing three to five repetitions and taking the highest value of the tests performed 30,33. The sniff nasal pressure measurement has also been used by performing it from the residual functional capacity 49,50 (Figure 1).
Training
Limb muscle training
Low to moderate intensity exercises have shown safety in patients with pulmonary hypertension. It has been identified that training can improve exercise capacity and health-related quality of life. To start with the training protocols, patients are receiving their pharmacological therapies and are supervised, minimizing complications 4. Step climbing unsupported arm/leg exercises with and without dumbbells; use of circuits that involve large muscle groups using specific equipment for strengthening, such as leg and bench press, leg extension, lateral pulldown, and abdominal crunches 51. It has also been reported that strength training in the quadriceps should be progressive, and it depends on what was obtained in the initial evaluations, starting in the first week with three sets of 12 repetitions at 50% of the one-repetition maximum test and progressing to 75% at week 7, until reaching week 12 with the same series and repetitions. Regarding resistance, the number of repetitions is increased to 30, also three series, but starting in week one at 30% of the one-repetition maximum test and progressing to 40% in week 7, also until reaching week 12 46.
For the upper extremities, dumbbell workouts with low weight (500-1000 g) have been reported, focused on muscles independently 51,52; for 30 minutes, five times a week during 12 weeks; this could be due to the intention of carrying out safe activities that avoid as much as possible the appearance of complications related to musculoskeletal alterations and also to the heart-lung interaction 53.
One of the most reported results is the relative decrease in type IIx fibers after muscular training in pulmonary rehabilitation. This result is strongly correlated with the decrease in CO2 production 44; results that have been identified not only in pulmonary arterial hypertension patients but also in chronic thromboembolic pulmonary hypertension patients who also improved their functional aerobic capacity and quality of life 52.
It has been reported that after training, there is an improvement in the distribution of muscle fibers 23, Activities as bicycle ergometer with continuous (30 min 50% peak workload) and interval training (1 min high/30 slow; 10-25 min; 10-60 W; with intensity 60-80% peakVO2); progressive increase during program 54,55. The specific training of the quadriceps has caused improvement in the performance and muscular function, this improvement consequence of morphological changes through the increase in the capillarization and the oxidative enzymatic activity evaluated with vastus lateralis biopsy 46,56.
Neuromuscular electrical stimulation has been used as an intervention in patients with chronic pulmonary disorders and is an alternative for those who do not have enough capacity to participate in moderate to high-intensity exercise programs 57. This method is passive and more tolerable for patients with severe symptoms resulting from a low metabolic load on the cardiorespiratory system 58,59.
In pulmonary hypertension, although there is little evidence to support its use; An 8-week study used Neuromuscular electrical stimulation on quadriceps and delts with 50 Hz frequency in 350 μs pulses over an on: off duty cycle, which was increased weekly from 2:15 s to 5:20 s to 10:15 s. The intensity was increasing according to the tolerance of the patient. The protocol was scheduled for 40 minutes a day three days a week. The intervention improved peripheral muscle strength, muscle cross-sectional area and thickness, arterial stiffness, exercise capacity, functional mobility, balance, balance confidence, physical activity level, and quality of life in patients with pulmonary arterial hypertension 59.
In general, muscle training promotes the increase of the maximum and peak oxygen consumption; as well the reduction of symptoms during exercise measured with the Borg scale; likewise, at the hemodynamic level, changes in heart rate and systolic and diastolic pressures demonstrate benefits that range from functional to structural, with molecular and clinical changes 43,55.
When the results obtained are integrated, it has been found that strength training improves Health-related quality of life when evaluated with questionnaires such as CAMPHOR and SF36; changes generally occur in physical, mental, health perception, bodily pain, and vitality functions 43,55,60.
When training patients with a disease such as pulmonary hypertension, which has a high compromise in the cardiovascular and pulmonary system, with a high risk of complications, adverse effects are a risk. There have been reports of patients with syncope that can generally appear hours after training and episodes of tachycardia in patients with a history of arrhythmia; however, these adverse events did not transform into clinical worsening of heart failure resolved quickly. Continuous monitoring and training by highly trained personnel is the best way to mitigate these risks.
Respiratory muscle training
The patients that have been reported to benefit from respiratory muscle training are those with moderate 48 and even with severe pulmonary hypertension 61; due to the severity and cardiovascular compromise of the patients, the prescription must be carried out safely and effectively.
According to the evidence reviewed, the threshold inspiratory muscle training device is the most used to train muscles involved in inspiration, using loads of 30% of maximum inspiratory pressure for 30 minutes 7 days a week for six weeks 30. The threshold inspiratory muscle training allows training in a range from 9 cm H2O to 41 cm H2O. the loads generally start at 30% of the maximum inspiratory pressure; 15-minute workouts are reported twice a day for eight weeks, five days a week 48.
Training activities that are accompanied by respiratory therapy performed five times a week have also been included. Other activities, including exercises to stretch the muscles related to breathing and trunk muscles, techniques such as pursed lips and conscious modulation of breathing patterns 49, and yoga techniques (Ujjayi breathing), which have been shown to improve baroreflex sensitivity in a healthy population 62.
Continuous monitoring of hemodynamic variables is required to perform the procedures while the intervention is being performed. The cut-off point is suggested at ≤130/min in heart rate. Regarding the peripheral oxygen saturation, a saturation value ≤85% is considered to decide to reduce the intensity; in cases where saturation decreases, the patients can receive supplemental oxygen during the performance of the procedures, which can be delivered utilizing low or high flow 63.
It has been reported that the addition of respiratory muscle training to the functional treatment of the upper and lower extremities offers more significant benefits to the improvement in the function of the muscles that are involved, also the positive benefits in the cardiocirculatory system, quality of life and the reduction of dyspnea during exercise 61. However, another study showed that performing muscle training with a threshold inspiratory muscle training device five days a week for 15 minutes, twice a day, only managed to improve the strength of the respiratory muscles, but no other parameters (quality of life and symptoms). This result may reinforce the idea that muscle training should be carried out in both respiratory muscles and limb muscles; and that the benefits are obtained with localized training accompanied by global training 48 (Table 1).
Table 1 Strategies and observations for muscle training in patients with pulmonary hypertension
| Region | Strategy | Observations |
|---|---|---|
| Respiratory Muscles | Threshold inspiratory muscle training device | Allows training in a range from 9 cm H2O to 41 cm H2O. the loads generally start at 30% of the maximum inspiratory pressure 8,30 |
| Lower Limbs | Specific equipment for strengthening | Leg and bench press, leg extension, and lateral pulldown; starting in the first week with 3 sets of 12 repetitions at 50% of the one repetition maximum test and progressing to 75% at week 7 for strength 46,51 |
| For resistance, the number of repetitions is increased to 30, also 3 series, but starting in week 1 at 30% of the one repetition maximum test and progressing to 40% in week 7 46. | ||
| Upper Limbs | Dumbbell workouts | Low weight (500 - 1000 gr) have been reported, focused on muscles independently for 30 minutes, five times a week during 12 weeks. Making increments according to the patient's response 4,51,53 |
Conclusion
There are several alternatives for muscle testing and training in pulmonary hypertension. Muscle training in patients with pulmonary hypertension has been shown to be safe and effective; the selection of the appropriate patient, based on the severity of the disease, taking into account the values obtained in the right heart catheterization, imaging, biomarkers, and functional classification of patients; promoting early inclusion in training programs, which may be within the framework of pulmonary rehabilitation; is essential to choose forms of assessment and intervention.











 text in
text in 



