Remark
| 1) Why was this study conducted? |
| This study was conducted because we wanted to describe the changes in cervical cancer mortality over time, separating each of the effects. In such a way that we could be clear about the behavior for each age group, each period or each cohort and thus be able to associate interventions that could explain these trends. |
| 2) What were the most relevant results of the study? |
| We found that cervical cancer mortality is explained by age, period, and cohort effects. The most relevant changes could be associated with interventions that modified the frequency of risk factors or cofactors, that helped early diagnosis or that increased progression-free survival. |
| 3) What do these results contribute? |
| The results are an important input for new research questions, for example, to determine the influence of each of the interventions on cervical cancer frequencies. On the other hand, they show that APC models are an important input when analyzing the temporal trends of a health event, particularly for cervical cancer mortality, since they allow a more precise analysis of the possible consequences of specific interventions. |
Introduction
By 2020, cervical cancer was the third cause of incidence and the fifth cause of cancer mortality in Colombian women. There were 4,742 new cases and 2,490 deaths were reported, with a crude incidence rate of 18.3 cases per 100,000 women and a mortality rate of 10.1 per 100,000 women 1. On the other hand, in 1990 it also ranked third in incidence and mortality, with a crude rate of 22.3 per 100,000 women and a mortality rate of 6.2 per 100,000 women 2. Therefore, despite observing a clear decrease in both incidence and mortality, it continues to be a pathology of great importance that requires improvements in screening programs, prevention strategies, and improved opportunities for access to treatment, as well as the analysis of the behavior of its frequencies is relevant.
In Latin America and the Caribbean, Colombia ranks 19th (out of 30) in incidence with an age-standardized rate of 14.9 per 100,000 women, equal to the rate for the entire region, while in mortality it ranks 22nd with an adjusted rate by age of 7.4 per 100,000 women 1.
The analysis of the cancer mortality trend has been studied in different regions of the world and has even been analyzed as an indicator of quality of life 3. Cancer incidence and mortality rates are closely monitored to track the burden of cancer and its evolution in different populations 4,5, provide etiological theories and hypotheses of the different types of cancer 6-9, show inequalities 10,11 and evaluate: the diffusion, implementation, and possible effects of the different kinds of procedures for early detection, diagnosis 12,13, and therapeutic innovations 14.
A standard "toolbox" of graphical and quantitative methods for the analysis of cancer incidence and mortality has been developed. Perhaps the most widely used methods include classic descriptive plots based on the Lexis diagram 10, age-standardized rates, estimated annual percentage change, and the joinpoint regression method 15. However, this type of methodology does not allow discriminating the effects of age, period and cohort. The age-period-cohort (APC) model has been developed in the statistical literature as a mathematical counterpoint to purely descriptive approaches 10, which is based on fundamental generalized linear model theory and allows the epidemiologist to generate and test hypotheses about the trends.
The age-period-cohort (APC) models identify whether the changes in the incidence or mortality of the disease are due to the effects of changes in the age of the population; to factors located at a moment in time and that have an influence on all age groups simultaneously, generally associated with period effects (date of death); or to factors that affect a generation (birth cohort), which show changes of magnitude in the rates of the different age groups in successive periods. Likewise, the APC models are adjusted to determine the effect of each of these factors, separately, on the evolution of an outcome over time. 11.
In Colombia, these types of models have not been adjusted for the analysis of mortality from cervical cancer. This paper aims to determine the temporal effects, through an APC model of cervical cancer mortality in Colombia, during the period 1985-2014, following the methodology proposed by Carstensen 10.
Materials and Methods
The information on mortality from cervical cancer for the period 1985-2014 was obtained from the official records of death certificates processed by National Department of Statistics (DANE) 16. Information on age, date of death, place of residence and underlying cause of death was used from each record. Information on deaths from cancer in patients older than 20 years was included.
The basic cause of death was coded by DANE according to the International Classification of Diseases (ICD). 17; until 1997 the ICD-9 was used and later the ICD-10. The ICD codes used were 180.0 and 180.1 for ICD-9 and C53.0, C53.1 for ICD-10. Cases without age and with residence abroad were eliminated. Population projections for Colombia made by DANE were used to estimate the population at risk. 16. Ages and periods were grouped in five-year groups from 20 years old to reaching the category of 80 years or more.
Truncated age-adjusted rates, starting at age 20, were calculated using the Segi world reference population. 18, for each period.
To model mortality rates as a function of age (𝑎), period (𝑝), and cohort (𝑐), a generalized linear model with Poisson response, canonical link function (natural logarithm), including age, period and cohort as factors. Five models were adjusted: age, age-drift, age-cohort, age-period-cohort and age-period, which were compared through the likelihood ratio test, to establish the significance of each of the effects.
To fit the age-period-cohort model, an age-drift model was first fitted, estimating the average annual percentage change (APPC) in mortality rates during the 30 years of observation (Equation 1).
Where α a is the effect of age group 𝑎, ε is the random error and δ the slope of the period (drift), which allows calculating the APPC of mortality rates, adjusted for age (Equation 2).
For a more detailed description of mortality, an age-period-cohort model was fitted to the rates λ𝑎𝑝, using the methodology proposed by Carstensen 10. The estimates were obtained by maximum likelihood, under the restriction that the effects of the period are zero on average and with zero slope, taking ages, periods and cohorts as factors (Equation 3).
The exponential of the age coefficients (𝛼𝑎), are the age-specific rates in the reference cohort (1950); those of the cohort (𝛽𝑐), are the rate ratio with respect to the reference cohort; and those of the period (𝛶𝑝), the ratio of rates relative to a prediction of an age-cohort model (residual). The results of the age, period and cohort effects are presented graphically with a confidence level of 95%.
The analyses were performed with the statistical program R. For the estimation of the age-period-cohort models, the Epi package 10 was used and the Akaike information criterion (AIC) was used to compare the fit of the models.
Results
During the study period, there were 42,567 deaths from cervical cancer, among these, only 56 (0.13%) did not have age information, so they were excluded from the analysis. The age-adjusted mortality rate from cervical cancer for the period 1985-1989 was 12.26 deaths per 100,000 women-year, while for the period 2010-2014 it was 10.34 deaths per 100,000 women-year (Table 1), showing an APPC, controlled by age, of -1.38% (95% CI: -1.49% to -1.04%).
Table 1 Mortality rates (crude) by period and proportion of deaths due to malignant neoplasm of uterus, part unspecified (C55).
| Period | 1985-1989 | 1990-1994 | 1995-1999 | 2000-2004 | 2005-2009 | 2010-2014 |
|---|---|---|---|---|---|---|
| Crude rate per 100,000 | 12.26 | 11.42 | 13.20 | 13.15 | 11.88 | 10.34 |
| Deaths in unspecified part (%) | 30.30 | 28.13 | 19.29 | 17.23 | 14.5 | 13.12 |
Estimates of mortality from cervical cancer presented a particular trend, with respect to age, an exponential trend was observed in the mortality rate up to 50 years, with a significant decrease in the slope up to 70 years, when it increases again. With respect to the cohort, in general, there is a decrease in risk for the younger cohorts, although an increasing trend was observed since the 60s, remaining below or at most at the same level as the 1950 cohort. For the period, an increase in the estimated risk is observed in the 90's, it remains constant until 2002 and then decreases (Figure 1).
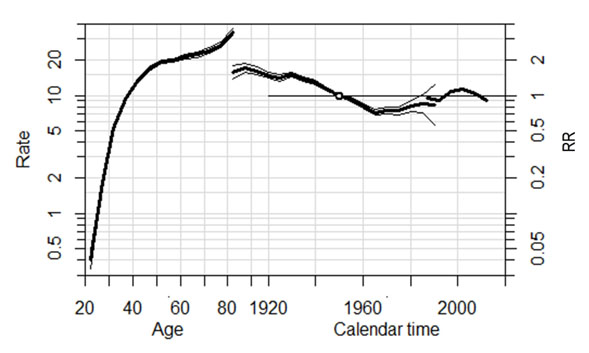
Figure 1 Estimation of the effects of age and 95% confidence intervals: estimated age-specific mortality rates (left), period: rate ratio (right), and cohort: rate ratio (RR) with respect to the reference cohort (center), for cervical cancer mortality, 1985-2014. APC model.
The results of the APC models are shown in Table 2. The model that best fits cervical cancer mortality includes effects of age, period and cohort, since it is the model with the lowest AIC (137.66). Additionally, by comparing models, the significance of these effects can be observed (4 vs 2, p-value= 0.000 and 5 vs 3, p-value= 0.000). On the other hand, a good fit of the model was obtained, since it explained 99.4% of the mortality variability (pseudo R2= 99.4%).
Table 2 Results of the APC models for cervical cancer mortality in Colombia during the period 1985-2014.
| Model | Model description | Goodness of fit | Model Comparison | ||||
|---|---|---|---|---|---|---|---|
| Df | Deviance | AIC | Comparison | Deviance | Df | ||
| 1 | Age | 65 | 1096.36 | 1226.36 | 2 vs 1 | 583.87 | 1 |
| 2 | Age - drift | 64 | 512.49 | 640.49 | 3 vs 2 | 268.29 | 4 |
| 3 | Age-period | 60 | 244.20 | 364.20 | 4 vs 2 | 186.50 | 16 |
| 4 | Age-cohort | 48 | 326.00 | 422.00 | 5 vs 4 | 276.34 | 4 |
| 5 | Age-period-cohort | 44 | 49.66 | 137.66 | 5 vs 3 | 194.54 | 16 |
Discussion
The burden of cervical cancer is greatest in low- and middle-income countries, which account for approximately 90% of women who die of cervical cancer globally 19. In Latin America, both incidence and mortality rates are higher than those of more developed countries such as the United States. At the regional level, it has been found that, in general, the highest rates of morbidity and mortality from cervical cancer are found in countries with the lowest human development index 20.
During the period of this study, Colombia was located at an intermediate point between the countries of the region, in addition, a decrease in mortality over time (EAPC = -3.2) has been evidenced in different studies, which is consistent with the results found 2,7,21. On the other hand, it is known that factors related to one's own sexual behavior and that of the partner increase the risk of HPV infection, a necessary cause for cervical cancer. Likewise, cofactors such as: high parity, smoking, prolonged use of oral contraceptives and sexually transmitted co-infections such as HIV, are associated with the appearance of this type of carcinoma 22 and could explain, in part, the behavior of mortality.
The results show that cervical cancer mortality in Colombia is determined by age, period and cohort effects. Estimates of age-specific mortality rates are consistent with incidence estimates based on reports from population-based cancer registries, in which there is a fast-growing trend up to age 45 years, followed by a gentler slope up to age 70 years when a steeper slope is observed again (19. This increase, observed after 70 years, may be related to the increase in life expectancy at birth in women, which has gone from 70 years in 1980 to 78 in 2010 and is consistent with the finding in Colombian women of a second peak prevalence of HPV infection in women over 55 years of age (13.2%), found in a study that analyzed a cohort of women in Bogotá D.C., which also suggests that the possible causes of this increase may be related to reactivation latent infections, hormonal changes, changes in partners or sexual behavior of their partners 23.
Regarding the effects of the periods, the decrease in the estimated mortality rates, starting in 2005, may be related to factors such as: the implementation of multiple strategies to favor the early detection of lesions, changes in the frequency of factors of risk and advances in the treatment of the disease, which could have had an effect mainly in the groups of younger women, as we will explain below. In the 1960s Profamilia and the Liga Colombiana contra el Cáncer (Colombian League Against Cancer) made the first attempts to establish a screening program, however, due to lack of organization and little participation, they were not successful, until in the 1990s a national program coordinated by the Instituto Nacional de Cancerología (National Cancer Institute), promoting the performance of cervicovaginal cytology outside the maternal care program, to reach the high-risk population. This program was regulated in 2000 by Resolution 412, which led to a decrease in the incidence of cervical cancer and therefore in mortality due to this 24,25; similarly, in 2004, colposcopy with biopsy was included for women affiliated with the subsidized regimen 26. Likewise, what has been observed since 2005 may be related to the decrease in the prevalence of some risk factors such as smoking, which went from 21.4% in 1993 to 12.8% in 2007 27. Another factor may be related to the fact that at the end of the 1990s a concomitant chemo-radiotherapy scheme with cisplatin began to be implemented for patients with locally advanced cancer, which showed an improvement in progression-free survival and a decrease in mortality 28.
The model estimated that the risk of death decreases until the cohorts born after the 60s, where it begins to rise until the younger cohorts, without reaching the levels of the 1950 cohort. Some possible explanations may be related to changes in the frequency of some cofactors, as well as risk factors for HPV infection 22,29. One of these cofactors is the long use of oral contraceptives, which began to be used in the 1960s, when the first contraceptive pill was approved in the United States and the first pills arrived in Colombia. From this moment, the cohorts began to be exposed to the use of oral contraceptives, likewise, this leads to modifying the sexual behavior of women, possibly increasing risk factors for HPV infection, such as the age of onset relationships and the number of sexual partners, increasing the risk of developing cervical cancer 30. This could be combined with poor access to the health system and therefore early detection of precancerous lesions, particularly in regions strongly affected by violence in some remote territories, especially during the 80s and 90s (decades in which women born between the 60s and 70s would begin to have an active sexual life), where illegal groups disputed control, which not only hindered access to health services but also made women the main victims of sexual abuse . This is also reflected in the cancer mortality atlases in Colombia, which have shown higher mortality in regions near navigable rivers, as well as in the Orinoquía 6,31.
In the future, an analysis using APC models will allow evaluating the effects of the incorporation of the human papillomavirus vaccine within the Expanded Program on Immunization (EPI) in Colombia, which included the HPV vaccine since August 2012, for through the implementation of the catch-up program for schoolgirls aged 9 to 17 32. Given that some studies have reported that vaccination with the bivalent or tetravalent vaccine can prevent up to 68% of cervical cancer and between 48-81% of other types of cancer related to HPV, a significant decrease in the cervical cancer mortality is expected in the corresponding cohorts. Likewise, when the 9-valent vaccine begins to be applied in the country, it is expected to prevent 88% of cervical cancer and 85-100% of other HPV-related cancers 1, which could also be analyzed and evidenced in the future through these models.
On the other hand, Resolution 3280 of 2018 adopted the guidelines on the screening strategy for cervical cancer in the country, indicating cytology for women between 25 and 30 years of age, HPV testing between 30 and 69 years of age and VIA/VILI strategy for remote populations with low access to health systems 33. The implementation of this program is expected to reduce the number of routine screening visits and create an adequate follow-up line to guarantee treatment within 30 days after diagnostic confirmation by colposcopy/biopsy 24. The results of this regulation can be evaluated in the future and will most likely be reflected in period or cohort effects.
Limitations
Mortality data come from official death registries, which may be underreported, especially for periods prior to 1997, because the information collection system was done through the municipal mayors, which reported based on individual death certificates. No adjustment was made for registration coverage, which could lead to underreporting of mortality rates. Likewise, given that the denominators of the rates were taken from the population projections made by DANE, it is possible that they do not completely reflect the real population behavior; however, it is hoped that these differences have not been more accentuated in some age group or at some point in time 34.
In addition, only information related to deaths coded with cause of death C53 was included, i.e., no redistribution of cases of malignant tumor of the uterus in unspecified part (C55) was made. The above could modify the observed changes in mortality by period, considering that the percentage of deaths reported as C55, of the total of those related to cancer of the uterus, has been decreasing over time (Table 1), especially in the first five years analyzed. However, this would not change the downward trend in mortality estimated since 2000 (Figure 1).
Another important consideration when analyzing the results is that the confidence intervals for the younger cohorts are quite wide, due to the few cases that are presented for these cohorts, so it is advisable that further analyses such as this one continue to be carried out to corroborate the trends obtained. Similarly, it should be kept in mind that the APPCs should be interpreted with care, since they are averages and therefore tend to be unstable when the study period is long.
Other studies are needed to directly link the possible causes of cervical cancer mortality trends in order to evaluate programs and new technologies ranging from screening to treatment.
Conclusion
Integrated cancer prevention campaigns, effective screening programs and effective access to treatment have played an important role in the reduction of cervical cancer mortality. Demographic factors and the demographic transition may be explanatory processes for the behavior of cancer mortality in the Colombian population, as well as the implementation of public policies within the health system in the last two decades.











 text in
text in 



