Introduction
Mullerian malformations are a heterogeneous group of alterations that occur in the reproductive system, secondary to alterations in the development, fusion, or canalization of the Müllerian ducts in the embryonic stage 1
The literature reports the appearance of these alterations since 330 BC, being Columbo, in the XXVI century, the one that brings to public knowledge the first case of vaginal agenesis. Subsequently, the first classification of these anomalies was made in 1979 by Buttram and Gibbsons. However, it was only until 1988 that the American Society for Reproductive Medicine (ASRM) proposed a classification based on anatomy, and later in 2013, the European Society for Human Reproduction and Embryology (ESHRE) and the European Society for Gynecological Endoscopy (ESGE) carried out the classification that remains in force to date 2
The prevalence of these malformations, reported in the general population, ranges around 5%, reaching 8%, 13%, and 24% in infertile women, those with spontaneous abortion, and infertile women with a history of spontaneous abortion 3
Within the classification of these malformations, the ESHRE / ESGE system expresses uterine anatomical variants derived from the same embryological origin, where the following main classes stand out: U0, normal uterus; U1, dysmorphic uterus; U2, septate uterus; U3, bicorporal uterus; U4, Hemi-uterus; U5, aplastic uterus; U6, for cases not yet classified. Each class is subdivided into subclasses that express some anatomical variety with clinical importance 2
Class U4 (Hemi-uterus) refers to cases of the unilaterally formed uterus. In the hemi-uterus, a formation defect, the uterus develops unilaterally, with the contralateral part incomplete or absent. Depending on whether there is a functional rudimentary uterine hemicity or not, class U4 is subdivided into class U4a and U4b. Class U4a presents a Hemi-uterus with a rudimentary functional cavity characterized by the presence of a communicating or non-communicating horn. Class U4b, on the other hand, is characterized by the presence of a non-functional contralateral uterine horn or by its aplasia 2
Given the complications associated with this Mullerian malformation (hematocavity, ectopic pregnancy in a rudimentary horn), surgical removal of the rudimentary cavity has been recommended, even if the horn is communicating 4,5
This investigation presents a report of three cases that pose a surgical proposal for Hemi-uterus repair with a non-communicating functional rudimentary cavity (Figure 1A) in adolescent patients with disabling pelvic pain during menstrual periods to depressive states and functional disability secondary to pain.
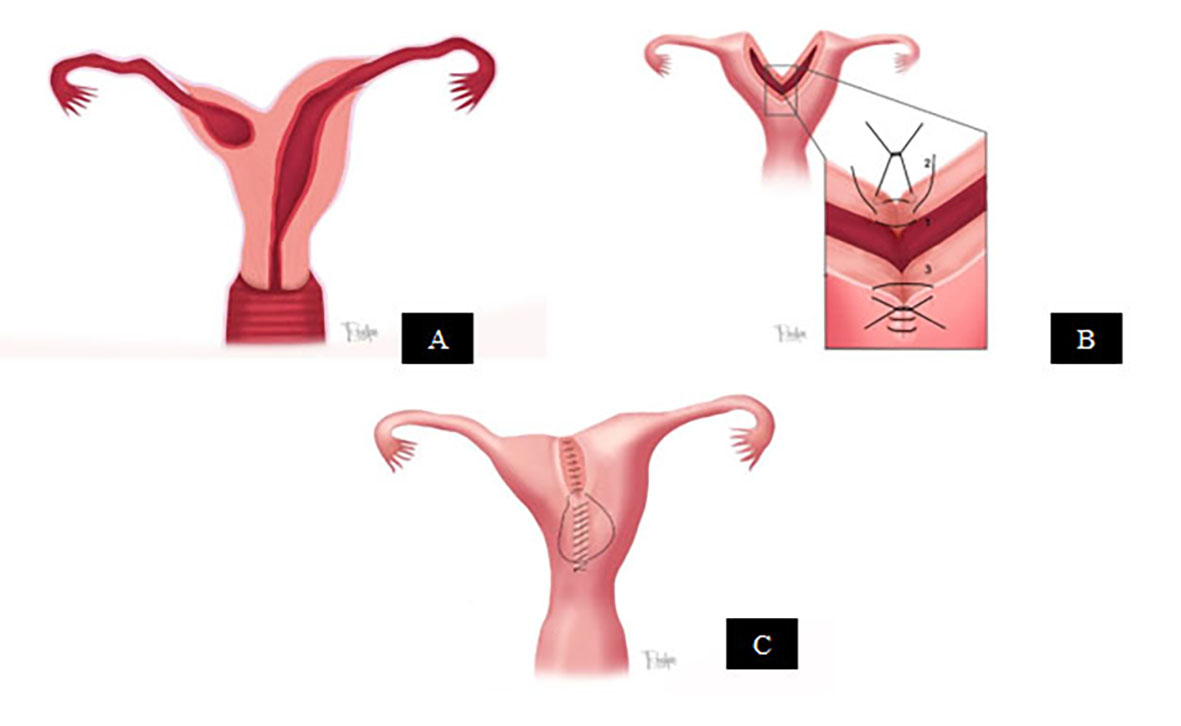
Figure 1 A: Graphic representation of Hemi-uterus with non-communicating functional rudimentary uterine cavity, Class U4a. B: Graphic representation of the surgical technique (three-layer suture). 1) Endometrial premucosa. 2) Muscular. 3) Serosa. C: Graphic representation of the postoperative result.
The obstetric result in the follow-up process of one of the cases is mentioned.
Case reports
1- A 13-year-old patient, G0 P0 presented with severe cyclical dysmenorrhea of about 18 months of evolution, associated with nausea, emesis, and inability to have sexual intercourse. Physical examination: weight 57 kg, average breasts, abdomen with tenderness in the hypogastrium, normal external genitalia. On digital rectal examination: small uterus, nonpalpable adnexa, marked pain towards right iliac fossa (RIF). The performance of a transvaginal ultrasound showed uterine malformation, and magnetic resonance imaging (MRI) revealed Hemi-uterus with a rudimentary functional non-communicating right uterine cavity. She was treated with anti-inflammatories and analgesia without improvement.
2- 12-year-old patient, G0 P0 presented with severe cyclical dysmenorrhea, nausea, postural hypotension, and inability to have sexual intercourse. In addition, signs of mild depression and easy crying were observed. She requested radical surgical treatment (Hysterectomy) because of her pain. On physical examination: weight 52 kg, IV tanner breasts, hypogastric pain on deep palpation. On digital rectal examination: small uterus, irregular towards left annex. A transvaginal ultrasound was taken, and it showed an arcuate uterus. MRI revealed a Hemi-uterus with a rudimentary functional non-communicating left cavity and a hematometra at the level of the rudimentary left cavity.
3- A 13-year-old patient, G0 P0 presented with dysmenorrhea, severe colic, episodes of emesis of 8 months of evolution, without surgical and pathological history, and without sexual initiation. This patient took analgesics and anti-inflammatory drugs chronically without improvement. On physical examination: weight of 53 kg, with decay signs and easy crying, normal thyroid, IV tanner breasts, pain with deep palpation in the hypogastrium, normal external genitalia. On digital rectal examination: a small and painful uterus, difficult to locate due to pain. Transvaginal ultrasound showed a Hemi-uterus with a functional rudimentary right cavity not communicating with a hematometra; RNM confirmed findings.
In all cases, a hysteroscopy was performed. As a result, it was possible to appreciate the following: single cervix, elongated uterus with a reduced uterine endometrial cavity in area, and the presence of a single ostium on the side of the communicating horn.
The surgical procedure performed on the patients, once it was explained to their parents and having obtained informed consent for its performance, was carried out as follows:
Under general anesthesia and in lithotomy position, a Foley catheter (number 18) was placed in the uterine cavity. The balloon was inflated with ten cc of distilled water, and R33 was connected with a 20 cc syringe containing methylene blue diluted 1 to 10 cc with saline solution. A bladder catheter was placed for drainage.
Suprapubic incision of the Pfannenstiel type and dissection by planes to the abdominal cavity was made. The non-communicating horn was identified in each case. Normal tubes and ovaries were noted in each patient, and endometriosis was classified according to the American Society for Reproductive Medicine (ASRM) criteria 6. The bladder insertion to the uterus was evaluated in the anterior face and from the colon to the posterior face to determine abnormal insertions that could favor the presence of complications. Intraoperative chromopertubation was performed with R33, injecting methylene blue into the uterus, showing the blind horn, its distention, and the permeability of the tube on that side. Both horns were opened with a 2 cm or 3 cm incision to adequately reveal both cavities stained with methylene blue (Figura 2).
The approach point was initially placed at the lower edge of both openings at the submyometrial level to approximate the cavities with Prolene 3.0 and a cardiovascular needle. Then, a three-layer suture was performed as follows to join both cavities (Figure 1B. Figura 3A, 3B, and 3C ):
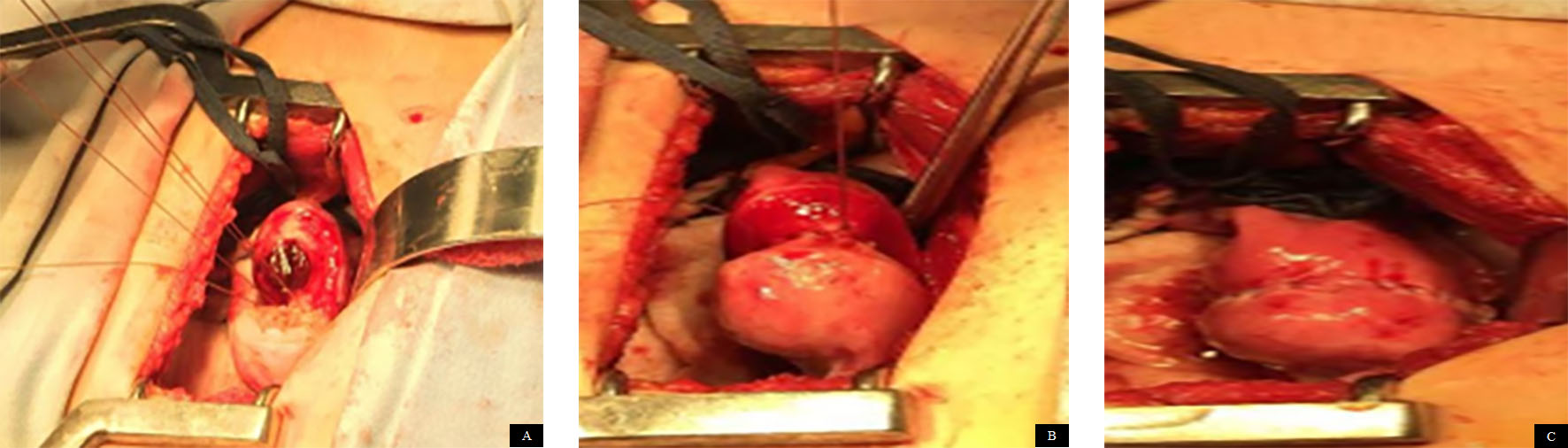
Figura 3 A: Approach point to the lower edge of both openings, at the submyometrial level, to approximate the cavities. B: Join both cavities: suture in the muscular plane. C: Three-layer suture: continuous suture with invaginant technique in the serosa. Final visualization of the procedure.
First layer: endometrial premucosa with 3-0 chromic catgut continuous suture (Figura 3A ).
Second layer: muscular (myometrium), with chromic catgut 2-0 continuous suture (Figura 3B ).
Third layer: serosa, with prolene 3.0 cardiovascular needle, continuous suture, invaginating technique (Figura 3C ).
Subsequently, chromopertubation with methylene blue was performed through a urinary catheter, showing simultaneous permeability in both tubes and no evidence of leakage through the suture. Endometriosis foci were flashed, and a mechanical barrier was placed: Intersed, in all of them to prevent adhesions. In Figure 1C and Figura 3C , the final result regarding the three published cases is represented.
All patients received prophylactic antibiotics and had a good postoperative evolution. The patients were assessed at the 1st, third, and sixth months, showing a marked improvement in their dysmenorrhea. They considered a minimum pain of approximately 1 to 2 on a scale of 1 to 10. In addition, there was an improvement in the depressive state; there was no change in the volume of her menstrual bleeding, and one of these patients achieved pregnancy with normal prenatal control and cesarean delivery, obtaining a full-term newborn without complications.
Discussion
The incidence of Mullerian malformations is not yet well known, with an estimated prevalence of up to 5.5% in the general population has risen secondary to advances in the different diagnostic imaging modalities. Its diagnostic detection and management are important since it affects the quality of life of patients, with marked symptoms of dysmenorrhea, pelvic pain, low self-esteem (depression), sexual difficulties, which can appear months after menarche, and alterations associated with the fertility process 7
The Hemi-uterus subclass U4a is characterized by having a functional rudimentary uterine cavity, which may or may not be a communicating one. Clinically, it can generate the presence of disabling chronic pain and adverse obstetric events, for which it is a pathology that may require surgical management to help alleviate symptoms and improve reproductive prognosis in a selected population 8
Among the techniques mentioned, the removal of the horn has been done through an open abdominal approach and sometimes by a laparoscopic technique, depending on the training and skill of the surgeon. Surgery that, although it can remove the symptoms in the patient, is bloody and does not favor subsequent reproduction. In the case of pregnancy, they could present multiple complications, such as the threat of premature labor and abortion.
In 1907, Paul Strassman first described the surgical correction of the double uterus; since then, the Strassman metroplasty has stood out as the standard procedure for the correction of the bicornuate uterus, showing a success rate for conception, reaching term gestation of up to 70-80% after the procedure; in addition to the improvement of the painful symptoms referred by the patients 9, for which continuing to innovate in less radical procedures can be the future advance in the area of microsurgery in Gynecology.
However, the Strassman technique is not fully indicated in the present case since it is not a pure bicornuate uterus, which limits its use.
The microsurgical technique proposed in this paper allows the early resolution of the problem, with substantial improvement of the symptoms in the patients (McGill Pain Questionnaire) 10, without the need to perform a resection of the horn and rudimentary uterine cavity, which is established in the literature as a primary treatment option for Hemi-uterus with a non-communicating functional rudimentary cavity 11) This procedure could contribute to conserving or improving long-term reproductive options in these patients by preserving a more significant amount of endometrial tissue.
It should be noted that the microsurgical technique leads to a decrease in the formation of adherent tissue, which limits long-term fertility and improves the anatomical disposition to avoid subsequent ectopic pregnancies. At the same time, we presume that by having a uterine cavity with a larger area, obstetric complications that have been published in this type of patient will be reduced; however, it is only a proposed hypothesis since verification with a more significant number of cases is required.
Regarding the main difference between Strassman's surgery and the one proposed in this work, it is found that, with the first, the closure is performed in two layers without respecting the uterine cavity. In the proposed technique, the closure of the cavities is performed in three layers, considering not to invade the uterine cavity with the innermost suture. With the outermost suture at the level of the serosa, traditionally, in the Strassman technique, 1-0 catgut is used, and in the proposed technique, it is performed with 3-0 prolene with invaginating edges to avoid adhesions.
Possible complications in Strassman surgery can occur due to the invasion of the uterine cavity, generating adhesions, compromising the patients' reproductive future. In the proposed surgery, not entering the endometrial cavity considerably reduces the probability of forming adhesions at this level; therefore, the impact on the reproductive future is less. Regarding bleeding, Strassman's surgery presents a greater possibility of bleeding due to resections of broader tissue at the uterine level. With the microsurgical technique, dissections try to avoid bleeding when incisions are made at the tissue level.
Complications may occur more frequently in Strassman surgery due to the use of closure elements since they favor a greater inflammatory process, the production of adhesions and infections that can obliterate the cavity during recovery. Among the complications that can occur with our technique are infections. Although it is considered less likely because less damage is generated at the tissue level, it avoids hypoxia in it, in addition to the fact that materials that offer less inflammatory reaction are used like monofilament. Regarding the surgical time, the microsurgical technique may have a slightly longer duration than the classic Strassman technique; however, in our experience, it is not a significantly longer time.
Finally, this technique must be performed by highly experienced surgeons in the field of microsurgery with certified training in this area, which allows achieving the objectives when proposing this procedure; because tissue management techniques, the use of inadequate sutures, blood loss, in addition to tissue hypoxia, are fundamental factors for success or the appearance of complications.
Because, in most cases, the patients are minors, it is essential to make it clear, within the informed consent and to their parents, that the primary objective of the surgery is to restore the anatomical alteration of the uterus, whose main and immediate benefit it is the disappearance of pain, as has happened very well in the cases presented here. It is also important to emphasize that the secondary benefit may be in the future when they wish to become pregnant since this technique could improve the reproductive capacity of patients.
Finally, we consider essential the combination of endoscopic surgery, hysteroscopy type and abdominal approach (microsurgical procedures), to precisely define the reconstructive procedure to be performed and to be able to have the expected success; in addition, with the appropriate use of prophylactic antibiotics during the procedure due to the inherent risk of infection, attributed to the approaches.











 text in
text in 




