Remark
| 1) Why was this study conducted? |
| To estimate gastric cancer survival in the Colombian population notified to the National Cancer Information System (NCIS) that received health services within the framework of the national health system. To compare these results with those obtained by a population-based cancer registry. |
| 2) What were the most relevant results of the study? |
| People with insurance paid by the government have lower gastric cancer survival than those affiliated with the third payer and the special insurance. The Colombian National Cancer Information System (NCIS) obtained gastric cancer survival estimates higher than those of the population-based cancer registry. Gastric cancer survival in Colombia has a gap of at least 40 percentage points compared to countries that perform population-based screening |
| 3) What do these results contribute? |
| The Colombian government can use survival indicators to monitor the gastric cancer control plan. |
Introduction
Stomach cancer is among the most frequent and lethal types of cancer worldwide. By 2020, it was the fifth type in terms of incidence, and every year accounts for more than 1.1 million and 0.8 million new cases and deaths, respectively 1,2.
Stomach cancer is the leading cause of specific mortality in Colombia and Andean low-middle income countries in Latin America, where gastric cancer incidence rates are higher than those observed in high-income countries 3. Although the stomach cancer burden of morbidity and mortality has steadily decreased in the last decades, its survival remains the lowest compared with other solid tumors such as breast, prostate, or cervical 4.
Survival is one of the most interesting indicators for cancer surveillance and control because it reflects the effectiveness of prevention and treatment. Associated factors with stomach cancer survival are diverse; and could be related to the individual, the disease itself, and the health system 5. However, the key prognostic factor is staging at diagnosis, and it depends on a well-organized screening population program. Japan and Korea have significantly improved stomach cancer control through nationwide screening programs that can detect up to 70% of new cases in the early stages 6-8. In Latin America, the screening coverage is poor, with low cost-effectiveness of the implemented programs 5,9-11; and about 90% of people are diagnosed in advanced stages.
Colombia has a situation comparable to Latin America, lacking a nationwide stomach cancer screening program despite its epidemiologic and economic burden; as well as a high prevalence of Helicobacter pylori infection, which represents a major risk factor for stomach cancer 12. According to the High-Cost Diseases Fund (CAC in Spanish), 73% of the new cases that received care within the framework of the national health system in 2019 were diagnosed in advanced stages 13.
The National Cancer Information System (NCIS) managed by the CAC collects and analyzes demographic, clinical, and administrative information on people with cancer in Colombia through the annual report of 134 variables. The NCIS methodology and scope have been published elsewhere 14.
The NCIS survival estimates are a metric of the effectiveness of cancer care providers and insurers in the Colombian health system that report cancer cases to the NCIS. On the other hand, the Population-based cancer survival provides an indicator of the overall effectiveness of the health care system to deliver screening, early diagnosis, and evidenced-based treatment services and follow-up care to all individuals in the population. The survival estimates of both information systems are complementary, so they could serve as a mutual verification method 15,16.
Therefore, we aimed to estimate 3-year net survival at the national level in people treated within the framework of the national health system during the period 2015-2019, with data from NCIS managed by the CAC; and 5-year net survival in Cali from the Population-based Cancer Registry of Cali (RPCC in Spanish) during the period 1998-2017.
Materials and Methods
Setting
Colombia, a middle-income country, has a population of 50.6 million and a gross national income per capita of U.S. $6,510 17. In 1994, it was established the current health insurance system, which is considered public-private 18. It is a universal and mandatory system that covers almost 96% of the total population. There are two insurance sources; the first is funded by the third payer, and groups the country's workforce; in the remaining cases, the state resources support the second, including the unemployed. The third payer and state insurance cover approximately 45% and 49% of the insured population. The remaining population is under private insurance, in addition to the third payer or government insurance (police, military forces, or government employees) 19.
Cali is the third-largest city in Colombia and the most densely populated in the country's southwest, with 20% of the Colombian population. According to the 2018 census, Cali had 2.2 million inhabitants, 53.2% of which were women, and 26.2% were self-reported as afro-descendants 20. The average life expectancy at birth was 74.4 years 20. Cali has more than 165 enabled oncology services in urban areas 21, but only five centers have integrative oncology services. More than 9.5 thousand new cancer cases were diagnosed in 2019, 55% of whom lived outside Cali.
Data sources
NCIS
The NCIS, administered by the CAC, performed survival analysis on real-world and nationwide data. The NCIS is a passive and non-public registry created by the Colombian Ministry of Health in 2014 22. Its goal is to collect and analyze demographic and clinical information on people who receive health services within the national health system through the annual report of 134 variables. The national health system insures 98% of the Colombian population, and health insurers and providers must report all cancer cases to the NCIS 19. This information system can provide reliable information on real-life trends in access to health care for common types of cancer in Colombia, including identifying barriers to adequate access to treatment. To identify and protect the personal information of the participants, they have created unique identifiers. Data is updated for prevalent cases yearly, while new cancer cases are fully registered. A well-established data monitoring process guarantees information quality, which is carried out in two steps: a prior identification of mistakes in the reporting process through a systematized algorithm. Then, the reported information is audited and compared with clinical health records to ensure accuracy for all new cases. The NCIS methods and scope have been previously described 14. In 2019, the proportion of data quality was up to 83%, and it has increased throughout the years, consolidating the NCIS as a reliable data source.
The Population-based Cancer Registry of Cali (RPCC)
The RPCC has operated continuously since 1962. The official censuses carried out by the National Department of Statistics (DANE) in 1964, 1973, 1983, 1993, and 2005 provide information on the population of Cali 19,23.
The RPCC includes the new cases of stomach cancer throughout notification and active searching in primary data sources, including hospitals, clinics, pathology laboratories, and cancer centers. General mortality by age, sex, and calendar year is periodically obtained from death certificates from the Secretary of Health in Cali. The RPCC integrates the data into the database following the international standards of good practice 24,25. The RPCC is a certified member of the International Association of Cancer Registries and meets the international standards of quality recommended by the International Agency for Research on Cancer (IARC) 24,25. Elsewhere is a complete review of history, goals, logistics, coverage, procedures, and methods for incidence, mortality, and survival estimations 21,26.
Patient selection
NCIS
Case definition. The NCIS included all the new cases of a primary stomach cancer in people aged ≥15 years and reported between January 2nd, 2014, and January 1st, 2019. Health providers confirmed the diagnosis on medical records through a data monitoring process. The International Classification of Diseases 10th edition (ICD-10) 27 defined the location (C160-C169) of the tumor. For net survival analysis, NCIS applied additional exclusion criteria. Cases with a time from diagnosis to death or last contact of unknown length or “0” years, as well as a follow-up time higher than the maximum (3 years), were excluded. Patients with tumors classified as in-situ were also excluded. Information regarding death was reported to the CAC by health insurers. In addition, the deaths were verified by external sources from the Ministry of Health and the National Registry of Civil Status.
RPCC
Case definition. Men and women aged 15-99 years old, residing in the urban area of Cali, with a diagnosis of primary malignant neoplasm of the stomach, codified as C16 according to the Classification of Diseases for Oncology 3rd edition (ICD-O-3) 28, no matter if it was confirmed or partially or fully treated; and registered in the RPCC from 1998 to 2017. The basis for the diagnosis can be microscopic (fluid cytology, bone marrow, histology of a primary tumor and autopsy); and non-microscopic (clinical, surgical, and imaging diagnosis). Cases that have come to the city for treatment or diagnosis are not considered as residing in Cali 15.
The RPCC updated the vital status and date of the last contact by crossing with external sources: the mortality database of the Secretary of Public Health in Cali, the registry of hospital discharges from medium and high complexity healthcare institutions, pathology reports, and insurance databases (public and private).
Full follow-up. People who die before or on the same follow-up closing date, o people who die after the follow-up closing date; or people who are alive and the date of the last contact is greater than the closing date of the follow-up.
Incomplete follow-up. People who are alive, and the date of the last contact is less than the closing date of the follow-up.
Cases with the following conditions were excluded from the analysis: i) cancer diagnosis only based on death certificates, showing the same date for both diagnosis and death, and ii) other causes: unknown age or sex and benign tumors. In the supplementary Table, S1 has summarized the quality indicators for cases.
Statistical Analyses
NCIS
We performed a descriptive analysis of demographic and clinical variables at baseline, including age at diagnosis, sex, health insurance, region of residence, and clinical stage. According to their distribution, continuous variables were reported as medians and interquartile ranges (IQR), while categorical data were summarized as absolute variables and proportions.
In all analyses, the dependent variable was the time between diagnosis and death for any cause or being censored. It was set to a maximum of 3 years. People who did not have the event or were lost to follow-up were censored. 3-year overall survival was estimated using the Kaplan-Meier method, while net survival was calculated through the Pohar-Perme estimator 29. Life tables for all-cause mortality in the general Colombian population were built to estimate expected net survival. The period approach was used because the established follow-up was unavailable for all patients. We also analyzed overall survival and net survival by sex, health insurance, region of residence, and stage at diagnosis, comparing the curves with the log-rank test and the method developed by Pavlič and Perme (log-rank type test) 30, respectively. Net survival was age-standardized using a traditional direct method with an internal standard.
We also estimated a flexible parametric model with restricted cubic spline functions for modeling non-linear and time-dependent effects on the log excess hazard scale proposed by Royston-Parmar 30-33. A generalized linear model using a Poisson assumption with smoothing splines was selected because it violated the proportional hazards principle. To determine the model's complexity and goodness of fit, the Akaike information criterion was evaluated 33.
The final model had 4 knots and 5 degrees of freedom. It was adjusted by age and stage at diagnosis, sex, health insurance, and region of residence, and the results are presented as hazard ratios (H.R.s) and their 95% confidence interval.
RPCC
The dependent variable was the time of follow-up between cancer diagnosis and the event of interest (death by any cause) or being censored. The maximum observation time until the occurrence of the event was five years. Censoring was defined as loss of follow-up and cases without the event at the end of the study period (December 31st, 2018).
The 20-year survival was estimated by combining the cohort analysis approach for the periods 1998-2002, 2003-2007, and 2008-2012, and the period analysis for the interval 2013-2017 due to the lack of complete five-year follow-up information for all subjects 34,35. 5-year net survival was calculated by using the Pohar-Perme estimator 29. Life tables for all-cause mortality in the general population in Cali were built from the number of deaths and population by age, sex and calendar year 35,36. Survival estimations were age-standardized using the international cancer survival standard weights (group 1) 37.
Ethical considerations
NCIS
This study has no risk for participants. Information was collected and analyzed following international standards (The Declaration of Helsinki, The Belmont Report, and The International Guidelines prepared by the Council for International Organizations of Medical Sciences (CIOMS)), as well as national regulations (Resolution 8430 of 1993, stated by The Colombian Health Ministry) for conducting human research. Confidentiality was guaranteed throughout the information processing (reporting, managing, analysis, and publication). All records were anonymized before the analysis. Furthermore, access to data was restricted to the research team and the results only can be used for approved research or academic purposes.
RPCC
The RPCC follows the European Network of Cancer Registries (ENCR) guidelines 38. The director of the RPCC is responsible for security data and confidentiality. Team members of the RPCC sign an agreement for maintaining data confidentiality and privacy of personal information. Access to the RPCC installations is restricted only for authorized personal. Confidential information is accessed by security passwords, closed files, and the destruction of supports with personal identification when they are no longer useful. Only the manager of the RPCC is authorized to perform the initial matching for detecting new cases and updating vital status and last contact information. Each case is identified with an internal I.D. assigned by the RPCC and all datasets are anonymized for statistical analysis.
This research study was approved by the institutional ethics committee of the Universidad del Valle as stated in the approval certificate number 001-020 dated January 2020.
Results
NCIS
Demographic and clinical characteristics at baseline
A total of 8,549 people reported from 2015 to 2019 met the inclusion criteria and were analyzed. Demographic and clinical characteristics of new cases of stomach cancer at baseline are shown in Table 1. Most cases occurred in men above 50 years, affiliated with the third payer insurance, living in the Central Region, and diagnosed in advanced stages.
Table 1 Age-standardized baseline demographic and clinical characteristics of people with stomach cancer within the Colombian health system, 2015-2019
| Variable ‡ | New cases (n=8,549) |
|---|---|
| Age at diagnosis (years) | 65 (54-74) |
| Age groups | |
| 15-19 | 6 (0.1) |
| 20-24 | 36 (0.4) |
| 25-29 | 95 (1.1) |
| 30-34 | 184 (2.1) |
| 35-39 | 264 (3.1) |
| 40-44 | 374 (4.4) |
| 45-49 | 619 (7.2) |
| 50-54 | 868 (10.2) |
| 55-59 | 969 (11.3) |
| 60-64 | 1,061 (12.4) |
| 65-69 | 1,111 (13.0) |
| 70-74 | 1,044 (12.2) |
| 75-79 | 930 (10.9) |
| 80 and more | 986 (11.6) |
| Sex | |
| Males | 5,226 (61.1) |
| Females | 3,323 (38.9) |
| Stage at diagnosis † | |
| Early | 1,442 (16.9) |
| Advanced | 4,709 (55.1) |
| Unknown | 2,398 (28.0) |
| Health insurance | |
| Third payer | 4,844 (56.6) |
| Paid by the state | 3,459 (40.5) |
| Exception | 79 (0.9) |
| Private | 57 (0.7) |
| Uninsured | 110 (1.3) |
| Geographical region of residence § | |
| Bogotá, D.C. | 2,111 (24.7) |
| Caribbean | 450 (5.3) |
| Central | 2,852 (33.3) |
| Eastern | 1,371 (16.0) |
| Pacific | 1,649 (19.3) |
| Other provinces | 116 (1.4) |
‡ Values are absolute numbers (%). Age is reported as median (interquartile range).
† Stages IA, I.B., IIA and IIB were grouped as early. Advanced stage includes IIIA, IIIB, IIIC and IV.
§ Colombian provinces are grouped in six regions, according to their gross domestic product by the Department of National Statistics (DANE in Spanish) as follows: 1) Bogotá, D.C (country's capital); 2) Caribbean (Atlántico, Bolívar, Cesar, Córdoba, La Guajira, Magdalena and Sucre); 3) Central (Antioquia, Caldas, Caquetá, Huila, Quindío, Risaralda and Tolima); 4) Eastern (Boyacá, Cundinamarca, Meta, Norte de Santander and Santander); 5) Pacific (Cauca, Chocó, Nariño and Valle del Cauca); 6) Other provinces (Amazonas, Arauca, Casanare, Guainía, Guaviare, Putumayo, San Andrés, Vaupés and Vichada).
Survival analysis
All participants contributed a total of 9,317 years, and 4,478 deaths were observed. The Median follow-up time was 0.8 years (min: 0.2 years, max: 3.0 years). 3-year net survival was 36.8% (95% CI: 35.5-38.1). Net survival at 1 and 2 years was 55.8% (95% CI: 54.7-56.9) and 41.2% (95% CI: 39.9-42.4), respectively.
We also estimated net survival by sex, age, health insurance, stage and region of residence at diagnosis. Regarding health insurance (Figure 1), net survival was significantly higher in people affiliated to special insurance (61.7%; 95% CI: 44.8-74.8) or to the third payer (40.5%; 95% CI: 38.7-42.3) in those affiliated to state insurance (30.7%; 95% CI: 28.7-32.8) (log-rank type p < 0.001). Figure 2 shows that net survival was significantly higher in women (42.6%; 95% CI: 40.2-44.9) than men (34.8%; 95% CI: 33.1-36.5) (log-rank type p < 0.001).

Figure 1 Colombia. Three-year net survival standardized by age according to health insurance in people diagnosed and treated with stomach cancer..

Figure 2 Colombia. Three-year net survival standardized by age according to sex in people diagnosed and treated for stomach cancer.
On the other hand, net survival was significantly higher in people diagnosed at early stages (IA, IB, IIA, IIB) (58.1%; 95% CI: 54.5-61.5), compared with those at advanced stages (25.1%; 95% CI: 23.4-26.9) (log-rank type p < 0.001) (supplementary Figure S1). Net survival was also significantly higher in people aged <60 years (33.9%; 95% CI: 31.9-36.0), compared with those aged ≥60 years (38.4%; 95% CI: 36.7-40.1) (log-rank type p < 0.001).
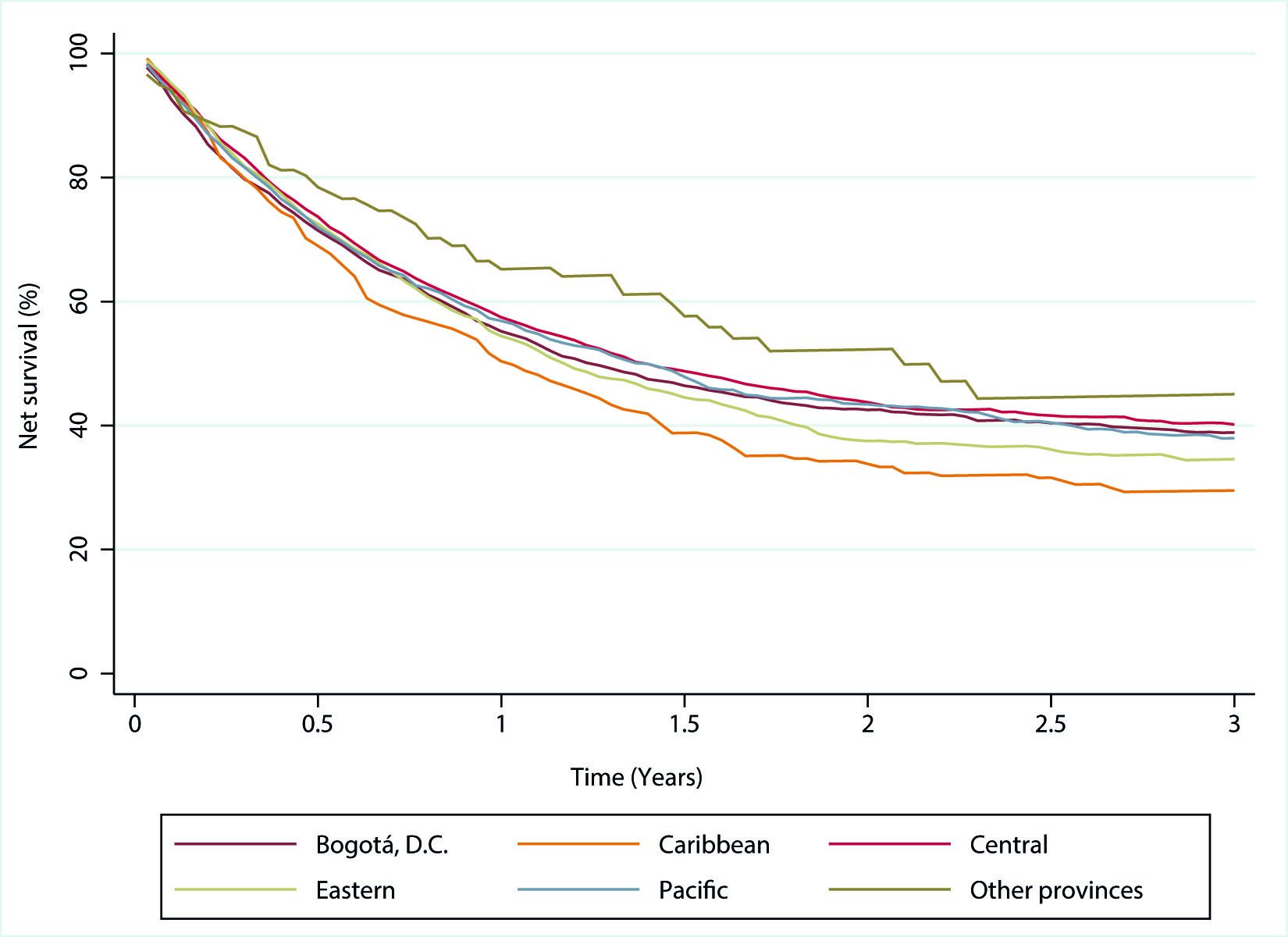
Supplementary Figure S2 shows net survival by region of residence at diagnosis. There were no statistically significant differences, except for people living in the Caribbean region (29.4%; 95% CI: 24.0-35.0), who had a significantly lower net survival than those in the Central region (38.5%; 95% CI: 36.2-40.8).
Flexible parametric model results
Overall, people under state insurance were at a higher risk of death those affiliated to the third payer (adjusted HR=1.2, 95% CI: 1.1-1.3; p <0.001). Otherwise, people with special insurance had a significantly lower risk (adjusted HR=0.6, 95% CI: 0.4-0.9; p= 0.022). Regarding sex, men had a significantly higher risk of death than women (adjusted HR=1.2, 95% CI: 1.1-1.2; p <0.001). Furthermore, people diagnosed at early stages had a lower risk of death than those with unknown staging (adjusted HR=0.6, 95% CI: 0.5-0.7; p <0.001). The age-stratified model showed a higher risk in men aged ≥60 years. Furthermore, older people with state insurance risk was also higher than younger people. The effect of early detection remained the same despite age (Table 2).
Table 2 Multivariable-adjusted hazard ratios in people with stomach cancer treated within the Colombian health system
| Variables § | Aged <60 years | Aged ≥60 years | ||||
|---|---|---|---|---|---|---|
| (n= 3,212) | (n=5,335) | |||||
| HR-adjusted | 95% CI | p-value | HR-adjusted | 95% CI | p-value | |
| Sex | ||||||
| Females (reference) | 1.0 | - | - | 1.0 | - | - |
| Males | 1.1 | 0.9-1.2 | 0.209 | 1.2 | 1.1-1.3 | <0.001 |
| Health insurance | ||||||
| Third payer (reference) | 1.0 | - | - | 1.0 | - | - |
| Paid by the state | 1.1 | 0.9-1.2 | 0.335 | 1.3 | 1.2-1.4 | <0.001 |
| Exception | 0.7 | 0.4-1.2 | 0.187 | 0.9 | 0.6-1.3 | 0.646 |
| Special | 0.5 | 0.2-0.9 | 0.036 | 0.7 | 0.4-1.3 | 0.220 |
| Uninsured | 1.0 | 0.7-1.5 | 0.915 | 0.9 | 0.6-1.4 | 0.660 |
| Stage at diagnosis | ||||||
| Unknown (reference) | 1.0 | - | - | 1.0 | - | - |
| Early | 0.6 | 0.5-0.7 | <0.001 | 0.6 | 0.5-0.7 | <0.001 |
| Advanced | 1.5 | 1.4-1.7 | <0.001 | 1.4 | 1.3-1.5 | <0.001 |
| Geographical region of residence | ||||||
| Bogotá, D.C. (reference) | 1.0 | - | - | 1.0 | - | - |
| Caribbean | 1.2 | 0.9-1.5 | 0.061 | 0.9 | 0.8-1.1 | 0.616 |
| Central | 0.9 | 0.8-1.1 | 0.742 | 0.8 | 0.7-0.9 | <0.001 |
| Eastern | 0.9 | 0.8-1.1 | 0.388 | 0.9 | 0.8-1.1 | 0.747 |
| Pacific | 1.1 | 0.9-1.2 | 0.866 | 0.9 | 0.8-0.9 | 0.027 |
| Other provinces | 0.6 | 0.4-0.9 | 0.048 | 0.6 | 0.4-0.9 | 0.024 |
§ All variables were measured at diagnosis.
H.R.: hazard ratio, CI: confidence interval.
RPCC
Six thousand seven hundred seventy-six people diagnosed with stomach cancer, living in Cali, and registered in the RPCC database between 1998 and 2019, aged between 15 and 99 years, were included in survival analysis (42.4% were women). Otherwise, 687 cases (9.2%) were excluded (25,26). During the period 2013-2017, 83.3% of cases were morphologically verified, and 2.7% had a death certificate as the only evidence for cancer diagnosis.
Table 3 shows 1, 3, and 5-year net survival for both sexes of people with stomach cancer between 1998 and 2019. In the last decade (2008-2017), 5-year net survival was close to 21% being, significantly higher than the previous decade (1998-2007). Furthermore, in the last quinquennium, it improved by 4.7 percentage points that representing an increase of 25% compared with the first quinquennium (21.3% (95 CI%: 19.2-23.6) vs. 16.6% (95% CI: 19.2-23.6)).
Table 3 Cali, Colombia. Age-standardized net survival at 1, 3 and 5 years in adults (15-99 years) diagnosed with stomach tumors, by calendar period (both genders).
| Period of diagnosis | Net Survival § | |||||
|---|---|---|---|---|---|---|
| 1 year | 95% CI | 3 years | 95% CI | 5 years | 95% CI | |
| 1998-2002 | 32.1 | 29.8 - 34.3 | 18.8 | 16.7 -21.1 | 16.6 | 14.5 -18.9 |
| 2003-2007 | 35.1 | 33.0 - 37.1 | 21.0 | 19.1 - 23.1 | 18.7 | 16.7 -20.9 |
| 2008-2012 | 39.4 | 37.2 - 41.5 | 22.7 | 20.7 - 24.8 | 21.0 | 18.9 - 23.2 |
| 2013-2017 | 43.8 | 41.4 - 46.0 | 23.8 | 21.7 - 25.9 | 21.3 | 19.2 - 23.6 |
§ Values are percentages.
CI: confidence interval.
5-year net survival by sex is described in Table 4. In men, it remained stable during the last 20 years; while in women, it significantly improved in the last decade, showing an increase of 50% (8.6 percentage points) in the previous quinquennium compared with the first one (24.8% (95% CI: 20.4-29.3) vs. 16.2% (95% CI: 13.1-19.7)).
Table 4 Cali, Colombia. Age-standardized net survival at 5 years in adults (15-99 years) diagnosed with stomach tumors, by sex and calendar period.
| Period of diagnosis | Male | Female | Both | |||
|---|---|---|---|---|---|---|
| NS§ | 95% CI | NS § | 95% CI | NS§ | 95% CI | |
| 1998-2002 | 17.2 | 14.3 - 20.4 | 16.2 | 13.1 -19.7 | 16.6 | 14.5 -18.9 |
| 2003-2007 | 18.5 | 15.8 - 21.5 | 19.2 | 16.2 -22.4 | 18.7 | 16.7 -20.9 |
| 2008-2012 | 19.1 | 16.4 - 21.9 | 24.0 | 20.4 -27.8 | 21.0 | 18.9 - 23.2 |
| 2013-2017 | 19.1 | 16.2 - 22.2 | 24.8 | 20.4 -29.3 | 21.3 | 19.2 - 23.6 |
§ Values are percentages.
NS: net survival; CI: confidence interval.
Supplementary Table S1 shows that about 63% of people diagnosed with stomach cancer died during the first year of follow-up.
Discussion
The NCIS provides nationwide stomach cancer data; this survival analysis was performed with Observational Routinely collected health Data (RECORD). In addition, the Cali population-based Cancer Registry, one of the oldest in Latin America, compared these survival estimates at the national level with those calculated by its team for the city of Cali.
Population-based cancer survival reflects the overall effectiveness of the health system for cancer control. It measures the mean survival achieved by all patients with stomach cancer despite their demographic and clinical conditions. Survival is the primary goal in the care of patients with stomach cancer. Early detection of stomach cancer and radical surgery associated with adjuvant treatments are the driving force behind stomach cancer control 39.
Stomach cancer is a multifactorial disease mainly related to Helicobacter pylori gastritis, which usually begins early. Environmental, infectious and host-related factors may interact to develop the disease. During the last half-century, stomach cancer incidence and mortality rates have significantly decreased worldwide. It is associated with the lower use of salt in processed food and the greater availability of fresh fruits and vegetables. In many countries, tobacco use and the prevalence of H. pylori infection have also decreased 40,41.
Unfortunately, advances in the treatment of stomach cancer are insufficient, there is no vaccine development against H. pylori, and early detection programs in Latin America have not been successful due to a lack of continuity and low-cost effectiveness. Chemoprevention remains an option for stomach cancer control as a primary prevention strategy to eradicate H. pylori infection 9,10.
Regarding our analysis, the CAC gathers a large volume of RECORD data by an interconnection platform that allows the flow of cancer data in real-time between health insurers and providers 42. On the other hand, the RPCC was established in 1962; it is a population-based cancer registry that provides continuous information on new cases of all types of cancer in permanent residents of Cali through active search and notification 21, 26. For stomach cancer survival analysis, these two information systems, CAC and RPCC, have comparable variables for the person, tumor, vital status, and date of the last contact. Unfortunately, there is a limitation to obtaining information about staging.
The 3-year net survival was 36.8% (95% CI: 35.5-38.1), according to the NCIS. In the flexible parametric model, we found that people with insurance paid by the state had a significantly higher risk of death than those affiliated to the third payer and the special insurance. The mortality risk was also significantly higher in men than women; and in people diagnosed at advanced stages. When analyzing data from the RPCC, the 5-year net survival during the period 2013-2017 was 21.3%. In addition, we observed it was almost stable in men; while in women, it significantly improved in the last decade and, in the previous quinquennium, it showed an increase of 50% compared with the first one.
Stomach cancer survival from the RPCC was higher than observed in other Latin American countries such as Ecuador and Chile (19.1% and 16.7%, respectively) while were lower than estimated in Costa Rica (40.0%) during the period 2010-2014 22 (Supplementary Table S2). The above suggests that stomach cancer continues to have a high social burden in Cali and Colombia, being the major cause of cancer deaths 26,43.
In most countries, advances in surgical and multimodality treatments and post-operative care have only modestly improved survival and prognosis. South Korea and Japan have well-established national stomach cancer prevention and screening programs 2,44 with 5-year net survival of 69% and 60% (Supplementary Table S2),respectively, with an average increase between 10% and 20% in the last 20 years according to CONCORD-3 35. In those countries, strategies have been focused on eradicatingH. pyloriand the early detection of cancer by population-based endoscopic screening programs.
CONCORD-3 results also highlighted that survival increased up to 5% in five European countries (Denmark, Lithuania, and the United Kingdom in North Europe, Poland in Eastern Europe and Austria in western Europe), with 5-year net survival ranging from 20% to 27%. In the United States and Austria, survival estimations ranged from 30% to 35% during the period 2010-2014 35.
When comparing survival in Japan or Korea with the estimations reported in the United States, the overall difference is due to earlier diagnosis, fewer proximal and gastroesophageal junction lesions, and histologic or genetic variations in Asian countries 45,46. Self-selection bias and lead-time bias could overestimate the survival gap between countries. Healthy or health-conscious individuals may overrepresent participants in screening programs, and ever-screened patients may seem to be surviving longer because they are diagnosed earlier, not screening-test effect. It could lead to an overestimation of the effectiveness of the screening program. Western countries such as Colombia have no population-based screening programs for stomach cancer 47.
Results from both the NCIS and the RPCC are consistent regarding better survival in women than men. In contrast, in Japan, women show a small but consistently lower survival associated with more advanced stages among women. It suggests a gender inequity in screening, medical examinations, or treatment for stomach cancer in Japan 48. Our findings show that gender inequity in Colombia goes in the opposite direction.
One of the most important findings from the NCIS analysis was the statistically significant differences in the risk of death by health insurance, with better outcomes in people affiliated with the third payer or special insurance than those insured by the state. Our results are consistent with a study performed with data from a population-based registry in Manizales, Colombia. People affiliated with the third payer had about 30% lower risk of dying than people with state insurance 49. In both cases, insurance could be a proxy of access and health care quality. It would also represent the distribution of exogenous sociodemographic factors related to risk awareness and a timely diagnosis and treatment 50. Despite the increase in coverage from 2010, there is differential access to health care according to the insurance system, and inequities in cancer diagnosis and treatment persist even between types of insurance 49.
Finally, it is worth mentioning that our results are valuable for improving cancer planning and strengthening national information systems on cancer and population registries. Furthermore, results from both approaches allow identifying gaps in the reporting process of cancer cases that receive care within the national health system. Regardless of differences in their methodology and scope, the NCIS and RPCC information may be complementary to identify cancer burden in terms of its frequency, distribution at demographic and insurance levels, as well as barriers for adequate access to health care and outcomes of cancer management performed by insurers and providers such as survival.
Prevention will always be preferable to cure, especially for gastric cancer with high lethality. Unfortunately, there is no vaccine development against H. pylori, and early detection programs in Latin America have not been successful. Therefore, chemoprevention remains an option for stomach cancer control as a primary prevention strategy to eradicate H. pylori infection.
However, cancer treatment costs are increasing and creating financial hardship in providing high-quality cancer care equally to all citizens. The evidence from this research suggests that there is inequality in gastric cancer care in the current Colombian health system. People with insurance paid by the government have lower survival than those affiliated with the third payer and the special insurance. Decision-makers in the Colombian government, insurance companies, and hospitals that provide cancer care in the Colombian health system must introduce policy changes to reduce existing gaps. It is unacceptable that there is political tolerance of inequality in access to affordable cancer care 16.
Strengths and limitations
Our study's main strength was exploring stomach cancer survival from two different but complementary data sources. Data from the NCIS provides a real-world approach from an insurance perspective at the national level, while the RPCC is population-based. Also, data from the NCIS was fully validated by a well-established and systematic data monitoring process. Regarding deaths, the official source of the Ministry of Health confirms that they are exhaustively validated 14.
On the other hand, population-based survival estimates by the RPCC reflect all patients with stomach cancer in Cali, regardless of socioeconomic status and disease characteristics. In addition, the RPCC follows the CONCORD-3 guidelines for the standardization, cleaning, and construction of quality indicators. This process facilitates a specific exclusion of cases from the study and allows a uniform coding format for the mandatory variables 16,35.
There is a limitation regarding the comparability of survival estimates obtained by the RPCC and the CAC due to their different definition of the stomach cancer case 21,51. The RPCC includes invasive stomach cancer cases, regardless of whether they have been confirmed or partially, or fully treated. The basis of the diagnosis can be both morphological; as non-morphological. For the 2013-2017 period, 83.3% of stomach cancer cases had morphological verification. In 14%, the diagnosis was clinical, and in 2.7%, the cancer cases were registered from the death certificate only 52.
In contrast, Colombian health insurers notify the CAC of stomach cancer cases with morphological or clinical confirmation treated in the framework of the national health system. Although notification of stomach cancer cases to the CAC is mandatory, it does not guarantee the completeness and could limit the comparability of our findings 14,51.
Due to the above, the NCIS information could underestimate cancer incidence rates and overestimate survival compared to those obtained by the RPCC. In addition, the quality of notification of cancer cases is related to the organization of cancer services, which influences the clinical outcomes of cancer.
The RPCC does not have information on tumor stages in patients with stomach cancer. The RPCC passively follows up to obtain the vital status of the patient and the date of the last contact. The RPCC periodically updates the vital status with the Secretary of Health in Cali, but the linkage with the national databases is insufficient and depends on death certificates that have inherent inaccuracies and missing data. Furthermore, Cali does not have a census of the migratory flows of the population and lacks life tables by socioeconomic stratum and by the state of insurance to the national health system.
Final comments
The RPCC and CAC regularly conduct cancer situational analyses and are essential to monitor and evaluate national and regional progress in stomach cancer surveillance and control. Collaboration between reporting systems and cancer registries enables these complementary systems to verify survival estimates to identify gaps, implement standards, and develop improvement plans to ensure data quality.
The standardization of the data allows regional and international comparisons and facilitates decision-making. It is a priority to unify the case definition and for the CAC to work with the cancer registries to complement the incidence and survival information and achieve the link with the national databases to improve the passive follow-up process.











 text in
text in