Introduction
Trigeminal neuralgia, also called "Tic douloureux", is one of the worst ailments a human being can experience. This condition is defined as a sudden severe, usually unilateral, brief, shooting pain occurring in the distribution of one or more branches of the trigeminal nerve 1. Also described as "whiplashes” that are triggered in the face in bursts of seconds, triggered by touching the face or scalp and in situations such as chewing, brushing teeth, talking, and even applying makeup 2.
Its worldwide incidence varies, but it is estimated at 1 per 5,500 people 3, at the same time, it is estimated that three-quarters of patients with trigeminal neuralgia are over 50 years old 4. Most cases respond favorably to the use of antiepileptic drugs such as carbamazepine and derivatives, depending on the level of pain, the use of double medication is justified. In approximately 12% of cases, medication is insufficient to relieve pain or the adverse effects are greater than the therapeutic benefit, and surgical options should be considered 2,5. At present, microvascular decompression remains the preferred intervention for trigeminal neuralgia 6, possibly due to its high effectiveness of 80-90% for pain relief 6-9.
The surgical options available in Latin America can be divided into three large groups 10: open microsurgery such as: neurovascular decompression; percutaneous procedures such as: Rhizotomy, percutaneous Rhizolysis with glycerol, Gasser's ganglion stimulation with neuromodulation and percutaneous microcompression; finally, radiosurgery such as radiofrequency thermocoagulation 3,6. A current proposal is CyberKnife radiosurgery for refractory patients 11-14. Radiosurgery consists of the application of radiation measured in grays (Gy) capable of causing a controlled lesion in dosage and localization in millimeter ranges of precision generally assisted by a stereotaxic frame. Likewise, CyberKnife consists of a linear accelerator mounted on a robotic arm, which through the processing of computerized images and a real-time image obtained by two radio diagnostic tubes installed on the ceiling of the operating room, avoids the need for an invasive stereotaxic frame, allowing guiding X-ray beams in megavoltage range with a precision of up to 1 mm (accelerating electrons up to kinetic energies between 4 and 25 MeV), causing tissue changes such as axonal degeneration and necrosis, which, in the case of trigeminal neuralgia, leads to occlusion of vessels in aberrant arteriovenous loops compressing the trigeminal nerve root (Figure 1) 15, such compressions by arteriovenous loops are the cause of trigeminal neuralgia in 80-90% of cases 16.
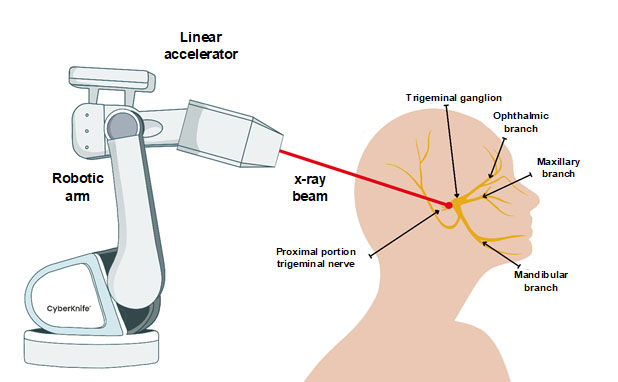
Figure 1 Principle of CyberKnife radiofrequency robotic surgery. The linear accelerator of the robotic arm is guided by 2 radio diagnostic tubes mounted on the ceiling of the operating room to produce a 70-90 Gy photon beam aimed at the proximal trigeminal root to cause vessel occlusion in the aberrant arteriovenous loops compressing the trigeminal nerve root.
Clinical case
Female patient, 37 years old, Colombian, medical professional, who since the age of 13 years suffered from paresthesias and twinges in the right nasal ala and ipsilateral cheek, appearing intermittently for several seconds in new facial and intraoral trigger points, becoming disabling to eat, talk, laugh, and every day increased in duration. She was diagnosed at 16 years of age with trigeminal neuralgia with an excellent initial response to carbamazepine, which evolved with a low response with pain modulators at maximum tolerated doses, later the patient underwent self-practiced management with acupuncture, soft laser, and multiple peripheral blocks by medical knowledge. At 24 years of age, she underwent right trigeminal microvascular decompression as the first line of surgical intervention, without intraoperative vascular conflict demonstrated by imaging and with transient improvement for one year. Due to the subsequent relapse of the initial pain, the treating neurosurgeon and neurologist indicated a change to Oxcarbazepine at a dose of 1,400-2,400 mg per day and Lamotrigine during pregnancy. At the age of 30 years, she developed trigeminal neuralgia in the left mandibular ramus, establishing bilateral trigeminal neuralgia that affected her quality of life, with more severe crises, triggered spontaneously during sleep and even reaching refractoriness to the peripheral trigeminal block, generating somnolence, depressive mood, and social isolation.
This case was evaluated by neurosurgery service with an emphasis on radiosurgery in different hospitals in the country, where in the medical board of the case, and in accordance with the analysis of the brain magnetic resonance (Figure 2) and the patient's history, it was decided to perform CyberKnife radiosurgery in mono-fraction on the left trigeminal and subsequently treat the contralateral trigeminal.
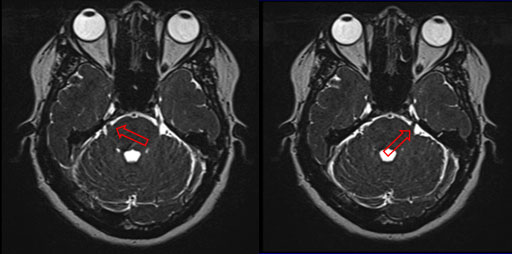
Figure 2 Bilateral trigeminal neuralgia by contrasted brain magnetic resonance. Vascular compression can be seen in both proximal branches of the trigeminal nerve (red arrow).
In 2019, taking the general measures of positioning the patient in a supine position, placing the mask, and comparing the tomography and images in real-time, the patient received the first dose of irradiation by CyberKnife with 70Gy on the left trigeminal with 80% isodose line. There was a total resolution of the left-sided symptomatology and an improvement of pain on the right side. Subsequently, in 2020 she received a second irradiation on the right trigeminal at 60Gy, where two branches were involved (mandibular/maxillary). During the 23-month follow-up, employing telephone calls, the patient developed, as an adverse effect to the procedure, a slight hypoesthesia in the right chin region without clinical significance. The patient reported a satisfactory response from four weeks after the irradiation to date, with only one report of crisis with minimal intensity and spontaneous resolution.
The postoperative results allowed to reduce the doses of Oxcarbamazepine that she had been taking for 5 years until its suspension a few days after the procedure. Finally, a review of the physical examination 6 months after CyberKnife treatment, with an exploration of the fifth cranial nerve revealed intact masticatory motility, good corneal, masseter, and sneezing reflexes, as well as good motor function for chewing and swallowing movements with preserved strength of the dental arches. About the general opinion of the patient, regarding the procedure, she says "It is a simple, low-risk, exact, outpatient treatment that did not generate medical incapacity and was not painful".
Discussion
Trigeminal neuralgia is a syndrome characterized by attacks or unbearable episodes of recurrent, generally acute, intense, unilateral and superficial pain located over the innervated areas of the trigeminal nerve, which has a good response to antiepileptic drugs (Carbamazepine/oxcarbazepine) as usual treatment, however, the chronicity of the disease leads to surgical management. Antagonistically, the probability of post-surgical relapses with an intensity of the original pain and incapacity of the patient in a microvascular decompression is 15-30% 3,7,8,16.
This case was atypical due to the onset of symptoms during adolescence, involvement of several branches, and the rarity of bilateral development, without being associated with a demyelinating disease of the nerve, by magnetic resonance studies or the appearance of other sensory-motor disorders in other body areas. Bilaterality without family history is only described in 5% of all cases 17.
The initial diagnosis of this pathology was based on the clear clinical picture of trigeminal neuralgia; severe or incapacitating paroxysmal pain attacks, shooting type, only localized in the distribution of the trigeminal branches without any neurological deficit and not being better explained by any other pain pathology, indexed in the International Classification of Headache Disorders (ICHD) as atypical or idiopathic persistent easy pain, Tolosa-Hunt syndrome, primary stabbing headache and trigeminal-autonomic headaches 16,18. In addition to its temporary effective response with the use of carbamazepine and lidocaine blocks, which is consistent with the clinical course of trigeminal neuralgia.
However, as occurred in this case, given the chronicity and gradual worsening over time and the intensity of the crises, with the appearance of new areas of the trigeminal nerve affected, pharmacological management by the neurology team was not a valid option over time, despite efficient dosage readjustments. The adverse effects, in addition to pain, suffered by the patient, potentially originated from the pharmacological treatment (2,400 mg of oxcarbazepine daily), among the most common: somnolence, diplopia, dizziness, ataxia, depression of cognitive functions, memory and concentration disorders 10, the above together with the pharmacoresistance of trigeminal neuralgia in 25-50% of patients 10,19 placed in the need for an undertaking of invasive surgical treatments 20, which were performed without the expected pain relief in time, as was the microvascular decompression.
Other options such as Gasser's ganglion neurolysis and rhizotomy were discarded, due to the possibility of less invasive management such as radiosurgery, which in persistent cases of trigeminal neuralgia, are part of the options within the new guidelines 3,11,13,14,16 for having greater effectiveness in eliminating pain 3,6 and less probability of complications such as hypoacusis, facial hypoesthesia, fistula of the cerebrospinal fluid or post-surgical hemorrhage 2. For this reason, with the idea of integrating new alternatives and achieving different results, it was decided to perform radiosurgery by CyberKnife, taking into account other case reports and studies that confirm its benefits 3,11-16,19, in addition to the history of several failed procedures performed on the patient such as acupuncture, exaggerated medication, microvascular decompression and her painful symptomatology that affected the social and mental part.
This is an aspect to take into account in this entity, since a previous history of invasive surgical interventions may diminish the therapeutic efficacy of CyberKnife 11. The expected risk or complication of this treatment is facial numbness in 4.3-12.0% of cases, which can best be described as a side effect positively associated with effective pain relief and directly proportional to the amount of Gy applied 11,13. So far, no mortality has been attributed to CyberKnife in any study, and among other complications found are cerebral edema, radionecrosis, hemiparesis, and dysesthesia 15.
During the 23-month post-procedure telephone follow-up, the patient only reported the appearance of hypoesthesia on the mandibular branch one year after her irradiation, which is one of the few adverse effects described for the procedure, even though she received the correct doses in direct mid-range in the proximal portion of the trigeminal nerve, which did not exceed 75 Gy. As an additional point of CyberKnife, we must remember that the perioperative or postoperative adverse effects decrease drastically with the use of this technology 16, therefore as an important result in this case, it must be emphasized that, although a therapeutic method does not have sufficient support it can be beneficial for a patient, as long as all other resources have been exhausted, the risks, benefits, and limited evidence have been explained to the patient, and there are at least reports or observational studies on its efficacy. With this, we avoid making the mistake of repeating the same methods wishing to obtain different results.
Conclusion
As trigeminal neuralgia is a multidisciplinary pathology (otorhinolaryngology, psychiatry, neurology, neurosurgery, pain physician), it would be crucial to develop criteria for early recognition of refractory cases and thus avoid ineffective interventions, preventable complications and decrease in the quality of life of patients. In this way, new interventions that have demonstrated efficacy, fewer recurrences, and few complications, such as radiosurgery by CyberKnife, could be proposed.











 text in
text in 



