Remark
| 1) Why was this study conducted? |
| The identification of patients at risk of hospital associated functional decline and the early adoption of interventions can prevent its occurrence and complications |
| 2) What were the most relevant results of the study? |
| There is a high prevalence of hospital associated functional decline at the time of discharge (43.6%) and it was associated with older age, longer hospital stay, the presence of delirium, and previous dementia. Interventions such as in-hospital physical therapy are useful for its prevention. The HARP scale underestimated the risk of Hospital associated functional decline for patients in the low and intermediate risk categories, and overestimated the risk for patients in the high-risk category. Both scales showed poor discriminatory capacity." |
| 3) What do these results contribute? |
| HARP and ISAR scales in the Colombian population have limited discriminative ability to predict hospital associated functional decline at discharge and should be used with caution. Hospital associated functional decline, being a frequent event in the elderly population requiring hospitalization, the detection of risk factors and early identification allow for actions to be taken for its prevention. |
Introduction
Older adults admitted to the hospital for acute illness are at higher risk of hospital-associated functional decline (HAFD) during stay and after discharge 1. For example, rent literature shows that three months after discharge, approximately 30% of older people treated for an acute illness lose the ability to perform some activity of daily living held before hospitalization 2. This can result in readmissions, new hospitalization, admission to a nursing home, increased mortality, and greater reliance on health resources 3.
The hospital-associated functional decline (HAFD) has two stages, pre-hospital and intra-hospital. Identifying at-risk patients and adopting early interventions (such as promoting mobility, preventing delirium, and maintaining a good nutritional status) may prevent permanent hospital-associated functional decline and reduce the risk of complications 4.
Several scales aim to identify patients at risk for hospital-associated functional decline 5. The most widely used are Hospital Admission Risk Profile (HARP) 6 and Identification of Seniors at Risk (ISAR) 7. The HARP is a practical, easy-to-apply instrument that stratifies hospital-associated functional decline risk at discharge and for three months in three risk categories: low-, intermediate-, or high- 6. This scale includes age, the Instrumental Activities of Daily Living (IADL), and an abbreviated Folstein Mini-Mental State Examination (MMSE). The ISAR scale detects older adults at risk for adverse clinical outcomes 90 and 180 days after visiting an emergency room. Such adverse results include death, institutionalization, readmission, and hospitalization. Also, ISAR english to has been proposed as a predictor of hospital-associated functional decline after three months of discharge 8. The ISAR classifies patients in low- or high-risk categories using six questions on functional and cognitive deficits, polypharmacy, visual impairment, and previous hospitalizations 7.
Colombia's life expectancy and social support differ significantly from other countries, so these scales need to be validated 9. Therefore, this study assesses the calibration and discriminative abilities of the ISAR and HARP scales as predictors of hospital-associated functional decline at discharge in a cohort of patients managed in a Colombian acute geriatric care unit.
Materials and Methods
The authors designed a study to validate a clinical prediction model (External validation) 10. We evaluated the calibration and discrimination ability of the HARP and ISAR scales to predict hospital-associated functional decline at discharge in a cohort of patients older than age 65 managed at the acute geriatric care unit of the Hospital Universitario San Ignacio in Bogotá D.C., Colombia. Data were collected from patients' clinical records between January 2018 and April 2020. The ethics committee of the Hospital Universitario San Ignacio in Bogota D.C., Colombia, approved this study (act No. 18- 2017).
We reported the study following the recommendations of the PROBAST tool, specifically designed to assess and report studies aimed at designing, validating, or updating prognostic models 11,12.
Participants
The study included patients with a Barthel index measured at admission and discharge. The study excluded patients hospitalized for exacerbated psychiatric conditions, those who requested voluntary discharge, those referred to another institution, and those with a basal high-dependence state at admission (Barthel score <10).
Predictors
We used the scales HARP 6 and ISAR 7 as described in the original studies published by Sager and McCusker, respectively. Without considering ethnicity, comorbidities, and diagnosis at admission
Outcomes
The study defined HAFD as a decrease of five or more points in the Barthel index at discharge compared to the basal score 13. The Barthel index assessed at admission and discharge relied on the 10-item Activities of Daily Living (ADL) questionnaire 14.
On admission, the calculation of IADL relied on the modified Lawton scale. The question: "Can you perform the following activities without help from anyone?"; assessed capabilities for 1) Managing her/his finances; 2) Making daily purchases (especially food); 3) Preparing food; 4) Doing daily home chores; 5) Doing her/his laundry; 6) Managing her/his medications; 7) Using public transportation or a taxi; 8) Using a telephone. Answer options were binary, scoring a 1 when the individual could perform a task alone (with or without difficulty); and 0 when the individual could not perform the task alone. Scores ranged between 0 and 8, with lower scores reflecting a more significant impairment in IADL 15.
The study defined:
Malnutrition, as a Mini-Nutritional Assessment (MNA) Short Form 16 scores under 11 points
Readmission, as any hospital admission within 30 days of discharge
Polypharmacy is the use of five or more medications
Social support, as assessed with a semi-structured interview.
Delirium, defined by the Confusion Assessment Method (CAM) 17
Nosocomial infection is described as any infectious disease acquired during hospitalization
Dementia, as an MMSE scores under 20 points 18.
In-hospital physical therapy is the initiation of therapy during the hospital stay.
Analysis
Comparison between patients with and without hospital-associated functional decline used a Ji 2 test for categorical variables and a Mann-Whitney U test or a t-test, according to the distribution of variables. Validation of scales considered two fundamental aspects: Discriminative abilities and calibration.
Discriminative ability is the capacity of a scoring system to predict different outcomes, in this case, hospital-associated functional decline at discharge. The study used the area under the diagnostic performance curve (c-statistic 19) to assess the discriminative ability of HARP and ISAR.
Calibration measures the correlation between predicted and observed outcomes. The study calibrated both scales by calculating the relation between observed/expected events (ROE) at each initial risk level. Risk levels were low, intermediate, and high for HARP; low and high for ISAR. Calibration also applied the Hosmer-Lemeshow (H.L.) goodness-of-fit test on ten groups of the same size (deciles) 20.
The statistical analysis used the STATA 15.0 program.
Results
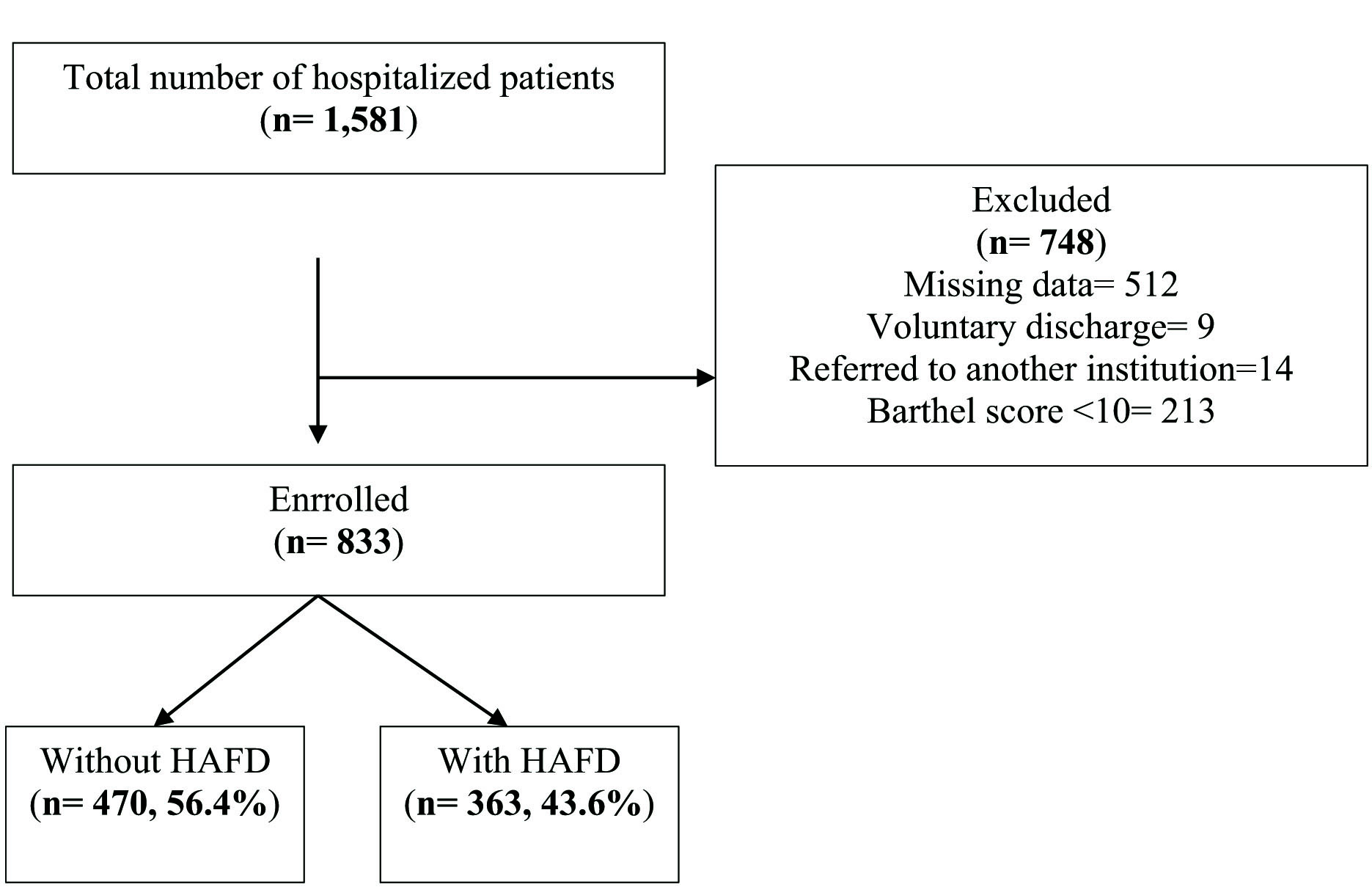
Of 1,581 eligible patients, seven hundred forty-eight were excluded due to various reasons (missing data (512), voluntary discharge (9), referred to another institution (14), Barthel score <10 (213)). The study finally included 833 patients (Figure 1), 473 female (56.9%), the majority older than 85 years (52.5%), mean age of 85.71 (SD 4.53). Of these, 363 (43.6%) presented hospital-associated functional decline at discharge. Table 1 shows the characteristics of patients, comparing groups with and without hospital-associated functional decline at discharge. The Median Barthel index at admission was 85 for both groups. However, the hospital length of stay was higher in the hospital-associated functional decline group (6 vs. 4, p-value <0.001). Likewise, delirium presented on admission in 201 patients, more commonly in the group with hospital-associated functional decline (18.3 vs. 31.7%, p-value <0.001).
Table 1 Comparison between patients with or without hospital associated functional decline (HAFD)
| Without HAFD (n= 470) | With HAFD (n= 363) | p-value | |
|---|---|---|---|
| Age in years, mean (S.D.), n (%) | 84.94 (4.4) | 85.71 (4.5) | 0.013 |
| 70-74 | 8 (1.7) | 2 (0.5) | 0.135 |
| 75-84 | 226 (48.1) | 160 (44.1) | |
| >85 | 236 (50.2) | 201 (55.4) | |
| Female sex, n (%) | 269 (57.2) | 204 (56.4) | 0.799 |
| Barthel score at admission, Median (IQR) | 85 (60-100) | 85 (60-95) | 0.574 |
| Modified Lawton, Median (IQR) | 7 (4-11) | 6 (3-10) | 0.029 |
| Malnutrition, n (%) | 295 (62.7) | 259 (71.4) | 0.009 |
| Hospital length of stay, Median (IQR) | 4 (2-6) | 6 (4-9) | <0.001 |
| Readmissions, n (%) | 59 (12.5) | 39 (10.7) | 0.422 |
| Polypharmacy, n (%) | 277 (59.1) | 222 (61.2) | 0.541 |
| Social support, n (%) | 65 (13.9) | 41 (11.3) | 0.271 |
| Delirium, n (%) | 86 ( 18.3) | 115 (31.7) | <0.001 |
| Nosocomial infection, n (%) | 7 (1.5) | 19 ( 5.2) | 0.002 |
| Dementia, n (%) | 133 (28.3) | 134 ( 37.0) | 0.008 |
| Hospital physical therapy, n (%) | 204 (43.4) | 91 (25.1) | <0.001 |
IQR: interquartile range, SD: Standard deviation
A previous diagnosis of dementia was more common in patients with hospital-associated functional decline (37.0% vs 28.3%, p= 0.008). Also, physical therapy during hospital stay was more common in the group without hospital-associated functional decline (43.4% vs. 25.1%, p <0.001).
HARP scale
Table 2 reports the HARP scale calibration using the ROE for each risk category. The HARP scale underestimated the risk of hospital-associated functional decline for patients in low-risk (ROE 1.82) and intermediate-risk (ROE 1.51) categories. The HARP overestimated the risk of hospital-associated functional decline for patients in the high-risk category (ROE 0.91). The H.L. was 55.96 with a p <0.0001.
Table 2 Calibration of HARP scale, observed vs expected events of hospital associated functional decline (HAFD)
| Lower limit | Upper limit | n | % total | Expected events | Observed events | Expected proportion | Observed proportion |
|---|---|---|---|---|---|---|---|
| 0 | 1 | 174 | 20.9 | 29.6 | 53 | 17 | 30.4 |
| 2 | 3 | 306 | 36.7 | 85.7 | 129 | 28 | 42.2 |
| 4 | 5 | 353 | 42.4 | 197.7 | 181 | 56 | 51.2 |
| Total | 833 | 100 | 312.9 | 363 | 37.6 | 43.6 | |
Expected proportion obtained from original study of HARP scale *Hosmer-Lemeshow = 55.96p<0.0001
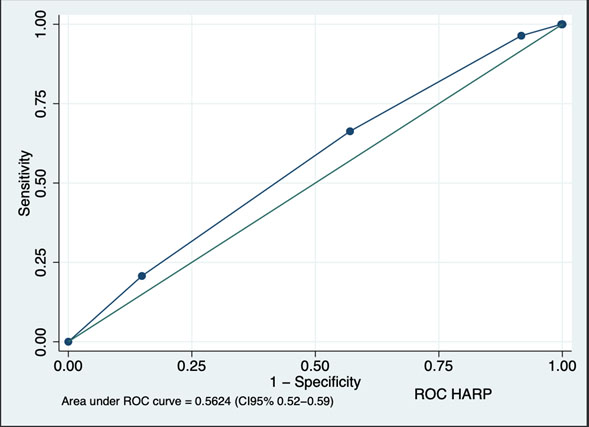
Figure 2 presents the assessment of HARP discriminative ability. The area under the curve (AUC) was 0.5624 (CI 0.52-0.59), well below the discrimination ability considered acceptable (0.7).
ISAR scale
Table 3 reports the ISAR scale calibration. The scale underestimated the risk of hospital-associated functional decline in both categories. The ROE was 1.59 in the low-risk category and 1.11 in the high-risk category. The H.L. was 30.15,p<0.0001.
Table 3 Calibration of ISAR scale, observed vs expected events of hospital associated functional decline (HAFD)
| Lower limit | Upper limit | n | % total | Expected events | Observed events | Expected proportion | Observed proportion | |
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 257 | 30.9 | 54.0 | 86 | 21 | 33.5 | |
| 2 | 5 | 576 | 69.2 | 247.7 | 277 | 43 | 48.1 | |
| Total | 833 | 100 | 301.7 | 363 | 36.2 | 43.6 | ||
Expected proportion obtained from original study of ISAR scale *Hosmer-Lemeshow = 30.15,p<0.0001
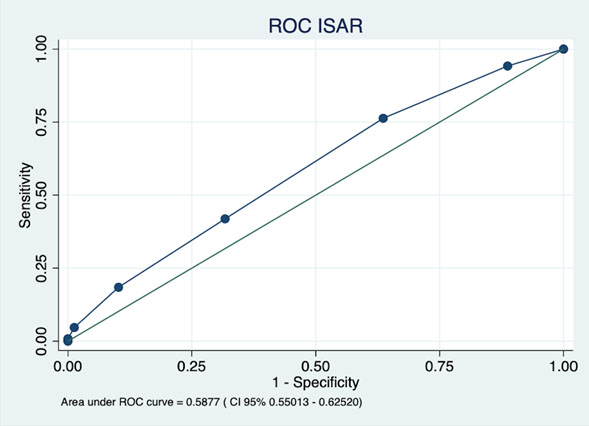
Figure 3 presents the assessment of ISAR discrimination ability. Again, the ROC curve showed a poor discrimination ability with an AUC of 0.587 (CI 0.55 - 0.62).
Discussion
The present study found a high proportion of hospital-associated functional decline at discharge (43.6%). This percentage was similar to previous studies, where the incidence fell between 35-70% 2-4.
In Colombia, Torres et al. (21, described that as many as 50% of patients aged 65 or older had an intermediate or high risk of hospital-associated functional decline, according to the HARP scale measured at admission. Such a proportion increased to 93.5% in patients older than age 85. Results in this study are similar, considering that most patients were older than age 85, with 79% in the intermediate- and high-risk categories.
Along with its ability to predict hospital-associated functional decline, the HARP scale is a good predictor of mortality. In a study following 474 patients, Liu described a significant increase in mortality risk at 30, 90, and 365 days in those with high HARP scores. In fully adjusted Cox proportional models, mortality odds in those patients was 3.5 times higher compared to patients with low HARP scores. This finding suggests that HARP allows for identifying patients with a high risk of hospital-associated functional decline and mortality after discharge 22. In addition, the same authors reported that the scale measured at admission could identify patients with a higher risk of requiring a skilled nursing or acute rehabilitation facility at discharge. After adjustment, the probability of being transferred to a facility was more than four times higher in participants with high HARP scores than in those with low scores (odds ratio= 4.58, 95% CI= 2.42-8.66) 23.
A systematic literature review searched for evidence of ISAR predictive value for adverse outcomes in older adults 8. The review included 32 studies with 12,939 patients and used a score ≥2 to identify patients at risk of functional decline. It found that ISAR had a modest predictive accuracy for emergency room return, hospitalization, or mortality. The scale had consistently high sensitivity (≥80%) and moderate to low specificity for all outcomes. That report considered ISAR a decision-making adjunct when determining which older adults might be safely discharged.
The present validation study found that HARP and ISAR have limited discrimination ability in predicting hospital-associated functional decline at discharge. Also, both scales may underestimate or overestimate the risk of hospital-associated functional decline. In other words, predicting hospital-associated functional decline with exclusive use of either scale may lead to underestimation of risk for patients categorized with low and intermediate risk. This could prevent those patients from receiving the necessary care to avoid deterioration during hospitalization.
The underestimation of the probability of developing HAFD in the low-risk categories observed in the ISAR and HARP scales may be due to the differences in our population compared to the studies in which the scales were initially described and in other populations in which that has been validated 24. In our population we found high rates of malnutrition, and older age, which predisposes our patients to worse outcomes. New studies should formally test this hypothesis.
Calibration was better for patients in the high-risk category of HARP, but the scale might slightly overestimate risk in some groups. This may lead to unnecessary interventions during hospitalization, increasing the cost of attendance. This is why these scales should be used as a complement to a thorough physical exam and tools that have already been validated. The comprehensive geriatric assessment (CGA), for instance, is a validated tool that assesses functionality as an expression of health in the elderly 25. Use of complementary tools helps to plan necessary interventions and treatments.
In this study, the use of physical therapy during a hospital stay was more common in the group without hospital-associated functional decline 26,27. The implementation of in-hospital physical therapy has advantages in multiple domains, such as physical, cognitive and functional. These findings are similar to that described in previous research, where it has even been shown that a multimodal exercise program is capable of reversing the changes associated with hospital-associated functional decline 13.
It is important to highlight that this is the first study with a large sample size that validates HARP and ISAR in a South American population.
This study has some limitations. It assessed the risk of hospital-associated functional decline at discharge but not at 30, 90, or 365 days. New studies are necessary to validate HARP and ISAR for long-term outcomes. This study did not measure variables that were part of the original validation, such as ethnicity. Our population corresponds mainly to white and mestizo patients, with a low representation of blacks or indigenous people, which makes it difficult to extrapolate results to these populations. New studies are required in these specific populations. Similarly, we did not record the admission diagnosis; however, previous observations have shown that the main reason for hospitalization in our population is a medical condition, with the most common discharge diagnoses being acute decompensation of cardiovascular, respiratory, and gastrointestinal diseases, similar to the populations in which the scales were designed
Conclusions
This study found that HARP and ISAR scales have limited discriminative ability to predict HAFD at discharge. The HARP and ISAR scales should be used cautiously in the Colombian population since they underestimate the risk of hospital-associated functional decline and have low discriminative ability.











 texto en
texto en