Remark
| 1) Why was this study conducted? |
| To describe factor associated with survival of patients living with HIV and cancer in Cali, Colombia. |
| 2) What were the most relevant results of the study? |
| Antiretroviral therapy and oncological treatment were associated with increased survival, and poorer prognosis was seen in patients with AIDS-defining infections and non-AIDS-defining infections. |
| 3) What do these results contribute? |
| These results assert the relevance of both antiretroviral and oncological treatment in the prognosis of patients with HIV and cancer, and reaffirm the importance of decreasing the rate of infections in these patients to improve survival. |
Introduction
In Colombia, the first case of AIDS was reported in 1984, three years after the first reports of the disease in 19811,2. According to UNAIDS, it is estimated that 200,000 [160,000 - 250,000] people of all ages with an HIV diagnosis live in Colombia, and 12,000 [8,400-20,000] new cases are diagnosed annually, for an incidence of 0.40 [0.26-0.61] per 100,000 inhabitants 3.
Various studies have shown that people living with HIV have a higher risk of cancer, including Hodgkin lymphoma, anal cancer, lung cancer, liver cancer and certain skin cancers, than the general population 4,5. With the emergence of combined highly active antiretroviral therapy (HAART), morbidity and mortality from HIV-related diseases, including Kaposi sarcoma and non-Hodgkin lymphoma, have been drastically reduced 6-8. However, morbidity and mortality from other types of cancer, such as anal, cervical, lung and oropharyngeal cancer and Hodgkin lymphoma, have remained high despite HAART 9,10.
According to an analysis of the HIV/AIDS situation in Colombia, non-AIDS-related neoplasms occurred in 0.74% of people living with HIV, while the frequency of AIDS-defining neoplasms were as follows: Kaposi sarcoma (1.76%), Burkitt lymphoma (0.34%) and invasive cervical cancer (0.14%) 11. This is comparable to estimates made in other parts of the world 5,12-15.
These estimates are made from different sources of information that are part of the country's Public Health Surveillance System 16. This system includes data on patients diagnosed with HIV and cancer 17,18. Nevertheless, there are other globally recognized sources of high-quality information, such as cancer registries, which collect, store, analyze and interpret data on new cases of cancer within a specific population and for a specific period and consequently allow estimates of the incidence, survival and mortality of cancer to be made 19. Therefore, there is a need to use high-quality and continuously collected information to understand cancer in people living with HIV. This study aimed to determine the survival of people with HIV and cancer.
Materials and Methods
Design and setting
A retrospective, hospital-based, observational cohort study was conducted in Cali, Colombia. Cali, the capital of the Valle del Cauca Province, is the third city in the country, with around 2,250,000 inhabitants in 2019 20. The network for cancer care has around 165 authorized oncology services in the Valle del Cauca located in the urban area 21. During the five-year period 2013-2017, 24,963 new cancer cases were diagnosed in permanent residents of Cali, with an age-standardized incidence rate for all locations in men of 191.2 and 175.4 in women 22.
Fundación Valle del Lili is a high-complexity university hospital serving as a southwestern Colombia reference center. It is one of the five hospitals that has integrated oncological services in the city, with a hospital-based cancer registry (HBCR) that includes data related to patient identification, cancer identification, the first course of treatment and outcomes. The case definition and registry methodology have been previously described 23. Data extraction was done by active search and continuous.
Patients and follow-up
HIV cases
Cases were obtained from the hospital HIV database from 2011-2019. This database included all people living with HIV treated in our hospital independent of time and place of diagnosis, disease stage, degree of immunosuppression or if they died during the observation time. Confirmatory tests for the diagnosis of HIV that are established in the "clinical practice guideline recommendations for the care of HIV/AIDS infection in adults, pregnant and adolescents" by the Colombian Ministry of Health were verified 24. A diagnosis of HIV was considered if the patient had two positive ELISA tests or two positive rapid tests, or a viral load above 5,000 copies/mL, or a positive Western Blot test. HIV cases are reported to the public health surveillance system database. The database includes information related to insurance, risk management and the impact of the disease 17,25.
Cancer cases
Cases were obtained from the Registro Poblacional de Cáncer de Cali (RPCC) database and HBCR from both sexes and all ages and localizations.
The RPCC is a population-based cancer registry that has operated continuously since 1962. It includes the new cancer cases through notification and active searching in primary data sources, including hospitals, clinics, pathology laboratories, and cancer centers. Then, it integrates the data into the database following the international standards of good practice. The RPCC has good information quality indicators, and its methodology has been previously presented 26,27.
Cases were men and women, all ages with a diagnosis of neoplasm (all localizations) codified according to the Classification of Diseases for Oncology 3rd edition (ICD-O-3) 28, no matter if it was confirmed or partially or fully treated. The basis for the diagnosis can be microscopic (fluid cytology, bone marrow, histology of a primary tumor and autopsy) and non-microscopic (clinical, surgical, and imaging diagnosis).
The Centers for Disease Control and Prevention (CDC) definitions of AIDS-defining neoplasms and AIDS-defining infections were considered 29. The oncological treatment variable included any medical-surgical intervention provided for cancer management.
Matching
The HIV cases database was matched with cancer cases databases (RPCC and HBCR). All neoplasms identified by the RPCC and HBCR were included.
Data
All cases were characterized based on the information in the medical records, the HBCR and the RPCC databases. It includes the IARC/WHO International Classification of Diseases for Oncology, third revision classification (ICDO-3), the age at diagnosis, location/topography, morphology and follow-up (last contact and vital status) of all patients.
The duplicate cases in all registries were identified and removed. Some characteristics such as identification, date of birth, health insurance regime, residence, ICD-O-3 code related to their cancer type and vital status were used to identify the common cases among databases.
A comparison was made in the proportions of HIV and cancer cases with the total cancer patients reported by the High-Cost Diseases Office report (period 2014-2018) and the RPCC (period 2014-2020).
Ethical considerations
The Comité de Ética en Investigación Biomédica of the Fundación Valle del Lili approved the study protocol following the ethical principles of medical research described in the Declaration of Helsinki and considering the regulations of Resolution 8430/1993 of the Ministry of Health and Social Protection of Colombia.
Statistical analysis
A descriptive analysis of the sociodemographic and clinical variables was performed using central tendency and dispersion measures.
Survival analysis was performed using the Kaplan-Meier method. Survival was calculated using the date of cancer diagnosis and the date of death or the last day of follow-up (the last day of hospital care and the date of last contact recorded; the most recent date was used). Random censoring was performed for cases that did not complete 5 years of follow-up. Overall survival for 12, 36 and 60 months of follow-up was calculated. The differences were evaluated using the log-rank test. A Cox regression was performed to evaluate the factors associated with survival. The assumption of proportionality was verified by specific tests of the model and Cox-Snell residuals.
A value of p <0.05 was considered statistically significant. All analyses were performed using STATA® (Version 14.0, StataCorp LP, College Station, TX).
Results
A total of 2,590 cases were reported in the hospital HIV database for the period 2011-2019; there were 463 duplicate records. Then, 245 patients were identified by matching the HIV and, RPCC and HBCR databases. After fulfilling the selection criteria, 72 patients were excluded due to incomplete information (n= 64), age younger than 18 years (n= 5) or the presence of a non-oncological tumor (n= 3). A total of 173 patients with HIV and cancer were included in the study.
Description of the cases
The demographic and clinical characteristics of the patients are presented in Table 1. The minimum age was 19, and the maximum age was 99 years. A total of 84.4% were male.
Table 1 Demographic and clinical characteristics of the included patients (n= 173).
| Characteristics | n (%) |
|---|---|
| Male sex | 146 (84.4) |
| Age (years), Me (IQR) | 43 (33-52) |
| Residence in Cali | 113 (65.3) |
| Cancer diagnosis year | |
| 1999-2005 | 7 (4.1) |
| 2006-2010 | 26 (15.0) |
| 2011-2015 | 99 (57.2) |
| 2016-2018 | 41 (23.7) |
| Time of onset of cancer since HIV diagnosis | |
| Prior to diagnosis | 107 (61.9) |
| Post diagnosis | |
| 0-2 months | 39 (22.5) |
| 2-12 months | 11 (6.4) |
| >12 months | 16 (9.3) |
| Hepatitis B | 8 (4.6) |
| Hepatitis C | 3 (1.7) |
| AIDS-defining neoplasms | |
| Non-Hodgkin lymphoma | 74 (42.8) |
| Kaposi sarcoma | 48 (27.8) |
| Cervical cancer | 8 (4.6) |
| Oncological treatment | 143 (88.8) |
| AIDS-associated infection | 108 (68.8) |
| Non-AIDS-associated infection | 113 (73.4) |
| Palliative care | 25 (16.6) |
| Vital status | |
| Alive | 109 (63.0) |
| Dead | 64 (37.0) |
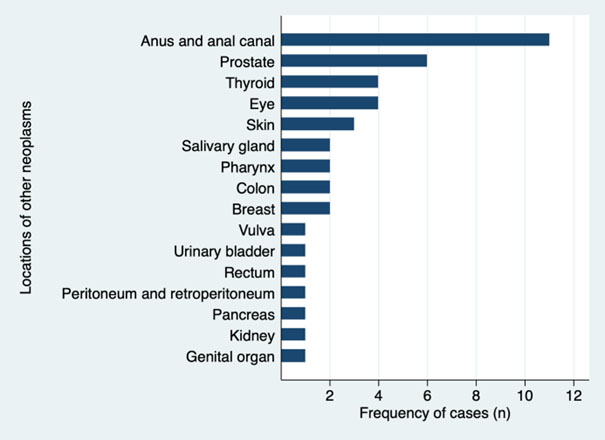
Thirty-three patients had a diagnosis of cancer prior to 2011. In most cases, the cancer occurred prior to the diagnosis of HIV (61.9%), while in 9.3% of cases, the cancer occurred one year after the HIV diagnosis. Regarding AIDS-defining neoplasms, the most common was Non-Hodgkin lymphoma (42.8%), followed by Kaposi sarcoma (27.8%) and cervical cancer (4.6%). The most common locations of other neoplasms (not related to AIDS) were the anus, anal canal (6.4%) and prostate (3.5%) (Figure S1, Supplementary file).
A total of 88.8% of the patients had undergone some cancer treatment: chemotherapy (n = 114), surgery (n= 31) or radiotherapy (n= 29). A total of 16.6% had at least one assessment for palliative care during their hospital stay. A total of 68.8% had an AIDS-defining infection. A total of 37.0% of the patients died during the follow-up period.
Comparison of cases
Table 2 shows the proportion of cases in our study (HIV and cancer) compared to the total number of cancer cases reported by the High-Cost Diseases Office report and the RPCC. A higher proportion of AIDS-defining neoplasms was observed in the FVL group for non-Hodgkin lymphoma and Kaposi sarcoma, while a higher proportion of cervical cancer was observed in the RPCC database.
Table 2 Comparison of Fundación Valle del Lili cancer cases, High-Cost Fund Report and RPCC.
| Type of neoplasms | HBCR* n=173 | RPCC† n=56,419 | CAC‡ n=24,405 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cali | Other Cities | Total | Cali | Other Cities | Total | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| AIDS-defining neoplasms | 130 | 75.1 | 3,349 | 9.2 | 2,036 | 10.2 | 5,385 | 9.5 | 961 | 6.3 | 717 | 7.8 | 1,678 | 6.9 |
| Non-Hodgkin lymphoma | 74 | 42.8 | 1,737 | 4.8 | 802 | 4.0 | 2,539 | 4.5 | 518 | 3.4 | 336 | 3.7 | 854 | 3.5 |
| Kaposi sarcoma | 48 | 27.8 | 109 | 0.3 | 37 | 0.2 | 146 | 0.3 | 36 | 0.2 | 14 | 0,2 | 50 | 0.2 |
| Cervical cancer | 8 | 4.6 | 1,503 | 4.1 | 1,197 | 6.0 | 2,700 | 4.8 | 407 | 2.7 | 367 | 4.0 | 774 | 3.2 |
| Other neoplasms | 43 | 24.9 | 33,152 | 90.8 | 17,882 | 89.8 | 51,034 | 90.5 | 14,302 | 93.7 | 8,425 | 92.2 | 22,727 | 93.1 |
*HIV and cancer cases, period 2011-2019.
†Population-based cancer registry, period 2014-2020.
‡High-Cost Diseases Office, period 2014-2018.
Survival analysis
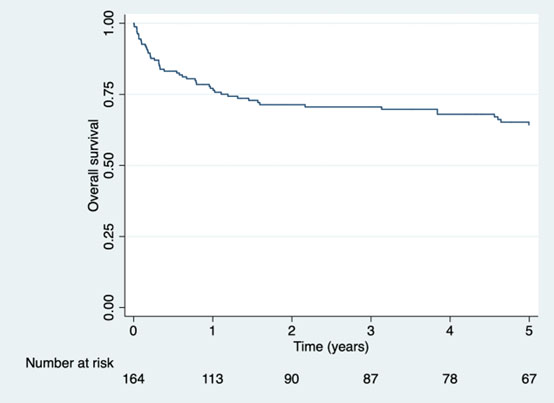
The median follow-up was 3.1 years (IQR= 0.4-7.2 years). Overall survival was 76.4% (95% CI: 68.9-82.3) at one year and 64.3% (95% CI: 55.7-71.6) at five years (Figure 1). Significant differences were found for the use of antiretroviral therapy (p= 0.021), AIDS-defining infections (p= 0.027), non-AIDS-defining infections (p= 0.013) and oncological treatment (p <0.001) (Table 3).
Table 3 Survival of patients with cancer and HIV in Cali, Colombia, period 2011-2019.
| Variable | Estimated five-year survival (95% CI)* |
|---|---|
| Sex | |
| Male | 61.7 (52.3-69.7) |
| Female | 77.8 (50.4-91.2) |
| Age | |
| <30 | 72.0 (47.6-86.4) |
| 30-39 | 59.3 (40.7-73.9) |
| 40-49 | 66.8 (50.4-78.9) |
| ≥50 | 62.2 (46.3-74.6) |
| Residence | |
| Cali | 64.5 (54.8-73.4) |
| Another municipality | 65.2 (49.1-77.3) |
| Antiretroviral therapy | 65.9 (56.4-73.8) |
| AIDS-defining malignancies | 62.3 (51.4-71.4) |
| AIDS-defining infections | 56.9 (45.7-66.6) |
| Non-AIDS-defining infections | 57.8 (46.7-67.4) |
| Oncological treatment‡ | 66.7 (57.4-74.4) |
*Kaplan-Meier method
‡ No data (n = 6)
Cox regression model that included the diagnosis of AIDS-defining infections, Non-AIDS-defining infections and oncological treatment showed that infections decreased survival (HR= 2.39, 95% CI: 1.05-5.46), while oncological treatment increased it (HR= 0.33, 95% CI: 0.14-0.80) (Table 4).
Discussion
This study presents survival findings for a cohort of people living with HIV and cancer from Cali, Colombia, during the HAART era. The findings show that AIDS-defining neoplasms (Non-Hodgkin lymphoma, Kaposi sarcoma and invasive cervical cancer) are the most frequently occurring types of cancer, followed by anal cancer, despite significant advances in the early diagnosis and treatment of HIV. Cancer treatment was found to significantly impact survival, while AIDS-defining infections contribute significantly to adverse outcomes.
Although the relationship between HIV and the occurrence of certain types of cancer is not fully understood, it has been associated with factors such as net immunity status (immunosuppression) and exposure to non-intrinsic exposure risk factors (coinfection with oncogenic viruses and lifestyle factors). This was reflected mainly by the frequency of alcohol and cigarette consumption and the frequency of AIDS-defining infections that characterize the advanced phase of HIV infection.
Non-Hodgkin lymphoma and Kaposi sarcoma are the most common neoplasms in patients with HIV 30-33. A study conducted between 2007 and 2014 at the National Cancer Institute in Bogotá DC that included 139 patients found that AIDS-defining neoplasms were present in 65.5% of cases; the most frequent were Non-Hodgkin lymphoma (n= 46), followed by Kaposi sarcoma (n = 42) 34. On the other hand, a study conducted in Cali described the incidence of these neoplasms before and during the HIV/AIDS epidemic (between 1962 and 2010) and found an association between the decrease in the incidence of Kaposi sarcoma in men and the introduction of HAART in Colombia starting in the year 2004 35. These findings show that AIDS-defining neoplasms are in decline due to advances in HAART and promotion and prevention strategies.
It is striking that the study, published by the public health surveillance system database in 2017, found a total of 736 cases of people living with HIV and cancer between 1983 and 2015 in the country, and of these, 35 cases (29 men and six women) were in the department of Valle del Cauca. The study was limited to neoplasms diagnosed between 60 months before and any date after the diagnosis of AIDS 36. It is very worrying that the public health surveillance system underestimates HIV-associated neoplasms (possibly due to limited sample size) because our study found at least 173 patients with these conditions during a shorter observation period and at a single hospital. This discrepancy shows an underreporting of people living with HIV and cancer, affecting public health decision-making and moving us away from the Sustainable Development Goals for HIV/AIDS. Similarly, it justifies the importance of cancer registries (population-based cancer registry and HBCR) as quality information sources for cancer.
Invasive cervical cancer was present in a low proportion in our cohort and can be explained by the lower proportion of women with HIV in the study population, which was also observed in the public health surveillance system report for this region 11. While cervical cancer continues to be the leading cause of cancer mortality in Colombia and the second leading type of cancer among women 37, it is possible that advances in primary prevention (prophylactic vaccines against HPV) and secondary prevention (early detection of cervical cancer with cervical cytology and DNA-HPV testing) and the strengthening of prevention and promotion programs through the implementation of clinical practice guidelines for early detection have had an impact on the burden of this disease in recent years.
Squamous cell carcinoma of the anus was the most common non-AIDS-defining neoplasm and had a mortality of 27%, similar to that reported in other published studies 38,39. This neoplasm is more prevalent among men who have sex with men (MSM) with HIV than in those who are not infected 40,41, and its incidence has increased in the last 30 years despite advances in HAART 42. These factors may be related to the low implementation of screening strategies for anal dysplasia in clinical practice 43-46, although it has been shown that anal HPV cytology has a positive impact on the reduction of anal cancer in MSM 47. Another factor to consider is the low vaccination rate in the male population48.
The overall survival at five years was 64%. Previous estimates for people living with HIV with AIDS-defining neoplasms range from 50-80% 49-51, and some estimates are higher than 90% 52. This is due to factors such as the human development index, access to the health system, neoplasia type, and the time since HIV diagnosis. In the patients in this cohort, a possible related factor was a delay in diagnosis of HIV, since 62% were diagnosed first with cancer and then with HIV. HIV preceded by a cancer diagnosis is a known predictor of mortality 52, a situation that has also been reported in Bogotá DC 34.
The age-adjusted mortality in Colombia was 3.31 (95% CI: 3.15-3.47) per 100,000 inhabitants, and the lethality was 13.17 per 1,000 in people living with HIV 11. Our study found no differences in survival between AIDS-defining and non-AIDS-defining neoplasms. Similar findings have been previously reported in Latin America, where patients with non-AIDS-defining neoplasms had survival probabilities that were equivalent to those with AIDS-defining neoplasms at one year of follow-up (81% vs. 79%) and were notably lower at five years of follow-up (60% vs. 69%). However, there were no significant differences (p= 0.18) 53. The survival rate found in this study was similar to that reported for other countries 54,55.
One factor associated with decreased survival was the diagnosis of AIDS-defining infections. Among the most prevalent opportunistic infections are Pneumocistys jirovecci (PCP), tuberculosis and toxoplasmosis 49,56,57. These infections are the main causes of mortality and admission to the intensive care unit in patients with HIV, despite advances in treatment 57. Therefore, the early and adequate initiation of HAART is relevant in this population, as is prophylaxis when the CD4+ lymphocyte count is less than 200 cells/mm3, a strategy implemented since 1989 and has improved survival 55,58. Similarly, close follow-up is necessary to control different risk factors in these patients, given that they have an immunocompromise profile different from that of the general population, and opportunistic infections can be present in as many as 70% of patients who die of HIV 49.
Regarding oncological treatment, it has been reported that the survival of patients with HIV and neoplasms is low, even when they receive oncospecific management 51,59. Although we found that oncological management was associated with better survival (HR= 0.32), management can be affected by several factors, such as the type of cancer and its location, the clinical stage at the time of diagnosis, secondary involvement, the type of treatment (surgery, systemic therapy, radiotherapy) and the presence of other associated comorbidities, which presents a challenge for professionals who care for people living with HIV and cancer.
Limitations
The study had several limitations, many of which resulted from its design. First, as a retrospective cohort study, it included data obtained from secondary data sources (medical records and health system databases); consequently, information bias could be present. Second, the study was conducted at a single health center in the city; therefore, it is not representative of the region. Finally, attempts to evaluate the impact of the presence or absence of cancer treatment on survival could be confounded by changes that occurred during follow-up, such as changes in the type of treatment, prescriptions and treatment approaches for cancer and changes in the patient's comorbidities. The situation was affected similarly by the prescription and initiation of HAART.
The strength of this study was the good quality of information regarding the description of cancer, its diagnosis and follow-up (vital status) from the RPCC and HBCR. The inclusion of this information makes this a unique study of the region.











 text in
text in