Remark
| 1) Why was this study conducted? |
| Traumatic wrist injuries have a high frequency of consultation, the structural damage, together with the immobilization time generates sequelae associated with pain, edema and functional limitation of the wrist and alteration of proprioception in the wrist joint. The evidence of its practice is not clear, there are multiple approaches, techniques, population sizes and follow-ups, which makes it difficult to establish which intervention should be used in rehabilitation, for how long it should be started and how often. This research aims to identify the evidence of proprioceptive interventions implemented in traumatic wrist injuries in adults. |
| 2) What were the most relevant results of the study? |
| Wrist proprioception rehabilitation is a topic that has received little attention in the scientific literature. Through the search conducted, few studies were found on the rehabilitation of proprioception of the wrist, however in the studies found that mention its clinical relevance in different pathologies not only traumatic but also degenerative of the hand and wrist, this lack of evidence is more pronounced when looking for the effectiveness of proprioceptive procedures. The results of the search indicate that the use of protocols based on motor imagery, sensory rehabilitation and proprioceptive neuromuscular facilitation can generate favorable clinical and statistically significant results in patients with traumatic wrist injuries, specifically with fractures of the distal third of the radius and triangular fibrocartilage injury. However, these results are not conclusive due to small sample sizes and the lack of unification of evaluation and follow-up criteria during treatment. |
| 3) What do these results contribute? |
| The findings of this research highlight the importance of exploring new avenues of study in the field of proprioception, especially in relation to the wrist. The lack of sufficient studies on the efficacy of proprioceptive techniques in this area underscores the need to undertake additional research with appropriate evaluation and follow-up protocols. To advance in this field, it is recommended that studies be conducted that consider the essential criteria of proprioception, such as the neuromuscular system, the sensory system, and the musculoskeletal system. These investigations must have a significant population sample in order to conclusively demonstrate the effectiveness and clinical relevance of proprioceptive techniques applied to the wrist. |
Introduction
Traumatic injuries of the wrist are frequent; out of 436 traumatic injuries of the upper extremity, 77.0 % are of the wrist, and of these, 38.6 % are fractures of the distal third of the radius, which can generate functional, proprioceptive, and occupational limitations 1,2. Proprioceptive impairment has gained importance in recent years, and proprioceptive re-education practices have been postulated as the primary strategy to improve function in this type of injury 3, which makes it necessary to initiate medical and therapeutic treatment 4 to reduce associated complications such as pain, edema, limitation of joint mobility, and loss of strength 5-7.
Proprioception is a sensory function with receptors in the skin, muscles, tendons, and joints that carry information to the central nervous system for conscious and unconscious control of position sense, joint movement, muscle strength, and balance 3,8,9 (Figure 1).
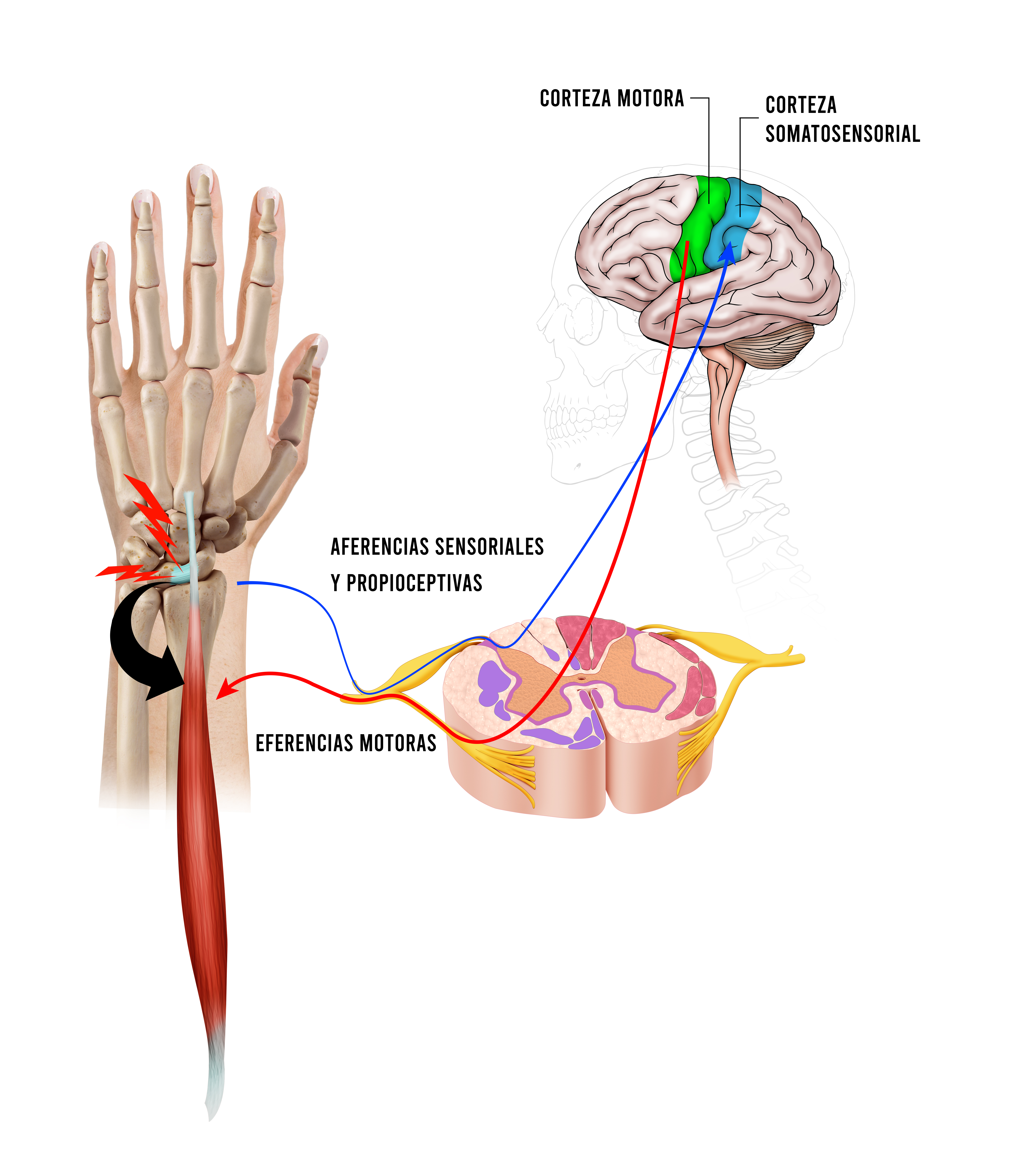
Figure 1 Principles of the wrist proprioceptive pathway. Certain anatomical and physiological criteria must be met for a joint to have a proprioceptive function. In the joints there are mechanoreceptors, which respond to stimuli (pressure, movement, and speed), sending afferent information through the dorsal horn of the spinal cord, information that will be processed in the somatosensory cortex and derived to the motor cortex to finally send the motor response that travels along the efferent pathway, reaching the anterior horn of the spinal cord, and from there the motor neurons will synapse at the neuromuscular junction to cause motor action.
Proprioceptive rehabilitation has been studied in lower limbs since the last century with positive results, and these have been extrapolated to upper limb rehabilitation. Only since 2009 has proprioceptive rehabilitation been investigated in the treatment of hand and wrist injuries of traumatic origin 9,10.
This review aims to identify proprioceptive rehabilitation strategies for recovering traumatic wrist injuries without neurological injury and their effects on pain, functionality, strength, joint mobility ranges, and edema.
Materials and Methods
A scoping review was carried out following the Prisma ScR 11 methodology for scoping review and the Joanna Briggs Institute Manual 12.
Inclusion and exclusion criteria
A search was conducted for scientific articles describing the use and outcomes of proprioceptive rehabilitation in adults with traumatic wrist injuries. Articles of clinical trials, cohort studies, and case studies were considered, and published in English, Spanish and Portuguese, with no restriction on publication date. The filters of title, abstract and content were applied, and the date of collection or search for information was made with a cut-off date of November 2023. The following research question (PICO) was established:
Participants: adult patients over 18 years of age with a diagnosis of posttraumatic wrist injury.
Interventions: proprioceptive rehabilitation in posttraumatic wrist injury.
Comparison: none, other intervention, or conventional management.
Results: pain, function, strength, joint mobility ranges and wrist edema.
Narrative articles, cross-sectional studies, editorials, and letters to the editor were excluded. Investigations with patients with neurological and adjacent joint lesions were excluded to better appreciate the effect of proprioceptive rehabilitation.
Search methods for study identification
The search process and identification of studies were performed using the following terms: Rehabilitation, Hand Injuries, Wrist Injuries, Proprioception, Physical Therapy Modalities, establishing the following combinations, (Rehabilitation) AND (Hand Injuries)) AND (Proprioception), rehabilitation [MeSH Terms]) AND (Wrist Injuries [MeSH Terms]) AND (Proprioception [MeSH Terms]), (Hand Injuries) AND (Proprioception), (Wrist Injuries) AND (Proprioception), ((Rehabilitation) AND (Proprioception)) AND (Wrist Joint). For the search of articles in Spanish and Portuguese, the translation of the term was performed with the thesaurus of structured and multilingual vocabulary, DeCS.
Searches were performed in PubMed, Embase, LILACS, PEDro, and Google Scholar databases.
After removing duplicate articles, two authors independently reviewed the selected articles to verify the study typology. Subsequently, the full text was reviewed to define the articles considered in the review. When there was a discrepancy between the authors, it was discussed, and consensus was reached with the third author. The following data were extracted from the selected articles: authors, country, study population, type of study, intervention performed, and main results, as well as the advantages and limitations of the study.
Results
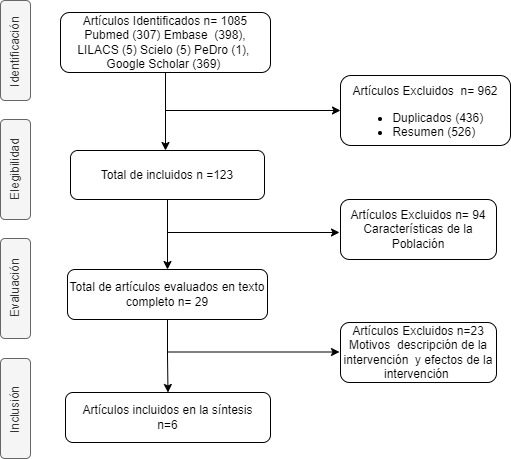
A total of 1,085 articles were identified in the databases. There were no meta-analysis articles. We removed 436 duplicate articles. The authors excluded 526 articles by abstract. A total of 123 full-text articles were retrieved, of which 94 were excluded because they did not meet the population criteria, and 23 articles were excluded because the description of the proprioceptive intervention was not explicit. The analysis for the review was performed on six articles (Figure 2).
Characteristics of the included articles
The six selected articles included 125 subjects, with female gender and right-handed dominance predominating. The most frequent diagnoses were distal radius fracture and triangular fibrocartilage injury. Table 1 shows the characteristics of the population and the type of study.
Table 1 Population, injury, and study type characteristics of the articles on proprioceptive wrist rehabilitation.
| Author | Country | Population | Diagnostic | Type of Study |
|---|---|---|---|---|
| Dilek et al. 13 | Spain | Group 1: 14 patients with conventional rehabilitation, 5 men and 12 women. Average age 52.59 | Distal-third radius fracture | Single-blind randomized controlled trial |
| Group 2: 19 patients with proprioceptive rehabilitation, 7 men and 12 women. Average age 47.16 | ||||
| Wollstein et al. 14 | United States | Group 1: 31 patients with conventional rehabilitation, mean age 63.9 | Distal-third radius fracture | Prospective therapeutic study |
| Group 2: 29 patients with proprioceptive rehabilitation, average age 62.3 | ||||
| Zhiqing et al. 15 | Singapore | One 23-year-old patient | Triangular fibrocartilage injury | Case study |
| Zhiqing et al. 16 | Singapore | 10 patients with proprioceptive rehabilitation have an average age of 33.5 | Triangular fibrocartilage injury | Pretest-posttest single-group experimental design |
| Karagiannopoulos et al. 3 | United States | 33 patients with proprioceptive rehabilitation: 20 surgical patients, mean age 58.4 13 non-surgical patients with a mean age 61.6 | Distal-third radius fracture | Prospective longitudinal cohort study |
| Hincapie et al. 17 | United States | One 43-year-old woman | Partial dorsal intercarpal ligament tear and right wrist scapholunate ligament sprain | Case study |
QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand; PRWE = patient-rated wrist evaluation JPS= joint position sense measurement
The articles describe the following techniques: graded motor imagery, sensorimotor home protocol, proprioceptive neuromuscular facilitation (PNF), motor work through dart coactivation, and mirror therapy.
In a randomized controlled trial in patients with surgically treated fractures of the distal third of the radius (19 patients), the graded motor imagery technique was used for eight weeks with image recognition and mirror therapy; it was compared with conventional therapy (14 patients), and progress was evaluated at the second, fifth and, eighth weeks with the visual analog pain scale (VAS), Jamar dynamometer, QuickDASH score (Quick Disabilities of the Arm, Shoulder, and Hand) and the Michigan Hand Questionnaire (MHQ). The intervention group showed improvement in pain intensity at rest and joint mobility ranges compared to the control group, and follow-up upper limb function was equivalent in the control and intervention groups.
The graded motor imagery technique was combined with sensorimotor strategies in patients with distal radius fractures (29 patients) compared to a conventional therapy group (31 patients). The progression of graded motor imagery is not detailed; sensory stimulation was performed by recognizing textures with eyes open and closed. The intervention was performed daily at home, and the evaluation was done in the third week and three months after the intervention. The sensory deficit was evaluated with sensorimotor tests with Semmes-Weinstein monofilaments, static and dynamic 2-point discrimination, vibration tests, temperature, Moberg detection in a timed manner, stereognosis, and proprioception tests 14. The investigation demonstrated sensory improvement; however, no differences were found in pain sensitivity, functionality, strength, or mobility.
In a case study, mirror therapy was the primary strategy for a patient with a triangular fibrocartilage lesion. This technique was used in the first weeks of intervention, promoting movement awareness exercises through the mirror; from the fifth week on, active muscle strengthening exercises were included with manual resistance in wrist stabilizing muscles and exercises with a gyroscope, which is a device that generates forces in multiple directions, thus stimulating proprioception. In the ninth week, active exercises with external resistance were started 17. After the intervention, significant changes were achieved in palmar pressure strength, pain, and functionality for the initial assessment.
The other three articles used the proprioceptive rehabilitation technique (PRT) 3,15,16. Chen et al., applied a protocol to a patient with a triangular fibrocartilage lesion consisting of dart throwing motion (DTM) work to organize manual restoration, adding closed kinetic chain exercises with attachments such as balls and generating weight load as well as bilateral upper limb patterns; then, weight and band work were added, and the load was organized according to the patient's response 15. The patient's pain and functional limitations decreased. Subsequently, he applied this protocol to ten patients with the same injury with similar results 16. In the last study, in 33 patients with fractures of the distal third of the radius (20 post-surgical and 13 without previous surgery), proprioceptive therapy was added to conventional rehabilitation without describing the technique or dose. They did not find significant changes concerning the control group 3.
Discussion
The term "proprioception" derives from the Latin "proprius" ("belonging to oneself") and "-ception" ("to perceive"). It allows to perceive body parts' location, movement, and action. For this purpose, it considers all central and peripheral structures; therefore, proprioceptive rehabilitation should integrate three principles: kinesthesia, joint position sense, and neuromuscular control, to reduce pain and edema, improve mobility, joint stability, and muscle strength, which translates into greater functionality of the involved segment. These principles are fundamental to optimizing the results of the interventional process. Kinesthesia, by focusing on movement awareness, improves control and coordination, strength, and stability. Work provides improved functionality and establishes a solid foundation for movement, thus enhancing functional capacity and reducing vulnerability to injury. Body awareness, essential for understanding position and movement in space, should be integrated into the rehabilitation process for this purpose as well; for its progression, the recovery times of the tissues involved should be considered 9,18.
Currently, several approaches work in isolation on the principles of proprioceptive rehabilitation; its applicability has been reported in joints such as the knee and ankle and neurological injuries 19,20. The risk associated with proprioceptive interventions is low due to the non-invasive nature of these techniques. In terms of economic efficiency, they are cost-effective compared to other therapeutic options since they do not require the purchase of specialized equipment, presenting an economical alternative to improve motor function and quality of life 8,9,21,22. These advantages of proprioceptive rehabilitation are similar when implemented for traumatic wrist injuries. However, there are limitations such as the number of subjects included in the studies, follow-up during treatment with low rigor and diversity of evaluation instruments.
Therefore, its clinical relevance and effectiveness are necessary for current and future practice in wrist rehabilitation, improving follow-up processes that include proprioceptive principles and integrating the neuromuscular, sensory, and musculoskeletal systems. Likewise, standardization processes should be generated that adjust the intensity and duration of the sessions according to the patient's condition and capabilities, thus reducing potential risk.
Other studies were excluded due to the lack of clarity regarding the interventions' dosage, frequency, and follow-up. The absence of detailed information on these critical elements makes it difficult to assess the effectiveness of the interventions studied effectiveness accurately 5,8,9,19-38.











 text in
text in