INTRODUCTION
Primary Health Care (PHC), defined by the Declaration of Alma-Ata [1] as a strategy that has the potential for achieving health for the entire population, refers to a series of values, principles, conceptual and methodological concepts which form a broader view of health that comprise a wide spectrum of aspects, from policies that govern, including the proposal of a number of tools for: establishing and implementing health systems with universal access; organizing and operating comprehensive health care services, focusing on the person, family, specific communities and population from a specific territory (as a whole); cross-sectorial and participatory formulation of public policy; and promotion of social and governmental leadership that might serve the main objective of contributing to the achievement of the highest level of health as possible, with emphasis on the right to health, equity and social solidarity. The World Health Organization (WHO) proposes the transformation of health systems under the approach of PHC to improve the health of communities by integrating interventions in public health, primary care, and the creation of public policies [2].
In Colombia, Law 1438 of 2011 [3] reformed the health system to strengthen it with a health service model framed in the strategies of PHC, allowing coordinated action of the State, institutions and community to improve health and generate a safe and healthy environment to provide inclusive, equitable and higher quality services [4].
The World Health Report 2008 [2] shows the relevance of PHC to transform health systems around the world. The experience of three countries (Canada, Brazil and Thailand) that have been able to accelerate the PHC reform point to three com- mon elements to advance in the effective dialogue on related policies, namely: (i) the importance of Health Information System (HIS) useful for the reform of PHC; (ii) the systematic exploitation of innovations; and (iii) the exchange of lessons on what is effective. The report highlights the role of HIS as providers of information required to guide policies on health and in general, to meet the needs of multiple organizations and users.
The most accepted definition of HIS is the one proposed by the International Medical Informatics Association (IMIA) [5] that conceived them as the composition between team, human resources, computer applications, procedures and policies for the management of health information. Given that HIS is an essential tool to support the strategies of PHC, it is important to have criteria and mechanisms to establish whether in a specific location these satisfy adequately the implementation of the PHC strategy. This satisfaction is affected by factors such as: different approaches or existing models of PHC; diversity of interpretations of the Primary Health Care [6]; use of HIS that was not designed to support PHC; and limited capacity of adaptation of HIS to regulatory changes that govern health systems.
The current paper presents a characterization of the information systems that support PHC, built upon a widely accepted model for the implementation of PHC strategies. This characterization has been developed as a first approach towards the formalization of criteria and mechanisms to be used in the evaluation of the degree of compliance of HIS to PHC strategies implementation.
1. MATERIALS AND METHODS
To the characteristics that determine the degree of adjustment of HIS to the strategies of PHC, the following steps described in this section were performed: i) identification of approaches used when implementing PHC strategies which resulted in the adoption of a PHC deployment formal model as the foundation for characterization; ii) literature review of HIS used in PHC, which allowed identifying a set of characteristics that represent requirements exposed by experts regarding the provision of health care services, HIS functionalities to withstand PHC, and features described in demonstration experiences of National Health Systems; iii) definition of the characterization of HIS according to the adopted PHC model, by means of selecting and classifying the identified characteristics, and specifying the instruments and procedures for verifying its accomplishment; and finally, iv) validation of the characterization by applying those instruments and procedures on a particular implementation of a strategy of PHC and comparing the results with relevant literature. For this validation the PHC strategy implementation in the municipality of Santander de Quilichao in 2015 was chosen.
1.1. Approaches to PHC
In order to determine which needs must be fulfilled by HIS to properly support a PHC strategy, it was necessary to count with a clearly defined approach for its implementation, however, diverse implementations of PHC exist, most of them derived from the Declaration of Alma-Ata [1].
According to the Pan American Health Organization (PAHO) [6], there are many erroneous conceptual interpretations of PHC, and discrepancies regarding its meaning among countries, and even within a same country. Finally, all the ideas on the role of PHC have been categorized by PAHO/WHO into four approaches [6]: i) selective primary health care -most common in developing countries- which focuses on a set of specific services defined as GOBI (Growth monitoring, Oral rehydration, Breastfeeding and Immunization control); ii) primary care -referred as the first level of care- which attends great part of the population, highly implemented in industrialized countries; iii) Alma-Ata “comprehensive primary health care”, a strategy for organizing healthcare systems and society to promote health, defined as “essential health care based on practical, scientifically sound and socially acceptable methods and technology made universally accessible to individuals and families in the community through their full participation and at a cost that the community and country can afford to maintain”; and iv) Health and Human Rights approach, which differs from Alma-Ata not so much on principles, but rather on highlighting the need to face social and political determinants of health.
PAHO and WHO have promoted the renewed approach to PHC [6], which rescues the initial concept of PHC declared in Alma-Ata and has become a formal concept adopted by many national health systems, including Colombia, that ratified it under the Law 1438 of 2011 [7]. The definition of an international approach to PHC implementation is very convenient, but it was not enough from this papers perspective, since such approach does not establish a model or methodology that facilitates the implementation process of PHC strategies . In this sense, different deployment models were found that are consistent with the guidelines set out in the declaration of Alma-Ata [8-11]. The main references of such models point to the work done by Dr. Sidney Kark in the health center of Pholela (South Africa) [12] during the 1940s, which resulted in the model known as Community-Oriented Primary Care (COPC). It is a practical model that aims to streamline, organize and systematize existing health resources through interventions that reflect the principles contained in the Alma-Ata Declaration [13-14].
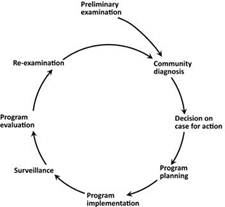
The COPC model consists of a cycle conformed by eight phases (figure 1), described below [11]:
Preliminary examination, corresponds to an overview of the community that will be intervened.
Community diagnosis, identification of the population, its geographical dispersion, relevant social characteristics and needs in health.
Decisions in cases for action, phase where a health problem or set of problems are selected throughout the analysis of priorities.
Program planning, in-depth analysis of health needs, including physical, biological and social determinants, making emphasis on prioritized health problems.
Program implementation, corresponds to the deployment of defined health programs, integrating promotion, diagnostic prevention, treatment and rehabilitation activities.
Surveillance, comprises monitoring activities and demographic surveillance to identify changes, as well as the follow-up of the population’s health condition.
Program evaluation, assesses the services provided to the community before and after, and the effectiveness of the intervention.
Re-examination, by means of “re-testing” it is decided if the program is maintained, modified or suspended, new priorities are set, and a new COPC cycle is started.
A full implementation cycle varies according to the population or selected health problems and the available resources during all phases.
The COPC model is the most complete and accepted according to the cited papers, so it was adopted as a formal model in this work to perform the characterization.
1.2. PHC Information Systems
HIS incorporate the use of Information and Communication Technologies (ICT) in the health domain, and thanks to their progress, they have extended throughout many places and services in the sector, to such extent that today, a wide variety of types can be identified, including traditional systems for the management of administrative and accounting information, electronic health records, more specialized information systems as those for radiology, laboratory, pharmacy, telemedicine, surveillance of public health, etc., and even decision support systems and personal health records [15].
HIS comprises a fundamental tool to support COPC model implementation since they help to obtain the specific characteristics of a territory and know the distribution of population and the penetration degree of community health services [11]. Nevertheless, it was necessary to establish in a precise manner the way in which these systems should support the PHC implementation and the required functionality so as to fulfill the expectations proposed by the declaration of Alma-Ata and the COPC implementation model. To achieve this, a literature review was conducted as described below, in which different Information Systems considered as referents were studied, as well as some descriptions and analysis of HIS for PHC.
1.2.1 National and Regional Health Information Systems
Some of the most representative National Health Information Systems (NHIS) involving PHC are: (i) the Canadian program Infoway [16], which has a unique information system that provides interoperable architectures, implementation guidelines of standards for PHC, and a framework for evaluation of information systems adapted to national standards and certification systems. Among its most representative components: the demographic information system, the provider of search for information, the system of allergies/intolerances, the observatory and the intervention HIS; (ii) NHS Digital [17] from the United Kingdom, which -as the Canadian model- offers guidelines and tools needed to implement information systems adapted to a national architecture. It has a great diversity of modules and services, including the Primary Care Informa- tion System (PCIS), which allows to integrate various information databases for data analysis, management of patients profiles, analysis and generation of statistics, geo-referencing of information, etc.; and (iii) Primary Health Network (PHN) [18], which is a project for strengthening the Australian health system, supported by the Australian Digital Health Agency [19]. within its objectives, it includes using telehealth systems to accelerate the flow of patient information among health care providers, and it includes a national infrastructure that supports maps of health needs, centralized reporting and the integration with My Health Record [20], a platform that manages the personal health records, and supports data standardization and knowledge-based decision-making.
In Latin America, some countries count with proper NHIS to support PHC strategies. For example Argentina, Brazil, Chile, Colombia, Costa Rica and Mexico have Integrated Systems of Social Information that allow to unify population registration, monitoring and evaluation of social programs and database integration [21], which are necessary functions for the first phases of the implementation of PHC. Also, it must be kept in mind that HIS works under each country’s strategies. For example, in Chile the strategy “Chile crece contigo” (Chile grows with you) [22] has enabled to develop a unique HIS [23], which integrates the system for monitoring and tracking of minors registered in the growth and development program, the registration of families, the exchange between databases of the social information record, etc.
In Colombia, Sispro [24] was developed as a tool that allows to manage information for decision making, policy development, and monitoring the services’ management in the attention levels and essential processes of the sector. It was designed as a data warehouse that integrates different sources of information used in the sector and contains the essential aspects to obtain the preliminary diagnosis of a population (initial phase of PHC). At regional level, in Bogotá there is a system called “APS en Línea” (online PHC) [25], with which population characterization, monitoring and intervention of actions developed by health service provider institutions can be performed [26]. Other relevant implementation experiences in the country´s history of public health reference the Multidisciplinary Research Center for Development (Cimder) at the Universidad del Valle, which developed an application program for PHC named “Sistema de Información de base Comunitaria para Atención Primaria en Salud” (Sicaps) (Community Based Information System for PHC) [27]. One of the use cases of this HIS for PHC was reported in [28], which evaluated the implementation of the PHC strategy in the municipality of Santander de Quilichao in the Department of Cauca; the use of Sicaps for data gathering through familiar data sheets and the analysis of the collected data was essential.
For closing this subsection, it is worth mentioning the affirmation of the PAHO cited in the last reference, in the sense that in order to achieve an adequate integration across the different levels of care, and to strengthen PHC, the requirements are: “good information systems that enable adequate planning, monitoring and performance evaluation; appropriate financing mechanisms that eliminate perverse incentives and assure continuity of care; and evidence-based approaches [for] diagnosis, treatment, and rehabilitation” [6].
1.2.2. Analysis of HIS for PHC
At a general level, the most relevant work found was the comprehensive analysis of the contribution of the Information Technologies (IT) to PHC in the developing countries, exposed in [29]. In this paper, a literature review performed on 52 prioritized articles out of 887 about this subject is presented, a classification for HIS is proposed, and its advantages and limitations are discussed.
Regarding specific experiences, the most significant were the following. An evaluation of the quality of HIS in the first levels of attention and how they contribute to PHC was made in Argentina [30]. The evaluation is based on the definition of HIS processes in the first level of care, and the measurement of indicators is defined on the basis of the components of Information Systems. In the description of the information system for PHC of Croatia, called Primary Healthcare Information System (PHCIS) [31], authors explain the challenges faced for its design and implementation, the architecture and key quality features considered such as interoperability, modularity, etc., and conclude that PHCIS is the cornerstone for the next generations of health services in this country. In the evaluation of the information systems that support the program Prevention of mother-to-child transmission of HIV (PMTCT) accomplished in two health districts of South Africa [32], the Primary Health Care Information System used in the Western Cape Province was included. It offers a set of functionalities for PHC such as the access to patient records through a unique identifier, the collection of demographic information, the control of appointments, etc. [33].
An information system used to support PHC strategies that deserves special mention is the District Health Information System (DHIS2) [34], which is widely used in the world and it is one of the most complete and most referenced systems in the PHC scope, providing a great contribution to the experience in the use of information systems in this context [35-38]. Ihe role of information in decision-making in PHC is described in [39], emphasizing on the use of surveys and studies for the collection of necessary data, and the need to have the right team. To support decision-making, an information management cycle is proposed, technologically supported by DHIS2, which is described in [40].
On the other hand, several papers describe the flaws of HIS in supporting PHC strategies [28,41-44]. In the PHC experiences in Colombia systematization published by the Ministry of Social Protection [45], authors describe how, although the PHC information systems have allowed to cover gaps in information and improve decision making, their particular development by regional or local authorities has generated conflicts and incompatibility with other HIS at a territorial level, and point out that the wrong assessment of HIS has resulted in many questionings to the systematiza- tion. Some of the most relevant problems described are: i) insufficient information for decision-making; ii) little ability to integrate information from other systems; and iii) HIS with inappropriate approaches.
1.3. Elements of characterization
From the literature review described in the previous section, it was concluded that there is no established set of features that can determine the degree of adjustment of HIS to the context of PHC, and that, on the contrary, there are different approaches, views and concepts about PHC and its implementation. However, this review allowed to identify 93 characteristics that represent:
Requirements exposed by experts in the PHC model both at political/administrative level and in the intervention, which specifically refer to the provision of health care services.
HIS functionalities to withstand this context, and
Features described in demonstration experiences of National Health Systems.
Table 1 presents the sources from which the identified characteristics were obtained, the number of these ones by each source, and their description.
Table 1 HIS characteristics identified in the PHC context
| Source | Identified characteristics |
|---|---|
| Infoway [16] | 8 characteristics, some of them are: patient demographic information, information from providers of services and products needed in care, patient care information, etc. |
| Adopting electronic medical records in primary care [46] | 11 characteristics, some of them are: relationship patient-health service provider, information associated to patient’s safety, calculation of time needed for imple mentation, etc. |
| Primary healthcare information system [31] | 6 characteristics that describe quality and technological HIS requirements, namely: use of interoperability standards (Hl7-EVN), interoperability with other systems, systems modularity, information migration capability, systems stability, information safety and privacy . |
| DHIS2 [35-39] | 5 characteristics, referring to DHIS2 as an information system in PHC, namely: data collection at different levels, to improve the information quality, to permit the information interpretation, to support the monitoring and assessment of health programs, activity planning, information analysis. |
| COPC model [8-11,13] | 25 characteristics, most of them refer to the needs of information for each PHC phase; some of them are: information of territory characteristics, distribution of population, penetration of health services (network of services), identification of the population, etc. |
| Renewed approach to PHC [2,6] | 4 characteristics, namely: definition of new priorities, availability of information, sufficient information, laws of the health systems in the countries. |
| NHS Digital [17] | 7 characteristics, namely: multiple users at the same time from different platforms; unified database; to see and print basic data; combination of data with other information sources; detailed analysis through graphics, data, etc.; geolocated data; information about finances, clinical records, pharmacy and laboratories. |
| Australian Digital Health Agency [18-20] | 5 characteristics, namely: personal health record, registration of information in the attention flow, to support knowledge based on decision-making, to support the development of the telehealth strategy, use of standardized data, priority population attention. |
| Chile strategy [22] | 3 characteristics, namely: follow up and control of children, family registration, unified database. |
| Sispro [24] | 3 characteristics, namely: unified database, detailed analysis through graphics, data, etc., use of standardized data. |
| Information systems in the first level of care [30] | 16 characteristics, grouped in three categories, namely: structure (redundancy, relevance, regulatory compliance), process (simplicity, use of available technol ogy, reliability, flexibility), result (effectiveness, efficiency, validity, clarity and conciseness, opportunity, use, confidentiality and safety, regulatory compliance). |
The next step after the identification was to unify equivalent characteristics and their classification. At the end 72 were obtained, organized in 3 dimensions and 16 subdimensions as shown in tables 2-5. These categories correspond to the different points of view which should be considered to determine the behavior and level of adjustment of HIS in the context of PHC; the dimensions represent the most general concepts while the subdimensions correspond to the most specific ones. Below, dimensions are described:
Table 2 Dimensions and subdimensions of the characteristics
| Dimensions | Subdimensions |
|---|---|
| Health Information Technologies | System functionality Software quality standards Integration and interoperability of information systems System requirements |
| Health Services Organization | Clinical records Administrative records Network of services provision Health service standards PHC implementation sheets |
| PHC Reference Model | Program evaluation Re-examination Community diagnosis Decision in cases for action Surveillance Program Planning |
Source: the authors
Table 3 Subdimensions and characteristics associated to health information technologies dimension
| Subdimension | Characteristics |
|---|---|
| System functionality | 1) Supports the process of data capture and processing; 2) Permits the query and verification of collected information; 3) Permits the data georeferentiation; 4) Permits to see and print basic data of the person, population or family. |
| Software quality standards | 5) Availability of the information system; 6) Efficiency of the information system; 7) The used system is modular; 8) Stability of the information system; 9) The presented information is sufficient; 10) Supports collection at different attention levels (scalability); 11) Supports multiple users at the same time (multiuser); 12) guarantees information privacy; 13) guarantees information safety. |
| Integration and interoper ability of information systems | 14) Contributes to the standardization of information; 15) Permits to combine data with other information sources; 16) Permits the migration of other information systems; 17) Supports the interoperability among the different used systems; 18) Use of standardized data; 19) Uses terminologies; 20) Uses standards for interoperability (HL7-EVN). |
| System requirements | 21) Contributes to the improvement of information quality; 22) Design of the information system with collaborative participation; 23) Supports different platforms both online and offline; 24) Supports the development of the Telehealth strategy; 25) Supports socio-technical interaction. |
Source: the authors
Table 4 Subdimensions and characteristics associated to health services organization dimension
| Subdimension | Characteristics |
|---|---|
| Clinical records | 26) Permits registration of allergies and intolerances; 27) Permits registration of personal health records; 28) Permits registration of information in the attention flow; 29) Permits registration of laboratories; 30) Permits registration of medication; 31) Permits registration of vaccinations; 32) Permits registration of clinical observations. |
| Administrative records | 33) Financial information (billing, contracting of services); 34) Presents operation costs. |
| Services provision network | 35) Administers information of health centers; 36) Permits the relationship patient-service centers; 37) Supports all the attention phases (promotion, prevention, diagnosis, treatment and rehabilitation). |
| Health service standards | 38) Supports the quality of attention evaluation; 39) Supports the patient’s safety evaluation. |
| PHC implementation sheets | 40) Permits registering an intervention; 41) Permits the project management. |
Source: the authors
Table 5 Subdimensions and characteristics associated to PHC reference model dimension
| Subdimension | Characteristics |
|---|---|
| Program evaluation | 42) Supports intervention efficacy evaluation; 43) Grants access to previous experiences; 44) Permits detailed analysis of information through graphics, data, etc.; 45) Permits reviewing compliance with strategy goals; 46) Permits review of pre and post implementation states. |
| Re-examination | 47) Gives implementation results, indicators and reports; 48) Allows to define new priorities; 49) Permits information interpretation; 50) Supports knowledge based decision-making. |
| Community diagnosis | 51) Identifies the population; 52) Identifies the population’s mobility capacity; 53) Manages individual and family demographic information; 54) Manages the distribution of the population to be intervened; 55) Permits to capture territory characteristics; 56) Permits registering family information; 57) Registers the community’s interests. |
| Decision in cases for action | 58) Administers resource availability; 59) Supports the selection of a set of problems to intervene; 60) Articulates the health plan; 61) Allows prioritizing attention to certain population segments; 62) Presents the study of health needs; 63) Presents the study of intervention costs; 64) Presents the available services in the community. |
| Surveillance | 65) Supports demographic surveillance (detection of population changes); 66) Supports monitoring and evaluation of health services; 67) Permits to carry out children follow-up and control; 68) Supports monitoring activities; 69) Supports to the population’s health state follow-up. |
| Program planning | 70) Characterizes the physical and demographic structures of the place the population dwells in; 71) Presents the study of physical, social, biological and psychological determinants of selected problems; 72) Performs activity planning. |
Source: the authors
The dimension of Health Information Technologies (HIT) includes features that represent systems functionalities; its capacity to facilitate the exchange of information among organizations by using interoperability standards and information standardized with terminologies, encodings and classifications; and software quality attributes.
The dimension of Health Services Organization includes features related to the standards of health service, which support the quality evaluation of services and safety of the patient; and the provision of health services, which takes into account assistance processes and administrative processes such as billing.
The dimension of PHC Reference Model includes features related to the management of information required to make diagnosis about the community, identify population risk, define access paths to the population, and assess social and biological determinants, among others.
The assessment of the level of compliance of HIS in PHC against the selected characteristics was accomplished through a quantitative evaluation of the information systems. This was done through a questionnaire with one question for each charac- teristic, that was graded according to the percentage of compliance (0 to 100 %); in addition, the information system that supports each characteristic was specified, with the particularity that the characteristics associated with the dimension of HIT were applied to all information systems used.
The verification procedure consisted of the instrument’s application by an evaluator or group of evaluators with knowledge of the three dimensions, namely: PHC/public health, organization of health services, and HIT. Each dimension required a specific role of the group in charge of the verification process. This procedure was performed after the implementation of the PHC strategy and on the HIS used therein.
The results of the assessment were obtained by analyzing the score of each charac- teristic and the average grouped by dimensions and subdimensions. The characteristics of the dimension of HIT were analyzed separately since their score was calculated for each information system used.
1.4. Validation of the characterization
The characterization validation was carried out by comparing results. To apply this method, a verification of the characteristics of HIS used in the implementation of a strategy of PHC by a health service provider institution was performed, and then the obtained results were compared against assessments, recommendations and reports related to PHC at a worldwide level (WHO) in countries similar to Colombia, in the same country, and at the same institution.
The verification of characteristics required an institution that had implemented a PHC strategy which would be willing to cooperate in the verification, and which also had experts in PHC, health services and HIT, the basic roles to meet the three dimensions defined by the characterization. The expert staff in primary care at the Departmental Health Secretariat of Cauca recommended to do the validation with the PHC strategy implemented in the municipality of Santander de Quilichao (Cauca, Colombia), led by the State Social Enterprise (in Spanish: Empresa Social del Estado, E.S.E.) Quilisalud. The verification was conducted by the Coordinator of the PHC strategy at the E.S.E., a professional nurse with a master’s degree in public health who served the first two roles, and the engineer in charge of the institution’s technological support and consequently of the implemented strategy, which was in charge of the third role.
2. RESULTS
2.1. Results of the verification of characteristics
The verification of characteristics in the PHC strategy of E.S.E. Quilisalud found that it was supported by a set of information systems that meet certain functionality in isolation. The used HIS were:
Health Information Management System, supported by DHIS2 [34].
Integrated Health Information System, in this case the system R-Fast [47], which includes electronic health records, billing and other caregiving and administrative modules used in the attention.
SISPRO [24], which corresponds to the unified national health information platform.
Spreadsheets, where specific attention data are collected and used for generating reports that are not supported by other systems.
The Health Observatory, which is the space for surveillance and monitoring of prioritized health indicators and includes the Health Situation Analysis (in Spanish: Análisis de Situación en Salud, ASIS), in each municipality and department in Colombia, as for example the Cauca department [48].
The total number of characteristics supported by these systems was 58, which represented 81 %. Table 6 shows the percentage of characteristics supported in each dimension by the used HIS, as well as the characteristics not supported by any system. It became evident that the main weaknesses were associated to the characteristics of the PHC Reference Model dimension, which represented 32 % of the characteristics without support.
Table 6 Percentage of characteristics supported in each dimension by the HIS of E.S.E. Quilisalud
| Dimension | DHIS (%) | R-FAST (%) | Sispro (%) | Observatory/ ASIS (%) | Spreadsheets (%) | Not supported (%) |
|---|---|---|---|---|---|---|
| Health Information Technologies* | 92 | 76 | 88 | 60 | 40 | 8 |
| Health Services Organization | 13 | 50 | 6 | 0 | 19 | 13 |
| PHC Reference Model | 32 | 6 | 3 | 3 | 23 | 32 |
*The characteristics associated to HIT are analyzed for each of the information systems applied
Source: the authors
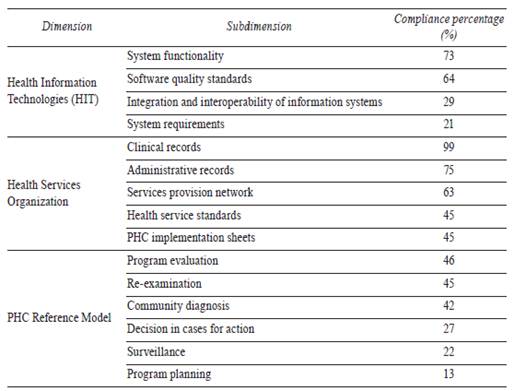
The subdimension ratings are shown in table 7; it can be observed that the used HIS obtained higher scores on the characteristics related to clinical and administrative records, but lower scores were obtained on characteristics related to program planning, surveillance, decision in cases for action, system requirements, and integration and interoperability.
2.2. Results of the characterization validation
The results obtained from the verification of the characteristics supported by the HIS used in the implementation of the PHC strategy of E.S.E. Quilisalud were compared with those published by several reports at national and international levels. Since the main purpose of verification is to identify aspects of HIS which require intervention to improve their support for PHC, the references to reports presented below have been focused on found weaknesses, which are highlighted in italics.
Perhaps the most important reference corresponds to the World Health Report 2008 [2], which is focused on PHC. This report collects the difficulties presented in the past and describes proposals for moving towards a renewed approach to PHC. In aspects related to HIS, it points out:
The waste of information at different levels, sometimes because data sources are not of public domain or outside the sector (integration and interoperability).
The focus of HIS on the identification of prioritized health problems and planning (decision in cases for action and program planning).
In an analysis of the adaptation of the Canadian model of PHC evaluation to the Latin American context [49], authors interpret as a conditional factor for achieving the objectives of PHC that information technologies (information systems according to the Canadian model) must be adapted to PHC and conclude that the application of any evaluation strategy will require developing indicators and instruments for information collection adapted to different contexts (system requirements).
In an evaluation of the health system and the strategy of PHC in Argentina [44], authors point out the lack of geo-referenced epidemiological information systems and systems for management registration. They consider that without this, information health systems will continue to be based on the traditional model of demand attention and propose a single health record system with epidemiological substrate, that facilitates the analysis at the local level with compatibility at higher levels (integration and interoperability); which is essential to make diagnosis, planning, monitoring and evaluation of policies and health programs (program planning, surveillance and decision in cases for action).
At the national level, in a study about the barriers encountered by nursing professionals for the implementation of the PHC strategy in Barranquilla [50], it was found that those concentrate in the planning and management actions of the PHC services. This situation affects the result of care processes due to factors such as: poor capability to identify problems and weaknesses in the integration of services, low cohesion of primary care teams, no use of tools for planning, management and evaluation. As a result, PHC is confused with the attendance of illnesses (surveillance and program planning).
In the description of the conceptual bases of the implementation process of the PHC strategy of E.S.E. Quilisalud [28], the author points out the need to integrate the different care levels and processes as reference and counter-reference (integration and interoperability), and have information systems that enable planning, monitoring and performance evaluation.
3. DISCUSSION
The proposed characterization identifies a set of essential features that HIS must offer to support PHC, organized by dimensions and subdimensions, plus the specification of roles and a verification process. With the result of verification, organizations may identify those aspects of HIS which require intervention to improve its support for the implementation of a PHC strategy.
A multidisciplinary team is required to perform this verification process, with knowledge in three specific fields: the PHC model, health services organization and health information technologies. This aspect has not been considered in the evaluations reported in literature, but that in the experience presented in this study turned out to be very enriching.
A first and essential step towards defining an evaluation mechanism for the support provided by HIS to the PHC strategies implementation is the determination of the model with which this implementation is contrasted. In the present study, the Community-Oriented Primary Care (COPC) model proposed by Dr. Kark, which describes an implementation cycle of eight phases (figure 1), has been chosen. This model follows the guidelines of Alma-Ata and is the most complete and referenced according to the literature review.
Due to time and resource constraints for the development of the project, the validation of the characterization proposed in this work was accomplished by a single case of comparison and the study of other PHC strategy implementations. Therefore, a more exhaustive validation is required to verify the completeness and relevance of the identified features. On the other hand, as the World Health Report 2008 argues that it is necessary to align health policies with PHC goals, since the priorities of the former can strengthen or undercut the latter [2], the type of health system determines some of the indicators that HIS must provide and defines who and how to use the information.
This aspect was not considered in the current proposal and therefore should be studied with the purpose of identifying new features that should be taken into account.
The verification process implemented in the E.S.E. Quilichao (Cauca, Colombia) evidences a high compliance of the used HIS with the characteristics of the health services organization dimension, mainly electronic health records and administrative management; but at the same time it reveals the failure of this institution’s HIS to support PHC reference model dimension, a significant percentage of its characteristics were not supported by any system (32 %). This situation reflects the WHO/PAHO investigations published in documents such as the Declaration of Montevideo, where it is pointed out that both the health education and health systems are focused on disease and diagnosis, leaving aside promotion, prevention and community participation in health care processes, which is the essence of PHC [51-52].
The comparison of results evidenced a great correspondence among the weaknesses identified in the PHC strategy of E.S.E. Quilisalud with the limitations reported by the cited studies. On the other hand, with the collaboration of the E.S.E. Quilisalud staff acting as experts, supported in turn by the information systems team of the Cauca Departmental Health Secretariat, it was possible to establish that the proposed characterization involves the most relevant features that information systems which support PHC strategies must comply to.
4. CONCLUSIONS
A set of 72 essential characteristics that HIS must offer to support PHC is proposed, plus the specification of the process and roles required to verify them. As a fundamental reference for contrasting these characteristics, the COPC model is adopted.
The applicability of the obtained characterization is determined mainly by the alignment of PHC implementations with the COPC model. Since this model is the most complete and accepted according to literature, it can be reasonably expected that characterization is applicable to a large number of PHC implementations.
Although identification of weaknesses in HIS constitutes an important step to make the necessary adjustments, the design of an improvement plan requires a more formalized evaluation of the information systems. Therefore, on the basis of the obtained characterization, the development of an evaluation methodology is under work and it takes into account the following aspects: