Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Ciencias de la Salud
Print version ISSN 1692-7273On-line version ISSN 2145-4507
Rev. Cienc. Salud vol.7 no.2 Bogotá May/Aug. 2009
The pattern of fall of serum bilirubin after operative relief of obstructive jaundice. A preliminary report
Perfiles de caída de la bilirrubina sérica luego de corrección quirúrgica de la ictericia obstructiva
David O. Irabor, MD1
1. Fellow of the West African College of Surgeons (FAWACS) College of Medicine, University of Ibadan, Nigeria. Department of Surgery, University College Hospital Ibadan, P.M.B. 5116 Ibadan, Nigeria. Correo electrónico: dirabor@comui.edu.ng.
Recibido: marzo 24 de 2009 Aceptado: mayo 29 de 2009
Summary
This is the beginning of a prospective study on patients who have obstructive jaundice to see how the serum bilirubin falls after operative relief of the obstruction. Seven of such patients have been studied; four had carcinoma of the head of the pancreas while the other three had choledocholithiasis. The patients with carcinoma had relief of the jaundice through a biliary -enteric anastomosis and those with common bile duct stones had choledochotomy with stone extraction which was completed with insertion of a T-tube. Serial bilirubin estimations were then performed post-operatively to chart the pattern and rate of descent of this in each patient. Our observations suggest that the pattern of fall of serum bilirubin after successful decompression of the extra-hepatic biliary tree exhibit a distinct pattern regardless of the surgical procedure performed for the relief of the obstruction.
Key words: serum bilirubin, obstructive jaundice.
Resumen
El presente artículo es el reporte preliminar de un estudio prospectivo de pacientes con ictericia obstructiva, que evalúa la disminución progresiva en los niveles séricos de bilirrubina luego de la corrección quirúrgica de la obstrucción. El estudio incluye 7 pacientes, 4 de ellos con carcinoma en la cabeza del páncreas y los 3 restantes cursaron con coledocolitiasis. Los pacientes con carcinoma fueron sometidos a una anastomosis bilio -entérica con el fin de corregir la ictericia, mientras que los pacientes con cálculos en el conducto biliar fueron sometidos a coledocotomía, extracción de los cálculos biliares e inserción de un tubo en T. Posteriormente, se realizaron numerosas cuantificaciones de los niveles de bilirrubina en suero, para determinar el patrón y la taza de descenso de dichos niveles en cada paciente. Los resultados muestran el patrón de caída de los niveles séricos de bilirrubina luego de la desobstrucción exitosa de las vías biliares extrahepáticas. Tres pacientes mostraron un patrón aberrante a pesar del correcto procedimiento quirúrgico.
Palabras clave: bilirrubina sérica, ictericia obstructiva.
INTRODUCTION
In the majority of health centers in Nigeria (Tertiary centers inclusive), pre-operative diagnosis of surgically-amenable hepatobiliary disease is possible, however post-operative assessment, especially those treated for obstructive jaundice, is difficult. Knowing the adequacy of a biliary -enteric anastomosis in the early post-operative period is essential in forestalling delays in re-operation in those anastomoses that fail to decompress the hepatobiliary tree.
An appropriate imaging technique for assessing the adequacy of a biliary -enteric anastomosis is a radioisotopic HIDA scan (1-2). This has the advantage of not being severely limited by the level of serum bilirubin the way an intravenous cholangiogram (which is available in many centers) is limited (3-5). Unfortunately very few tertiary centers possess facilities for HIDA -scanning, and the expense is beyond most hospital patients in this country (3).
By knowing the particular signature, so to speak, of an adequate biliary -enteric drainage through simple serial bilirubin estimations postoperatively, one may pick in time those who will require re-operation before they deteriorate.
MATERIALS AND METHODS
Seven adult patients with surgical (obstructive) jaundice were admitted over a period of 10 months onto the authors surgical unit.
Indices like age, sex, serum bilirubin, alkaline phosphatase, common bile duct diameter on ultrasound scan, Prothrombin time ratio and packed cell volume were recorded pre-operatively. Subsequently standard pre-operative preparation for obstructive jaundice patients were carried out in all the patients. These include low protein/high carbohydrate/no fat diet, bowel preparation, vitamin K injections, rehydration with normal saline infusion and procurement of mannitol infusion, 3rd generation cephalosporins, fresh frozen plasma and fresh whole blood for use in theatre.
Operative treatment was through a wide right subcostal incision. Those with common bile duct stoned had cholecystectomy, choledochotomy, extraction of stones with Desjardin forceps, irrigation of the extra-hepatic biliary tree with sterile saline, and this was completed with insertion of a T-tube. The 4 patients with carcinoma of the head of the pancreas had a loop cholecystojejunostomy and jejunojejunostomy. All the patients had closed tube subhepatic drains inserted which exited through separate stab wounds in the flank and were connected to drainage bags.
Post-operatively, intravenous ceftriaxone and metronidazole were continued for 5 days. Adequate pain control was by intramuscular injections of pentazocine. Satisfactory hourly urine outputs were ensured by adequate hydration. Serum bilirubin levels were requested for every 2 days and the effluents from T-tubes and/ or subhepatic drains were recorded daily. This line of management continued until the effluent from each subhepatic drain was less than 50mls daily and/or when T-tube cholangiograms done on the 10 th post-operative day showed flow of contrast into the duodenum and no evidence of retained stones.
RESULTS
There were 7 patients observed in this study. Four patients had carcinoma of the head of the pancreas (CAHOP); 3 males and 1 female. The three patients with ductal stones were all females.
The age range was 36 to 81 years. Five of the patients were in the sixth decade.
The total serum bilirubin ranged from 7.1 to 24.2 mg% with the majority between 11.5 to 17.1 mg% (5 patients). (Table 1) The conjugated bilirubin levels were between 3 to 17.6 mg% with a mean level of 11.6 mg%
The diameter of the common bile duct as measured on ultrasound scan ranged from 9 to 20mm with a mean of 14.3mm. The patient who had the widest common bile duct had the highest serum bilirubin level; this was a patient with carcinoma of the head of the pancreas.
The packed cell volumes (PCV) of the patients at presentation ranged between 25% and
42%, most were between 33-38% with only one patient having a PCV of 25%.
The Prothrombin time (PT) ratios were between 0.9 and 2.3. The patient with the lowest PCV (25%) had the most deranged PT (2.3).
The alkaline phosphatase levels were elevated in all the patients. The lowest level was 241iu/l while the highest was 2850iu/l.
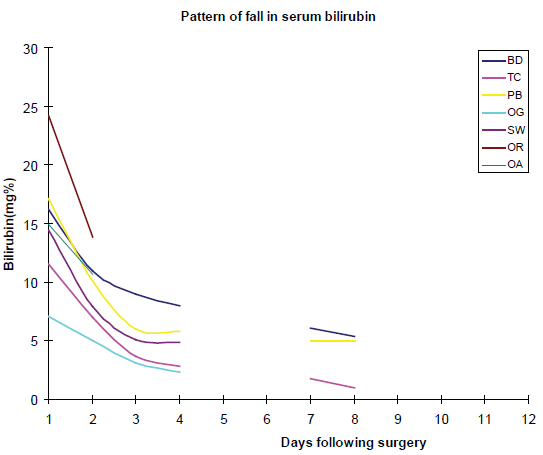
The observed pattern of reduction or fall in the serum level of bilirubin was that in all 7 patients there was an initial precipitous drop of roughly 2/3 rd of the presenting value by the 2 nd post-operative day. There was then a gradual decline up to the 7 th post-operative day when the measured levels were one-thirds of the presenting value and by the 14 th day the serum bilirubin was roughly one-fifths of the value at presentation. (Table 2, Figure 1)
The alkaline phosphatase levels did not fall proportionately with the serum bilirubin and levels stayed high for upwards of 2 weeks after surgery before a significant fall was observed, even after the jaundice had significantly cleared.
There was one mortality; the 81 year-old man with carcinoma of the head of the pancreas who had a presenting total bilirubin level of 24.2 mg%. He died on the 16 th post-operative day in the intensive care unit from multiple organ dysfunction.
DISCUSSION
When the likely pattern of a disease process is known it makes its diagnosis fairly straightforward, likewise a return to normalcy after an illness usually follows fairly well-known predictable steps. This is why a post-operative complication is defined as a deviation from the expected path towards recovery after an operation. The seven patients in this study have been recorded to show certain post-operative patterns after a successful relief of extra-hepatic biliary obstruction and the pattern was distinct enough to focus attention on. This implies that by the 2 nd post-operative day one should request for a serum bilirubin, if the latest values are not roughly 2/3 rd of the pre-operative value one should start having suspicions and if by the 7 th post-operative day the new levels are not roughly one-thirds of the presenting value, one should consider re-operation (at least in the third world where Iminodiacetic (IDA) isotope scans may not be available).
An exhaustive search through Pubmed and Google scholar did not yield any other study which has alluded to this distinct pattern.
Other observations made included the fact that the severity of jaundice did not determine how wide the common bile duct (CBD) would be and also did not determine the degree of derangement in the Prothrombin time (PT) ratio. (Table 1)
The widest CBD diameter (20mm) was seen in a patient with carcinoma of the head of the pancreas (CHOP) who had the highest level of serum bilirubin (24.2mg% with a conjugated fraction of 17.6mg%). The 2nd highest CBD diameter, 19mm, was recorded for a 50 year-old patient with CBD stones; however her total serum bilirubin was 11.5mg% with a conjugated fraction of 8.6mg%
In patients with ductal stones, obstruction of the CBD by the stones may not be total thus reducing the backpressure required to dilate the CBD and also elevate the serum bilirubin. A certain amount of fibrous thickening of the CBD also occurs when stones are present and this may limit the extent of distensibility. This may vary from patient to patient depending on the number of times they have had cholangitis and the severity of such episodes. This may explain the variability in CBD size and level of jaundice especially in patients with stones.
Derangement of the PT ratio (value 2.3) was seen in only one patient with a total bilirubin of 14.4mg%. She was a 65 year-old female with CAHOP. On an ascending scale her bilirubin level was 3 rd from the bottom while the patient with the highest level of bilirubin (24.2mg %) did not have a significant derangement of his PT ratio; he was an 81 year-old patient with CAHOP also.
It is still unclear why derangement in clotting profile is not proportional to the level of serum bilirubin given the fact that increases in bilirubin levels from extrahepatic biliary obstruction are a function of time i.e. the longer the obstruction, the higher the bilirubin levels. One should then expect that the longer there is no production of vitamin K-dependent clotting factors from the obstruction, the worse the PT ratio should be.
However our observations have shown that this relationship does not hold. This has also been observed in a previous study (6).
The alkaline phosphatase levels were elevated in all the patients. However the elevations were not pari passu with the serum bilirubin.
Some authors have stated that these two parameters rise in a progressive and parallel manner to characterize extrahepatic biliary obstruction 5.
This was not our finding as it was observed that the two highest levels of alkaline phosphatase were not seen in the two highest bilirubin levels (Table 1). In addition, in the post-obstructive phase, the serum bilirubin fell much more rapidly than the alkaline phosphatase. The return of alkaline phosphatase to normal following relief of biliary obstruction has been found to be extremely variable. 2 Long after the hyperbilirubinemia has subsided, reduction of alkaline phosphatase may be modest, may remain 2 or more times higher than normal despite an apparently successful clinical result. 2 This observation has been adduced to the period of full recovery of the hepatocytes and cholangiocytes from the toxic effect of the pent-up bile which may apparently take up to 2 months after the jaundice has resolved (2,7).
The pattern of fall of serum bilirubin in the patients in this study was unique in spite of the small number of patients that one was motivated to put it on record. (Table 2 and Figure 1).
The effluent of bile draining from the Ttubes and/or subhepatic drains was between 1.5 to 4.5 liters with the mode around 2.3 liters, yet the pattern of fall of bilirubin seemed to be uninfluenced by the different amounts of bile lost to the exterior in the different patients.
It is on record that following relief of biliary obstruction there is frequently a prompt and major choleresis and bile volumes may exceed 4 liters per day. The secretion of this bile is under an altered physiological drive thus during the days following biliary drainage, the bile is of low bilirubin and bile salt concentration (2).
Many hepatobiliary surgeons would have noticed this when the deep green bile encountered during surgery is replaced by a strawcolored bile postoperatively. This is also related to the loss of the enterohepatic circulation of bile salts in addition to a slow return of the impaired liver to normal function (2).
The mortality in this study was the 81 yearold man with carcinoma of the head of the pancreas who had a presenting serum bilirubin of 24.2mg%. He died of multisystemic organ failure on the 18 th postoperative day. Mortality in patients having surgery for obstructive jaundice has been reported to be associated with high pre-operative levels of serum bilirubin especially above 17.7mg% (8).
Table 1: Parameters at presentation
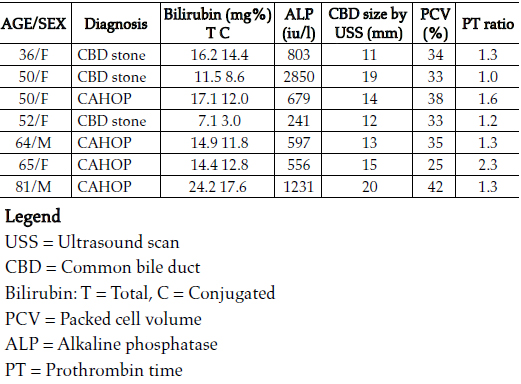
Table 2. Serial bilirubin values post-surgery
Figure 1: Graph showing pattern and rate of fall of serum bilirubin post-surgery
REFERENCES
1. Stadalnik RC, Matolo NM. Radionuclide imaging of the biliary tree. Surg Clin North Am. 1981;61(4):827- 42. [ Links ]
2. Benjamin IS. In: Blumgart LH (ed). Surgery of the liver and biliary tract. Vol.1, Chapter 10, Churchill Livingstone. Longman Group UK 1990. 115-117. [ Links ]
3. Lawal D, Oluwole S, Makanjuola D, Adekunle M. Diagnosis, management and prognosis of obstructive jaundice in Ile-Ife, Nigeria. West Afr J Med. 1998;17:255-60. [ Links ]
4. Berk RN. Radiology of the gall bladder and bile ducts. Surg Clin North Am. 1973;53(5):973-1005. [ Links ]
5. Badoe EA, Archampong EQ, da Rocha- Afodu JT (eds). Principles and practice of surgery including pathology in the tropics. 3 rd ed. Chapter 39, Archampong EQ. Liver and biliary system, Ghana Publishing Corporation. Tema. 2000. 685-721. [ Links ]
6. Irabor DO. The tendency towards a coagulation disorder in surgical jaundice: a retrospective analysis of some routine parameters. Pak J Med Sci. 2008;24: 479-82. [ Links ]
7. Koyama K, Takagi Y, Ito K, Sato T. Experimental and clinical studies on the effect of biliary drainage in obstructive jaundice. Am J Surg. 1981;142: 293-9. [ Links ]
8. Al- Fallouji MAR, Collins REC. Surgical relief of obstructive jaundice in a district general hospital. J Roy Soc Med. 1985;78: 211-6. [ Links ]














