Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Ciencias de la Salud
versión impresa ISSN 1692-7273versión On-line ISSN 2145-4507
Rev. Cienc. Salud v.9 n.1 Bogotá ene./abr. 2011
New Generation Antidepressants in Painful Diabetic Neuropathy
Antidepresivos de nueva generation en neuropatia diabetica dolorosa
Antidepressivos de nova geração na neuropatia diabetica dolorosa
Angela M. Gutierrez-Alvarez, MD-MSc1, Carlos B. Moreno, MD-EdM2
1 Servicio de Neurologia, Hospital Santa Barbara, Soria - Espana. Correspondence to: AM Gutierrez-Alvarez, e-mail: angelam.gutierrez@gmail.com
2 Grupo de investigacion NEUROS, Unidad de Neurociencia, Escuela de Medicina y Ciencias de la Salud, Universidad del Rosario, Bogota, Colombia.
Fecha recibido: octubre 26 de 2010 • Fecha aceptado: marzo 2 de 2011
Para citar este articulo: Gutierrez-Alvarez AM, Moreno CB. New Generation Antidepressants in Painful Diabetic Neuropathy. Rev. Cienc. Salud 2011; 9 (1): 33-42.
Abstract
The incidence of diabetic neuropathy increases with the duration of diabetes and the degree of hyperglycaemia. Pain is one of the most common and incapacitating symptoms of diabetic neuropathy and its pharmacological control is complex. The effectiveness of antidepressive agents has been described in different types of neuropathic pain, but their effectiveness, when used as analgesics in painful diabetic neuropathy, still remains controversial. Objective: To review the possible role of new-generation antidepressive agents in the treatment of pain in diabetic peripheral neuropathy. This work has thus consisted of a meta-analysis for determining which antidepressive agent had the best analgesic potential in managing pain in patients suffering from painful diabetic neuropathy. Methods: This search covered the Cochrane, MEDLINE, EMBASE and LILACS databases, between January 2000 and August 2007. The following information was obtained from each article: criteria for diagnosing diabetic neuropathy, patients' age average, antidepressant drug received and dose, sample size, duration of the disease and treatment follow-up, outcome measurement, evaluation of pain and rescue medication. Results: A combined RR: 1.67 (95% CI 1.38 - 2.02) was obtained; this result indicated that the antidepressive agent duloxetine, was effective for controlling pain in diabetic neuropathy. The corresponding NNT for Duloxetine was established, according to our interests; NNT = 6 (95% CI 5- 8) for achieving greater than 50% analgesia in patients suffering from painful diabetic neuropathy. Discussion: Antidepressive agents are frequently employed in the specific case of diabetic neuropathy; their analgesic benefit has been demonstrated.
Key words: "diabetic neuropathies", "pain", "antidepressive agents", "neuropathy", "meta-analysis"
Resumen
La incidencia de neuropatía diabética aumenta con la duración de la diabetes y el grado de hiperglicemia. El dolor es uno de los síntomas más comunes e incapacitantes de la neuropatía diabética y su control farmacológico es complejo. La efectividad de los antidepresivos ha sido descrita en diferentes tipos de dolor neuropático, pero su verdadera efectividad, al ser usados como analgésicos en el dolor en la neuropatía diabética, aún es controvertida. Objetivo: Realizar una revisión sistemática y meta-análisis para determinar el nivel de evidencia en relación con la potencia analgésica de estos nuevos antidepresivos para el manejo del dolor en el paciente con neuropatía diabética dolorosa. Métodos: La búsqueda cubrió las bases de datos Cochrane, MEDLINE, EMBASE y LILACS entre enero de 2000 y agosto de 2007. De cada artículo se obtuvo la siguiente información: criterios para diagnóstico de neuropatía diabética, edad promedio de los pacientes, antidepresivo recibido y dosis, tamaño de la muestra, duración de la enfermedad, seguimiento del tratamiento, medidas de desenlace, evaluación del dolor y medicación de rescate. Resultados: Se obtuvo un RR combinado de 1,67 (IC 95% 1,38 - 2,02). El NNT correspondiente para la Duloxetina fue de 6 (95% CI 5- 8), para obtener una analgesia superior a 50% en pacientes con dolor por neuropatía diabética. Discusión: Se ha demostrado que los antidepresivos son empleados con frecuencia y efectivos como analgésicos para el dolor por neuropatía diabética.
Palabras clave: Neuropatías diabéticas, dolor, agentes antidepresivos, neuropatía, metanálisis
Resumo
A incidência de neuropatia diabética aumenta com a duração da diabetes e o grau de hiperglicemia. A dor é um dos sintomas mais comuns e incapacitantes da neuropatia diabética e seu controle farmacológico é complexo. A efetividade dos antidepressivos tem sido descrita em diferentes tipos de dor neuropática, mas sua verdadeira efetividade, quando utilizados como analgésicos na dor na neuropatia diabética, ainda é controvertida. Objetivo: realizar uma revisão sistemática e meta-análise para determinar o nível de evidencia em relação com a potência analgésica destes novos antidepressivos para o manejo da dor no paciente com neuropatia diabética dolorosa. Métodos: A procura cobriu as bases de dados Cochrane, MEDLINE, EMBASE e LILACS entre janeiro de 2000 e agosto de 2007. De cada artigo se obteve a seguinte informação: critérios para diagnóstico de neuropatia diabética, idade em media dos pacientes, antidepressivo recebido e dose, tamanho da amostra, duração da enfermidade, seguimento do tratamento, medidas de desenlace, avaliação da dor e medicação de resgate. Resultados: obteve-se um RR combinado de 1,67 (IC 95% 1,38 - 2,02). O NNT correspondente para a Duloxetina foi de 6 (95% CI 5- 8), para obter uma analgesia superior a 50% em pacientes com dor por neuropatia diabética. Discussão: tem se demonstrado que os antidepressivos são empregados com freqüência e efetivos como analgésicos para a dor por neuropatia diabética.
Palavras chave: neuropatias diabéticas, dor, agentes antidepressivos, neuropatia, meta-análise.
Introduction
Diabetes mellitus is the most common cause of neuropathy (1, 2). It has been calculated that 20 to 30 million people in the world population are affected by symptomatic diabetic neuropathy1. The incidence of diabetic neuropathy increases with the duration of diabetes and the degree of hyperglycaemia (3, 4).
Pain is one of the most common and incapacitating symptoms of diabetic neuropathy and its pharmacological control is complex (5). The most used treatment for managing it consists of antidepressants, antiepileptics, opioids and topical lidocaine (6-8).
Tricyclic antidepressants used in optimum dose have been considered to be the most efficient medicaments for treating neuropathic pain (7, 9, 10); however, these medicaments have many associated risks, especially in elderly patients, due to adverse effects on the heart such as arrhythmias, tachycardia and myocardial infarction. Their anticolinergic effects also restrain their use in patients suffering from glaucoma and prostatic hypertrophy. It has also been mentioned that there is a higher suicide risk produced by tricyclic antidepressants than by other antidepressants (11). All these considerations limit their use in patients suffering from painful diabetic neuropathy, who are generally elderly, who require longtime treatment.
A new class of antidepressants has appeared on the pharmaceutical market during the last few years: selective serotonin reuptake inhibitors (SSRI) and serotonin and noradrenalin reuptake inhibitors (SNRI), which have potential analgesic properties and seem to have better tolerability and fewer secondary effects. In a prior review by Cochrane (12), which included the literature available up to December 2003, it was found that antidepressants were effective for managing neuropathic pain, greater evidence being found for amitriptyline, but with very limited data about the new generation antidepressants. Due to the increase of scientific literature on these new antidepressants in the last few years, it has been necessary to systematically and rigorously update their effectiveness in managing painful diabetic neuropathy, so that evidence-based clinical recommendations could be made. The objective of this work is to carry out a systematic review and a metaanalysis for determining the evidence level related to these new antidepressants' analgesic potential in the management of pain in patients suffering from painful diabetic neuropathy.
Methods
We have carried out search and systematic selection of all clinical assays concerning the analgesic treatment of diabetic neuropathy that have used new generation antidepressants and have been published from January 2000 trough February 2011. The search covered the Cochrane, Medline, EMBASE and LILACS databases, using combinations of the following MeSH terms: "diabetic neuropathy", "pain", "antidepressive agent", "duloxetine", "sertraline", "citalopram", "paroxetine", "fluoxetine", "venlafaxine", "fluvoxamine", "lofepramine", "milnazipram", "reboxetine", "sibutramine", "viloxacine", "mirtazapine", "nefazodone", "treatment outcome", "investigational therapy" "neuropathy" and "treatment". Clinical assays in adults aged 19 and older were established as being the only limits for the search. No limitation was placed regarding language. The search was carried out electronically; the titles and content of the summaries of corresponding articles were analysed. The complete text of those considered to be pertinent was obtained and all the references presented in each article were revised. The following journals were manually consulted for identifying other relevant articles: Acta Neurologica Scandinavica, Annals of Internal Medicine, Archives of Internal Medicine, BMJ, JAMA, Neurology, New England Journal of Medicine, European Journal of Pain, The Journal of Pain, Clinical Journal of Pain, Pain, Pain Medicine and The Lancet.
Random clinical assays compared with placebo were included which studied the analgesic effect of new generation antidepressants in adults suffering from painful diabetic neuropathy; they were evaluated so that improvement could be objectively classified. Studies that did not have relevant categorical measurements, case reports, summarised publications, and studies of treatment in research phase were excluded. All studies were independently read by each author involved in the present work and the validity of each assay included was evaluated based on five parameters: the method of assigning participants to an intervention within the study, blinding, follow-up, case definitions and clinical result. Any discrepancy was resolved by agreement amongst the authors. The following information was obtained from each article: criteria for a diagnosis of diabetic neuropathy, patients' average age, received antidepressant and dose, sample size, duration of the disease and treatment follow-up, outcome measurements, evaluation of pain, rescue medication and adverse side effects.
The data was placed in contingency tables in which the rows represented exposure (or not) to duloxetine and, in columns, the improvement (or not) of pain, since the variable response was binary. Effect measuring was defined as relative risk in these studies. The following tests were carried out: a) the DerSimonian and Laird and Galbraith plots for establishing homogeneity, b) a table of individual and combined results for the model of fixed and random effects and meta-analysis plots for combining results, and c) a funnel plot and the Begg and Egger's tests for publication bias. Epidat software (version 3.0, Pan-American Health Organisation, December 2003, a programme for the epidemiological analysis of tabulated data) was used for the meta-analysis.
The NNT (number needed to treat) value was calculated, as well as the 95% confidence interval (CI) based on the following formula:
NNT = 1/ARR
95% IC NNT = reciprocal of 95% IC ARR
95% IC ARR = ARR±1.96 SERR
where ARR = absolute reduction of risk.
Results
Seventeen publications concerning the use of latest generation antidepressants in managing pain in diabetic neuropathy using the methodology described here were found. The use of eight antidepressants for this type of pain was seen in these publications: four SSRI (citalopram, fluvoxamine, paroxetine, sertraline) and four SNRI (sibutramine, venlafaxine, nefazodone, duloxetine).
No evidence was found of milnacipran, reboxetine or viloxacine use in this pathology.
Fourteen of the 17 publications identified were eliminated for the following reasons:
-
7 were case reports related to using sertraline (13), fluvoxamine (14), sibutramine (15), nefazodone (16,17), venlafaxine (18,19) and duloxetine (20).
-
In two articles about the use of venlafaxine (21, 22) the follow-up period lasted only six weeks, in the study of Rowbotham et al. and the authors only reported the number of patients who improved using a high dose of the medication and the placebo (21). However, they did not report the patients who improved in other study groups. In the study of Kadiroglu et al., venlafaxine was compared to vitamins B1 and B6, not placebo (22).
-
Studies regarding venlafaxine (22, 23), citalopram (24), duloxetine (25-27) and paroxetine (24) did not provide sufficient categorical data for drawing up contingency tables, and they did not fulfil all the inclusion criteria.
Only three of the aforementioned publications fulfilled the inclusion criteria (28-30). These articles studied the analgesic effect of duloxetine in patients suffering from painful diabetic neuropathy, who were experiencing pain intensity equal to or higher than 4 on the 11-point Likert scale (0-10) and evaluated the patients during twelve weeks' follow-ups. The three studies allowed the concomitant use of acetaminophen as rescue medication, when necessary.
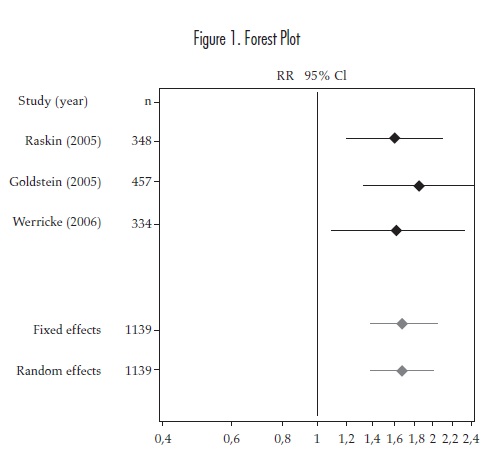
1,139 adult patients were included in this investigation from the three randomized clinical trials (RCTs) which investigated the analgesic effects of duloxetine. Patients were randomly assigned to the medication or placebo group in these studies. Variable response consisted of more than 50% pain improvement as measured on Likert's 11 point scale (0 - 10) and measuring the effect (relative risk). The results obtained when analysing them are shown in Table 1 and Figure 1.
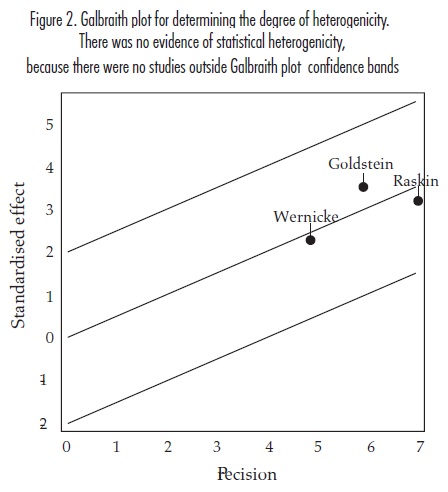
The Q test proposed by DerSimonian and Laird (31) was used to evaluate the degree of homogeneity and evaluate whether the results of the three studies could be summarised in a single measurement; this indicated that there was no statistical evidence of homogeneity (p=0.8059, Chi square 0.4315 with 2 df) having 95% level of confidence. This result corresponds with that observed in the Galbraith plot (Figure 2).
These studies all explicitly reported the number of patients who improved by more than 50% in dichotomous perception of pain(regarding base line) and evaluated pain improvement using very similar parameters.
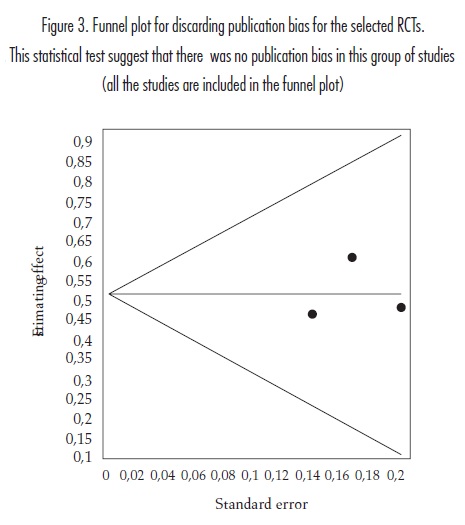
A funnel plot was used for discarding the existence of publication bias (Figure 3) and Begg (32) (p=0.5000, Z=0.0000) and Egger tests (33) (p=0.7359, t=0.4405 with 1 df) for contrasting the null hypothesis of the absence of publication bias.
Duloxetine NNT calculated from the results of the three studies was 5.4 with 95% CI (4.1-8.0). By convention, the NNT is rounded up to the next highest whole number NNT= 6 95% IC (5-8) (34).
Discussion
Painful diabetic neuropathy is a frequently occurring entity and its treatment is difficult. Traditional tricyclic antidepressants and antiepileptics have been mainly used for controlling pain (1, 11, 35). Unfortunately, tricyclic antidepressants have undesired effects in many patients, meaning that using a new class of antidepressants has been proposed, selective serotonin reuptake inhibitors (SSRI) and serotonin and noradrenalin reuptake inhibitors (SNRI) (8).
Among eight new generation antidepressants, only three clinical studies on duloxetine that fulfil the study inclusion criteria were found in this investigation, concerning the analgesic effect of these antidepressants in diabetic neuropathy. Studies regarding nefazodone, sertraline, venlafaxine, sibutramine, fluvoxamine, citalopram and paroxetine were found for the other antidepressants in this class, but none of them fulfilled study inclusion criteria.
A meta-analysis of the three duloxetine studies (28-30) was carried out for interpreting study results, specifically reporting 50% or more pain improvement as criterion for considering the clinical effectiveness of the antidepressant being used. They were also studies following similar methodology and having a minimum of 12-weeks' follow-up. Statistical homogeneity was shown in this group of studies (including 1,139 patients), as well as the absence of publication bias (Figure 2 and 3). A combined RR=1.67 (95% CI 1.38-2.02) was obtained (Table 01 and Figure 1). This result indicates that duloxetine was effective for controlling pain directly related to diabetic neuropathy in these patients, having a calculated NNT of 6 (95% CI 5-8). It has been suggested that this medicament's analgesic effect is related to the severity of the initial pain. Efficacy may even be enhanced in cases with relatively high pain intensity (36).
A systematic review prior to the appearance of duloxetine, with 251 patients affected by painful diabetic neuropathy, returned to 3.4 NNT (95% IC 2.6-4.7) for the antidepressants being evaluated (amitriptiline, clomipramine, desipramine, imipramine and maprotiline) (37). This NNT was lower than that obtained for duloxetine; however, due to methodological differences between both studies, valid conclusions cannot be drawn about duloxetine's analgesic effects regarding traditional antidepressants. Another latest generation antidepressant (venlafaxine) has a 4.5 NNT in 150-225 mg/day dose according to Rowbotham's study (21). This work was not included in our meta-analysis as it did not fulfil all the inclusion criteria (6-week follow-up only) and only mentioned the percentage of patients who reported lessened pain by over 50% in the high dose group, but not in the low dose group (as already mentioned). Kadiroglu's study (22), was also not included, as they compared venlafaxine to vitamin B complex; it also does not present the number of patients who lessened their pain, patients were taken as a group.
The most frequently described adverse effects associated with the use of duloxetine have been fatigue, nausea, hyperhydrosis and asthenia (38). The number needed to harm (NNH) could not be obtained for duloxetine in this investigation, as the studies reported the total number of adverse effects but did not by individual patient. Using antidepressants for managing neuropathic pain is basically limited for their adverse effects.
Given these conditions, there are few randomized clinical, double-blind, placebo-controlled trials measuring the analgesic effect of SSRI and SNRI antidepressants in diabetic neuropathy, there is also a lack of comparative studies on effectiveness and safety between two medicaments of this type. Therefore, the conclusions drawn here have to be preliminary and limited. Even though, there are some publications, a Cochrane review (39), a Post Hoc analysis (40), and another systematic review (41) that assessed the efficacy of duloxetine for neuropathic pain; they confirm the same NNT and calculated a NNH for duloxetine of 15 (95% CI 11-25) for side-effects leading to discontinuation of medication.
Managing pain in diabetic neuropathy, as we already said, is complex; around 30% of patients suffering from neuropathic pain do not respond adequately to monotherapy and require combined analgesic therapy (1) based on antidepressants and antiepileptics (11, 35). These patients also require control of hyperglycaemia and its complications, in order to avoid the neuropathy worsening, thus making pain management even more difficult (42).
Recent advances in research concerning the role of the immune response and inflammation in the onset of neuropathic pain have led to new possibilities for managing it therapeutically. Using tumor necrosis related factor-alpha (TNF-α) inhibitors would be an example of these promising treatment alternatives (43,44).
Conflicts of interest
There is no actual or potential financial or other conflict of interest related to the submitted manuscript
References
1. Said G. Diabetic neuropathy-a review. Nat Clin Pract Neurol 2007;3(6):331-40. [ Links ]
2. Kelkar P. Diabetic neuropathy. Semin Neurol 2005;25(2):168-73. [ Links ]
3. Llewelyn JG, Tomlinson DR, Thomas PK. Diabetic neuropathies. In: Dyck PJ, Thomas PK, eds. Peripheral neuropathy. Philadelphia: WB Saunders, 2005:1951 - 1991 [ Links ]
4. Sinnreich M, Taylor BV, Dyck PJB. Diabetic Neuropathies. Classification, clinical features and pathophysiological basis. Neurologist 2005;11(2):63-79. [ Links ]
5. Namaka M, Gramlich CR, Ruhlen D, et al. A treatment algorithm for neuropathic pain. Clinical Therapeutics 2004;26(7):951-79. [ Links ]
6. Gutiérrez-Álvarez AM, Beltrán-Rodríguez JA, Moreno CB. Antiepileptics in pain caused by diabetic neuropathy. J Pain Symptom Manage 2007;34(2):201-8. [ Links ]
7. Jackson II KC. Pharmacotherapy for neuropathic pain. Pain Pract 2006;6(1):27-33. [ Links ]
8. Dworkin RH, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: Evidence-based recommendations. Pain 2007;132(3):237-51. [ Links ]
9. Sindrup S, Jensen T. Efficacy of pharmacological treatments of neuropathic pain: An update and effect related to mechanism of drug action. Pain 1999;83:389-400. [ Links ]
10. Sindrup S, Jensen TS. Pharmacologic treatment of pain in polyneuropathy. Neurology 2000;55:915-20. [ Links ]
11. Dworkin RH, Backonja M, Rowbotham MC, et al. Advances in neuropathic pain: Diagnosis, mechanisms, and treatment recommendations. Arch Neurol 2003;60(11):1524-34. [ Links ]
12. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain (Cochrane Review). In: The Cochrane Library, Issue 1, 2006. Oxford: Update Software. [ Links ]
13. Goodnick PJ, Mendosa L, Kumar A, et al. Sertraline in diabetic neuropathy: Response and biology. Psychosom Med 2000;62(3):461-2. [ Links ]
14. Ogawa K, Sasaki H, Kishi Y, et al. A suspected case of proximal diabetic neuropathy predominantly presenting with scapulohumeral muscle weakness and deep aching pain. Diabetes Res Clin Pract 2001;54(1):57-64. [ Links ]
15. Davis JL. Use of sibutramine hydrochloride monohydrate in the treatment of the painful peripheral neuropathy of diabetes. Diabetes Care 2000;23(10):1594-5. [ Links ]
16. Goodnick PJ, Breakstone K, Kumar A, et al. Nefazodone in diabetic neuropathy: response and biology. Psychosom Med 2000;62(4):599-600. [ Links ]
17. Goodnick PJ, Breakstone K, Wen XL, et al. Acupuncture and neuropathy. Am J Psychiatry 2000;157(8):1342-3. [ Links ]
18. Kiayias JA, Vlachou ED, Lakka-Papadodima E. Venlafaxine HCl in the treatment of painful peripheral diabetic neuropathy. Diabetes Care 2000;23(5):699. [ Links ]
19. Lithner F. Venlafaxine in treatment of severe painful peripheral diabetic neuropathy. Diabetes Care 2000;23(11):1710-1. [ Links ]
20. Belgrade MJ, Cole BE, McCarberg BH, et al. Diabetic peripheral neuropathic pain: case studies. Mayo Clin Proc 2006;81(4 Suppl):S26-32. [ Links ]
21. Rowbotham MC, Goli V, Kunz NR, et al. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain 2004;110(3):697-706. [ Links ]
22. Kadiroglu AK, Sit D, Kayabasi H, Tuzcu AK, Tasdemir N, Yilmaz ME. The effect of venlafaxine HCl on painful peripheral diabetic neuropathy in patients with type 2 diabetes mellitus. J Diabetes Complications 2008;22:241-45. [ Links ]
23. Sindrup SH, Bach FW, Madsen C, et al. Venlafaxine versus imipramine in painful polyneuropathy: a randomized, controlled trial. Neurology 2003;60(8):1284-1289. [ Links ]
24. Giannopoulos S, Kosmidou M, Sarmas I, et al. Patient compliance with SSRIs and gabapentin in painful diabetic neuropathy. Clin J Pain 2007 Mar-Apr;23(3):267-9. [ Links ]
25. Wu EQ, Birnbaum HG, Mareva MN, et al. Cost-effectiveness of duloxetine versus routine treatment for U.S. patients with diabetic peripheral neuropathic pain. J Pain 2006;7(6):399-407. [ Links ]
26. Raskin J, Smith TR, Wong K, et al. Duloxetine versus routine care in the long-term management of diabetic peripheral neuropathic pain. J Palliat Med 2006;9(1):29-40. [ Links ]
27. Hardy T, Sachson R, Shen S, et al. Does treatment with duloxetine for neuropathic pain impact glycemic control? Diabetes Care 2007;30(1):21-6. [ Links ]
28. Raskin J, Pritchett YL, Wang F, et al. A double-blind, randomized multicenter trial comparing duloxetine with placebo in the management of diabetic peripheral neuropathic pain. Pain Med 2005;6(5):346-56. [ Links ]
29. Goldstein DJ, Lu Y, Detke MJ, et al. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain 2005;116(1-2):109-18. [ Links ]
30. Wernicke JF, Pritchett YL, D'Souza DN, et al. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Neurology 2006;67(8):1411-20. [ Links ]
31. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [ Links ]
32. Begg CB, Mazumbar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [ Links ]
33. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [ Links ]
34. Citrome L. Show me the evidence: Using number needed to treat. South Med J 2007;100(9):881-884. [ Links ]
35. Wong M, Chung JWY, Wong TKS. Effects of treatments for symptoms of painful diabetic neuropathy: Systematic review. BMJ 2007;335(7610):87. [ Links ]
36. Ziegler D, Pritchett YL, Wang F, et al. Impact of disease characteristics on the efficacy of duloxetine in diabetic peripheral neuropathic pain. Diabetes Care 2007;30(3):664-9. [ Links ]
37. Collins SL, Moore RA, McQuayHJ, et al. Antidepressants and anticonvulsants for diabetic neuropathy and postherpetic neuralgia: a quantitative systematic review. J Pain Symptom Manage 2000;20(6):449-58. [ Links ]
38. Wernicke JF, Wang F, Pritchett YL, et al. An open label 52-week clinical extension comparing duloxetine with routine care in patients with diabetic peripheral neuropathic pain. Pain Med 2007;8(6):503-513. [ Links ]
39. Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy or chronic pain. Cochrane Database Syst Rev 2009;(4):CD007115. [ Links ]
40. Kajdasz DK, lyengar S, Desaiah D, Backonja MM, Farrar JT, Fishbain DA et al. Duloxetine for the Management of Diabetic Peripheral Neuropathic Pain: Evidence-Based Findings from Post Hoc Analysis of Three Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Studies. Clin Ther 2007;29:2536-2546. [ Links ]
41. Sultan A, Gaskell H, Derry S, Moore RA. Duloxetine for painful diabetic neuropathy and fibromyalgia pain: Systematic review of randomised trials. BMC Neurology 2008, 8:29. [ Links ]
42. Nathan DM. The pathophysiology of diabetic complications: how much does the glucose hypothesis explain? Ann Intern Med 1996;124:86-9. [ Links ]
43. Arandjelovic S, Dragojlovic N, Li X, et al. A derivative of the plasma protease inhibitor alpha(2)-macroglobulin regulates the response to peripheral nerve injury. J Neurochem 2007 Oct;103(2):694-705. [ Links ]
44. Genevay S, Stingelin S, Gabay C. Efficacy of etanercept in the treatment of acute, severe sciatica: A pilot study. Ann Rheum Dis 2004;63(9):1120-1123. [ Links ]