Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Ciencias de la Salud
Print version ISSN 1692-7273
Rev. Cienc. Salud vol.11 no.1 Bogotá Apr./July 2013
Genotyping Klebsiella pneumoniae isolated from hepatic
abscesses in three patients from Bogota, Colombia
Genotipificación de Klebsiella pneumoniae aislada de abscesos hepáticos de pacientes de Bogotá, Colombia
Genotipificação de Klebsiella pneumoniae isolada de abscessos hepáticos de pacientes de Bogotá, Colômbia
Dora I. Ríos, Mic1, Luisa F. Tobón, Bac1, Danys Amado, MD2, Juan M. Pardo, MD, Esp MI2, Arley Gómez, MD, PhD1
1 Faculty of Science and Mathematics, Universidad del Rosario.
Correspondencia: dora.rios@urosario.edu.co
2 School of Medicine and Health Sciences, Universidad del Rosario.
Recibido: septiembre 14 de 2012 • Aceptado: febrero 28 de 2013
Para citar este artículo: Ríos DI, Tobón LF, Amado D, Pardo JM, Gómez A. Genotyping Klebsiella pneumoniae isolated from hepatic abscesses in three patients from Bogota, Colombia. Rev Cienc Salud 2013; 11 (1): 135-143.
Abstract
Pyogenic liver abscess caused by Klebsiella pneumoniae represents an ever increasing entity which has mainly been described as occurring in Asia, even though, on a smaller scale, cases are being more frequently described from the USA and Europe, 13% overall mortality being reached worldwide. Affected patients are severely sick, suffering from fever, sweating, having increased acute phase reactants and risk factors such as Diabetes Mellitus, alcoholism and the inherent characteristics of the bacteria causing the disease. Objective: in this work we used a Multilocus Sequencing Typing (MLST), a nucleotide sequence-based method in order to characterize the genetic relationships among bacterial isolates. Materials and methods: the report is focused on three cases involving patients suffering from pyogenic liver abscess caused by Klebsiella pneumoniae in two hospitals in Bogota, Colombia, where phenotyping and hypermucoviscosity studies were carried out, as well as the genotyping of cultured Klebsiella isolates. Results: it was found that the isolated microorganism in cases I and II corresponded to the same K. pneumoniae strain, having 100% sequence identity for the 5 genes being studied while the strain in Case III was genotypically different. Conclusion: it is important to carry out multidisciplinary studies allowing all pyogenic liver abscess cases reported in Colombia to be complied to ascertain the frequency of microorganisms causing this pathology in our country, as well as a genotyping study of different K. pneumoniae strains to compare them and confirm clonal and pathogenicity relationships through housekeeping gene analysis.
Keywords: pyogenic, liver abscess, hypermucoviscosity, Klebsiella pneumoniae, K1 capsular serotype, multi-locus sequence typing.
Resumen
El absceso hepático piógeno causado por Klebsiella pneumoniae representa una entidad descrita con frecuencia en los países asiáticos y, en menor escala, también en Estados Unidos y Europa. En el ámbito mundial su mortalidad alcanza a un 13%. Los pacientes pueden presentar un compromiso severo, el cual cursa con fiebre, sudoración y aumento de reactantes de fase aguda, sobre todo en individuos con factores de riesgo como la diabetes mellitus y el alcoholismo, además de las características inherentes de la bacteria responsable de la infección. Objetivo: a continuación se presentan tres casos de pacientes con absceso hepático piógeno causado por Klebsiella pneumoniae en dos hospitales de Bogotá. Materiales y métodos: se realizó caracterización molecular de los aislados de Klebsiella mediante la técnica de Multilocus Secquence Typing (MLST), análisis fenotípicos y de hipermucoviscosidad. Resultado: se encontró que el microorganismo aislado en los casos I y II corresponde a la misma cepa de K. pneumoniae, que tiene 100% de identidad de secuencia de los 5 genes en estudio mientras que la cepa en Case III fue genotípicamente diferente. Conclusión: es importante llevar a cabo estudios multidisciplinarios que incluyan todos los casos de abscesos hepáticos piógenos reportados en Colombia con el objeto de determinar la frecuencia de los microorganismos causantes de esta patología en nuestro país, así como un estudio de genotipificación de diferentes cepas de K. pneumoniae para confirmar las relaciones clonales y de patogenicidad.
Palabras clave: piógeno, absceso hepático, hipermucoviscosidad, Klebsiella pneumoniae, serotipo capsular K1, tipificación por secuencias de multilocus.
Resumo
O abscesso hepático piogênico causado por Klebsiella pneumoniae representa uma entidade descrita com frequência nos países asiáticos e, em menor escala, também nos Estados Unidos e na Europa. No âmbito mundial sua mortalidade alcança um 13%. Os pacientes podem apresentar um compromisso severo, o qual cursa com febre, sudoração e aumento de reagentes de fase aguda, especialmente em indivíduos com fatores de risco como a diabetes mellitus e o alcoolismo, além das características inerentes da bactéria responsável da infecção. Objetivo: a continuação apresentamse três casos de pacientes com abscesso hepático piogênico causado por Klebsiella pneumoniae em dois hospitais de Bogotá; Materiais e métodos: realizou-se caracterização molecular dos isolados de Klebsiella mediante a técnica de Multilocus Secquence Typing (MLST), análises fenotípicas e de hipermucoviscosidade. Resultado: encontrou-se que o micro-organismo isolado nos casos I e II corresponde à mesma cepa de K. pneumoniae, que tem 100% de identidade de sequencia dos 5 genes em estudo enquanto a cepa no caso III foi genotipicamente diferente. Conclusão: é importante levar a cabo estudos multidisciplinares que incluam todos os casos de abscessos hepáticos piogênicos reportados na Colômbia com o objeto de determinar a frequência dos micro-organismos causadores desta patologia em nosso país, assim como um estudo de genotipificação de diferentes cepas de K. pneumoniae para confirmar as relações clonais e de patogenicidade.
Palavras chave: piogênico, abscesso hepático, hiper-mucoviscosidad, Klebsiella pneumoniae, sorotipo capsular K1, tipificação por sequências de multilocus.
Hepatic abscess is a common cause of intraabdominal infection that can be single (58%) or multiple (42%), more frequently affecting the right lobe, leading to a lethal outcome in 8% to 31% of cases; such number has decreased thanks to the use of new diagnostic and therapeutic techniques such as percutaneous drainage.
Multiple etiologic agents can cause a hepatic abscess. The most frequent causal agent of acquired pyogenic liver abscess (PLA) in the community until the end of the last century was Escherichia coli; however, PLA caused by Klebsiella pneumoniae has increased in frequency during the last twenty years given the greater number of reported cases affecting adult patients (1). Patients suffering from K. pneumoniae-associated PLA frequently experience concomitant diseases such as type 2 Diabetes Mellitus and alcoholism (1, 2).
K. pneumoniae is a worldwide-distributed Gram-negative bacillus from the Enterobacteriaceae family which is associated with community-acquired or nosocomial infectious pathologies, such as urinary tract infections (UTI), bacteremia, pneumonia and intra-abdominal infections (3-5). The acquired invasive syndrome caused by this pathogen was described in 1981, being characterized by bacteremia, hepatic abscess and metastatic infections, among which endophthalmitis and central nervous system infections (manifested as suppurative meningitis or cerebral abscess were the most frequently found, although other abscesses in the lungs, pleura, prostate and soft tissues, like osteomyelitis and necrotizing fasciitis, have also been reported (6-8).
The pathogenic mechanism of K. pneumoniae is not fully understood. These bacteria possess a capsule formed by polysaccharides that have allowed their classification into 77 different capsular serotypes, from which K1 and K2 (associated with hypermucoviscosity) are the most frequently found, being associated with hepatic abscess cases (3, 9, 10). More than 900 cases of hepatic abscess have been reported worldwide to date, especially in Asia and eastern countries, although some reports from Europe and North America can be found (11, 12). There are no descriptions of this entity to date in Latin-America, particularly in Colombia; the present ones are the first reports from this continent to be described.
Case presentation
Case I report
A 34 year-old male attended the emergency room with a 5-day history of fever, generalized myalgia and intense migraine, accompanied afterwards by minimum effort dyspnea. As relevant background, the patient had suffered from type 2 Diabetes Mellitus which had been diagnosed 2 years before and he was currently being treated with metformin and insulin. Physical examination revealed that the patient was hypotensive, tachycardic, had marked mucocutaneous paleness, rales and a decrease in respiratory sounds on the right pulmonary base. During abdominal examination the patient presented pain on palpation of the upper right quadrant and epigastrium, without presence of ascites or hepatomegaly. A CBC was taken which showed normal leucocytes with neutrophilia and thrombocytopenia, 376 mg/ dl glycemia.
Coagulation tests were normal and urinalysis showed pyuria and ketonuria. He had high levels in liver function tests, as well as arterial gases with metabolic acidosis. Chest X-ray showed consolidations in the right inferior lobe with pleural effusion. Diagnostic impressions were right basal pneumonia vs. dengue (considered due to the thrombocytopenia and the patient's geographical origin). Intrahospitalary treatment was initiated with intravenous liquids and ampicillin/sulbactam (sultamicillin). However, the patient continued to deteriorate, which is why the antibiotic was changed to cefepime and the patient was transferred to an intensive care unit (ICU) where assisted mechanical ventilation and vasopressor support were initiated. Thoracic and abdominal computerized scans were requested, revealing pleural effusion with subsegmental atelectasis; abdominal images suggested an 8 cm diameter hepatic abscess in segment VI, with heterogeneous material and gas inside, accompanied by small bowel distension. The viral panel as well as the HIV test was negative. Abundant hemopurulent material and gas were observed in ecography-guided hepatic abscess drainage. A sample was sent for culture from which an ampicillin/sulbactam-resistant K. pneumoniae extended-spectrum -lactamase (ESBL) (-) was isolated; infection management was then continued with cefepime, adding metronidazole to the treatment accompanied by continuous drainage of the abscess.
The patient started showing signs of a multisystemic compromise with oliguria, signs of acute kidney injury, higher leukocytosis and worsening of the metabolic acidosis, so dyalisis therapy was initiated and the antibiotics were changed to carbapenems. The leukocytosis decreased during the following 24 hours but accompanied by rapid onset of neurological deterioration. A fixed mydriasis was observed during the physical exam, with no reactivity to light and the absence of stem reflexes. A brain CT scan was requested which showed multiple focal hemorrhagic lesions, predominantly cortical in both hemispheres with perilesional edema; no abscesses were observed, nor herniation signs. A brain perfusion scintigraphy was then requested, which showed the absence of blood flow; brain death was diagnosed and the patient died.
Case II report
A 76 year-old female patient attended the emergency room with a 3 day-history of abdominal pain in the epigastrium which afterwards irradiated to the right hypocondrium, accompanied by emesis, nausea, asthenia, adynamia and non-quantified fever. The patient also had dysuria, polyaquiuria and mild pain upon hypogastrium palpation. As relevant background, the patient suffered from a type 2 Diabetes Mellitus diagnosed 10 years before, high blood pressure, dyslipidemia and a supracondylar amputation of the lower left limb caused by a chronic occlusive arterial disease. Physical examination revealed hepatomegaly, with pain on deep palpation of the upper hemiabdomen, Murphy's sign (-). A diagnosis of cholelithiasis with cholecystitis was considered and lower urinary tract infection as secondary diagnosis. Paraclinical studies showed leukocytosis and neutrophilia with normocytic normochromic mild anemia, normal platelets having a high erythrosedimentation rate. Renal function tests were normal, with electrolytes showing mild hipokalema, bilirubin and normal amylase levels with increased alkaline phosphatase. Urinalysis showed proteinuria, glycosuria, ketonuria, bacteriuria and leukocyturia. A hepatobiliar ecography was performed, revealing a 24-mm vesicular calculus without cholecystitis or hepatomegaly and normal intra- and extrahepatic biliary ducts.
The patient had an episode of melena and, therefore, an upper digestive tract endoscopy was requested, where a hiatal hernia without esophagitis and an atrophic chronic gastritis without recent bleeding signs were observed. An abdominal contrast CT scan was carried out due to abdominal pain persisting, which showed multiple hepatic parenchyma abscesses, the largest of them measuring approximately 150 x 140 mm compromising segments I, II, IVA and B, V and VIII, with a calcified gallbladder, as well as a non-complicated diverticular disease. A piperacillin/tazobactam treatment was initiated, but the patient developed hypotension, tachycardia, tachypnea and increased abdominal pain. Surgery was then performed where multiple hepatic abscesses were found, one of them being ruptured. 800 cc of purulent material from abscesses and 700 cc of free pus in the peritoneal cavity were drained. The patient was open-packing laparotomized and then transferred to an ICU in worsening conditions where she suffered a septic shock and severe metabolic acidosis refractory to treatment, requiring a high oxygen supply, mechanical ventilation and inotropic support. The patient then had an asystolic episode and, despite the CPR maneuvers conducted, she died.
Case III report
A 56 year-old male patient attended the emergency room with an 8 day-evolution non-quantified fever, associated with generalized abdominal pain and hyporexia. As relevant antecedents, he suffered from a type 2 Diabetes Mellitus on insulin management, controlled high blood pressure and a gastric ulcer that had started 4 years before. The patient had undergone a laparoscopic cholecystectomy 4 months before and had also been treated for alcohol abuse up to 2 years before the present incident.
Physical examination showed that the patient was febrile, diaphoretic, had a mild jaundice without hepatomegalia and lower limb edema with fovea. A hemogram was performed, showing leukocytosis with neutrophilia and severe thrompocytopenia, normal urinalysis, increased alkaline phosphatase, normal amylase, high protein C-reactive and glycemia levels, normal EKG and chest x-rays. Abdominal ultrasound showed ecogenicity changes in hepatic segments VI and VII suggestive of liquid collection, measuring 96 x 79 x 87 mm, compatible with a hepatic abscess, having normal intra- and extra-hepatic biliary ducts, and mild hepatic steatosis.
An abdominal CT scan was requested, showing a 91 x 83 x 108 mm hepatic abscess containing gas and a small amount of perihepatic free liquid, without biliary duct dilatation.
Diverticulitis as well as a 20 x 41 x 21 mm collection next to the rectosigmoid were observed. The attending surgeon considered that the findings did not require surgical intervention and could be handled with antibiotic therapy and a liver abscess percutaneous drainage.
New lab tests were taken which showed prolonged coagulation times, mild normocytic normochromic anemia and a decrease in the leukocytosis. 4 U of fresh frozen plasma with 2 red blood cell units were transfused. The abscess was drained, obtaining profuse purulent material and a transient catheter was placed.
A new abdominal CT scan was performed 48 hours later where a 74 x 48 x 85 mm residual collection was observed in segments V, VI and VII, with persistence of gas inside, peritoneal free liquid, associated with pleural effusion and adjacent parenchyma atelectasis. Percutaneous drainage was continued through the catheter. Cultures showed ampicillin and piperacillin-resistant Klebsiella pneumoniae. The patient was evaluated by the Infectious Diseases' department who decided to continue the ampicillin/sulbactam therapy for 14 days. The patient showed a good clinical evolution, without systemic inflammatory response signs, was hemodynamically stable and had suitable glycemia levels. The patient was discharged with recommendations.
Discussion
K. pneumoniae is a Gram-negative bacillus associated with different pathologies (4, 8, 13) in both community- and hospital-acquired settings (one of them being the invasive syndrome), characterized by the presence of hepatic abscesses (5, 8).
Different genes have been recently identified and related to K. pneumoniae virulence, such as wab G (gene implied in external core capsular polysaccharide biosynthesis), uge (uridine diphosphate galactose 4 epimeraseencoding gene responsible for capsule and smooth lipopolysaccharide synthesis), kfu (the gene involved in the iron uptake system), fim H (the type-1 adhesin encoding-gene), rmp A (a mucoid phenotype regulator) and mag A (a gene associated with mucoviscosity) (10, 14). Moreover, the presence of several of them has been associated with patients having liver abscesses in Taiwan, rmp A and mag A being the most frequently occurring ones, the latter being associated with K. pneumoniae hypermucoviscosity and high virulence (6, 15).
The K. pneumoniae pathogenicity mechanism is still not well understood; however, according to studies carried out by Lee et al, K1 and K2 serotypes are the most frequently occurring ones which are associated with cases of hepatic abscess, especially K1 (16, 17).
Metastatic infection occurs in 3% to 12% of all PLA patients. Diabetes Mellitus and alcoholism have been described as being risk factors. Alcoholism leads to decreased glutathione pulmonary concentration, followed by with an increase in alveolar barrier permeability which can explain the appearance of pulmonary lesions.
However, its direct infection mechanism has still to be established (5, 6, 10).
Another complication concerns spontaneous rupture of an abscess which is related to abscess size (greater than 7 cm), gas formation or location in the left lobe (7), with clinical alarm signs given by diffuse abdominal pain and the presence of septic shock. No particular strain type (K1 or K2) has been found to be associated with spontaneous abscess rupture incidence (6, 9).
To the extent of our knowledge, this is the first report of pyogenic liver abscess cases in Colombia, the phenotypic and hypermucoviscosity studies being of special interest, as well as the genotypic comparison of K. pneumoniae isolated strains. Phenotyping and genotyping studies were carried out to determine the clonal relationship among the K. pneumoniae strains responsible for liver abscesses, from purulent hepatic material samples taken from patients hospitalized in different geographical areas in Bogota, Colombia. K. pneumoniae isolates were obtained of clinical samples from the three cases. Culture was performed on enriched media such as sheep blood agar. Unique colonies were observed with a mucoid appearance. Phenotype identification was done by an automated microbiological identification system (Biomerieux.vitek®2 system).
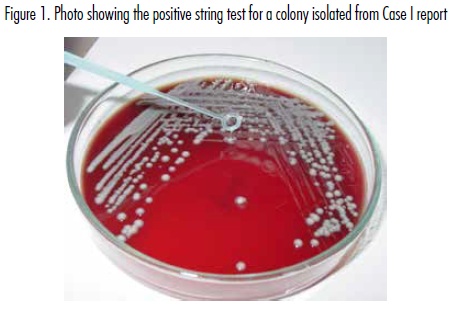
The hypermucoviscosity test was carried out on mucoid-aspect colonies using 24 hour incubation cultures in a 5% sheep blood agar medium; colonies were stretched using a loop. This test, also known as "string", is positive if there is a ≥ 5 mm long vertical string attached to the loop from the surface. The string test was positive for Klebsiella strains isolated from Case I and Case II, but negative for the isolate from Case III (figure 1).
Klebsiella strains were kept in BHI medium with 15% glycerol at -80°C for further genomic DNA extraction and genotypic study. Samples were genotyped using the multilocus sequence typing (MLST) technique. Five housekeeping genes were amplified by PCR from the extracted genomic DNA using a high fidelity polymerase (Pfx) for the following genes: rpo B (RNA polymerase, subunit B), gyr A (DBA, gyrase subunit A), gap A (glyceralde-hyde-3-phosphate dehydrogenase A), gyr B (DBA, gyrase subunit B), and omp A (outer membrane protein A). Each reaction contained 10x amplification buffer (Invitrogen), 50 nM MgSO4, 10 mM dNTP mix, 10 mM of each primer, 1U platinum Pfx DNA polymerase and 10-40 ng of DNA in a final 25 µL volume. The amplification conditions used were: one 3 min cycle at 95°C, 35 cycles consisting of: 58°C for 1 min, 68°C for 90 sec and 95°C for 1 min; a final cycle at 58°C for 1 min, followed by an extension step for 5 min at 68°. PCR products were purified using the Wizard PCR preps kit (Promega®) following the manufacturer's recommendations. Sequencing was carried out in both directions using the corresponding primer set and the BigDyeTerminator system (Macrogen®, Seoul, South Korea). Sequences were assembled using CLC DNA workbench 5 software (CLC bio®, Cambridge, MA, USA). A complete alignment was carried out for each gene using sequences from three samples (Case I: liver abscess sample, Case II: blood culture sample, Case III: hepatic drainage sample) using Clustal W software. Two PCR products from independent PCR amplifications were sequenced to avoid polymerase errors. A K. pneumoniae strain purchased from ATCC was used as control in all experiments.
It was found that the isolated microorganism in cases I and II corresponded to the same K. pneumoniae strain, having 100% sequence identity for the 5 genes being studied while the strain in Case III was genotypically different (table 1). These findings were related to the genotypic study which showed 88%-96% nucleotide identity regarding the former two strains, thereby classifying it as being a different strain.
K. pneumoniae-associated hepatic abscess was previously considered to be a rare disease, more frequently occurring in Asia; however, more reports have been emerging from North America, thus making it an emerging pathology nowadays. Diabetes Mellitus has been the main risk factor in all pertinent literature reviews, and appeared to be a constant in our patients. Alcoholism was also found in one case which can increase frequency.
The clinical presentation is also unspecific, fever being a common factor in all reviews and in our series, accompanied by superior hemiabdomen pain, shivers, nausea and vomiting, as common findings. Other symptoms have variable presentation and are often confused with other pathologies. The main complications involve metastatic infection of other organs, such as endophthalmitis, cerebral or prostatic abscesses, or pulmonary dissemination. These complications occur most frequently in K. pneumoniae rather than other hepatic abscess causative germs. Mortality has dropped from 50% to 13% when suitable and early treatment is applied, as well as with percutaneous drainage of the abscess (11-16).
It would be very interesting to carry out multidisciplinary studies allowing all pyogenic liver abscess cases reported in Colombia to be complied to ascertain the frequency of microorganisms causing this pathology in our country, as well as a genotyping study of different K. pneumoniae strains to compare them and confirm clonal and pathogenicity relationships through housekeeping gene analysis.
Acknolwledgement
The authors express the deep gratitude to doctor Manuel Alfonso Patarroyo from Fundación Instituto de Inmunología de Colombia (Fidic), for his kind support in reviewing the molecular biology aspects and the written version of this manuscript and the microbiological labs from Fundación Cardioinfantil and Hospital Mederi for their support by providing the clinical samples.
Disclaimers
The authors declare no conflict of interest in this manuscript. This research was funded by the University of Rosario and Institute of Immunology Foundation of Colombia (Fidic), Bogota.
Bibliography
1. Keynan Y, Rubinstein E. The changing face of Klebsiella pneumoniae infections in the community. Int J Antimicrob Agents 2007; 30 (5): 385-9. [ Links ]
2. Chen S-C, Lee Y-T, Lai K-C, Cheng K-S, Jeng L-B, Wu W-Y et al. Risk factors for developing metastatic infection from pyogenic liver abscesses. Swiss Med Wkly 2006; 136 (7-8): 119-26. [ Links ]
3. Lederman ER, Crum NF. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol 2005; 100 (2): 322-31. [ Links ]
4. Tsai F-CHuang YT, Chang LY, Wang JT. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis 2008; 14 (10): 1592-600. [ Links ]
5. Siu LK, Yeh KM, Lin JC, Fung CP, Chang FY. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis 2012; 12 (11): 881-7. A [ Links ]
6. Kawai T. Hypermucoviscosity: an extremely sticky phenotype of Klebsiella pneumoniae associated with emerging destructive tissue abscess syndrome. Clin Infect Dis 2006; 42 (10): 1359-61. [ Links ]
7. Ko W-C, Paterson DL, Sagnimeni AJ, Hansen DS, Von Gottberg A, Mohapatra S et al. Community-acquired Klebsiella pneumoniae bacteremia: Global differences in clinical patterns. Emerg Infect Dis 2002; 8 (2): 160-6. [ Links ]
8. Fang FC, Sandler N, Libby SJ. Liver abscess caused by mag A+ Klebsiella pneumoniae in North America. J Clin Microbiol 2005; 43 (2): 991-2. [ Links ]
9. Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: Epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev 1998; 11 (4): 589-603. [ Links ]
10. Yeh K-M, Kurup A, Siu LK, Koh YL, Fung C-P, Lin J-C et al. Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J Clin Microbiol 2007; 45 (2): 466-71. [ Links ]
11. Lee C-H, Leu H-S, Wu T-S, Su L-H, Liu J-W. Risk factors for spontaneous rupture of liver abscess caused by Klebsiella pneumoniae. Diagn Microbiol Infect Dis 2005; 52 (2): 79-84. [ Links ]
12. Nadasy KA, Domiati-Saad R, Tribble MA. Invasive Klebsiella pneumoniae syndrome in North America. Clin Infect Dis 2007; 45 (3): e25-8. [ Links ]
13. Connell NT, Thomas IA, Sabharwal AD, Gelbard MA. Klebsiella pneumoniae endophthalmitis with associated hepatic abscess. J Hosp Med 2007; 2 (6): 442-4. [ Links ]
14. Suescún AV, Cubillos JR, Zambrano MM. Genes involucrados en la biogénesis de fimbrias afectan la formación de biopelículas por parte de Klebsiella pneumoniae. Biomedica 2006; 26 (4): 528-37. [ Links ]
15. Chang L, Bastian I, Warner M. Survey of Klebsiella pneumoniae bacteraemia in two South Australian hospitals and detection of hypermucoviscous phenotype and mag A/rmp A genotypes in K. pneumoniae isolates. Infection 2013; 41 (2): 559-63. [ Links ]
16. Yu W-L, Ko W-C, Cheng K-C, Lee C-C, Lai C-C, Chuang Y-C. Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/ K2 serotypes. Diagn Microbiol Infect Dis 2008; 62 (1): 1-6. [ Links ]
17. Shon AS, Bajwa RP, Russo TA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: A new and dangerous breed. Virulence 2013; 4 (2): 107-18. [ Links ]