Introduction
Stigma is one of the main reasons why people with severe mental disorder (SMD) avoid seeking professional help 1,2. This fact explains the gap in medical attention for these disorders, which vary between 32% of schizophrenia cases and 56% of depressive disorders 3. Some factors that contribute to this situation are the lack of knowledge and the presence of prejudice and discrimination, either real or anticipatory, toward people who suffer from these disorders 4-6. Furthermore, high-income countries have reported a prevalence of self-stigma >40%, while, in Latin America, a high prevalence of stigma has been reported in people with SMD. Mascayano reported that public stigma was 40.5-70% 7; this proportion increased to 50-90% for self-stigma 8. Therefore, there is a need to implement interventions to reduce stigma within the general population as well as within the mental healthcare profession and for those who suffer from SMD and their family members 9,10.
Considering the magnitude and impact of stigma, several strategies have been implemented for to reduce it over several decades 7,11,12. The three principal strategies include social protest, education, and contact. Social protest involves the uniting of people who share a specific diagnosis so as to demand changes in the situations that are harmful to them. Through this action, awareness can be raised about rejection and exclusion and individuals can advocate for their rights 10,13. Education is characterized by the distribution of information aimed at changing misperceptions, stereotypes, and discriminatory attitudes in various population groups 10,14. Finally, direct contact strategy usually involves a person with SMD sharing their experience with professionals, students, and other people in order to favor the interaction between those affected and other social groups 10,15-18. However, the methods used to reduce stigma in mental health that are aimed at the general population are diverse and employ mass media mediums such as radio, newspapers, television, or internet 17,19,20. In interventions with specific groups, information is provided through workshops led by mental health professionals, and written documents and presentation of real cases are provided to help people understand the disorder 14,17,18. In situations where direct experience by the mental health service user cannot be accessed, indirect contact is employed through the analysis of cases, videos, vignettes, or interaction via social networks 18.
Unfortunately, studies on the effectiveness of interventions have revealed several discrepancies and gaps. For example, some studies have found that direct and indirect contact are equally effective 12,21,22), while others have reported that direct contact is better 17,23,24. Concerning the duration of the effect, a recent review by Thornicroft concluded that the results obtained were not sufficiently strong to determine the effect of long-term interventions, warranting further research on the subject 17. In addition, depending on the target population, the interventions have different objectives and strategies that make their comparison difficult 25. For instance, interventions are aimed at modifying the attitudes and knowledge based on educational programs among healthcare professionals 4,17,24), they are intended to reduce self-stigma for patients 4,17, and they are mainly provided through mass media for the general population 26. Furthermore, strategies based on coping have been proposed for families and caregivers to reduce stigma by association 8,27. On the other hand, interventions such as social contact and psychoeducation have been used in high school students to improve the level of awareness 22,29.
In low- and middle-income countries, the lack of resources and poor capacity to develop research are the factors that limit the implementation and follow-up of interventions to reduce stigma in mental health 24. There are only a few precedents to these types of interventions in Latin America, therefore, studies that serve as reference for cultural proximity and language mainly arise from Spain and Portugal 8. Moreover, there is a history of reforms in the healthcare systems between these two countries similar to that developed or under development in Latin America, which include guidelines such as reduction in the number of hospital beds and the incorporation of community services geared toward primary healthcare attention 30-32. Therefore, the gaps in research regarding the reduction of stigma among Latin America pose a challenge concerning identifying common areas of interventions. The investigators and policy makers need a solid empirical basis about the characteristics and impacts of stigma in order to assure that stigma can be handled and reduced 33. Based on the abovementioned reports, this review was conducted to describe the characteristics and the main results of interventions toward reducing stigma developed in Ibero-America during 2007-2017.
Materials and methods
A systematic review of articles from electronic databases such as Medline, EBSCOhost, Embase, LILACS, and SciELO and gray literature from Google Scholar between January 2007 and December 2017 was conducted. Based on the Virtual Health Library, the following Health Sciences Descriptors (DeCS) were used: Social stigma OR Attitude OR Behavior OR Prejudice OR Discrimination OR Social Distance OR Social Perception, AND Mental Disorder OR Mood Disorder OR Schizophrenia OR Bipolar Disorder OR Substance-Related Disorders OR Mental Health AND Interventions, Program OR Health Literacy OR Education OR Health Promotion OR Training OR Cognitive Therapy OR Narrative Therapy AND Latin America AND Spain AND Portugal.
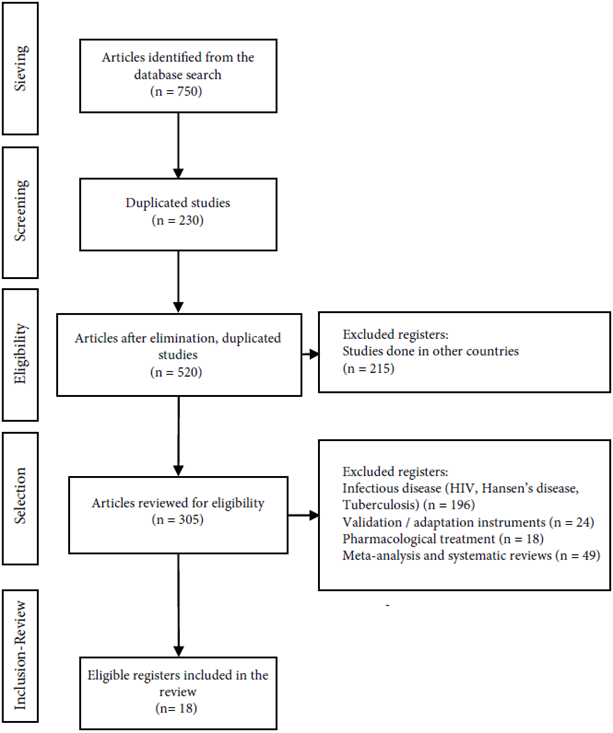
The inclusion criteria used were studies based on interventions to reduce stigma toward people with SMD, quantitative and qualitative studies, and studies performed in individuals aged >14 years that evaluated changes in knowledge, attitudes, and/or behavior as a primary or secondary variable. Publications from Ibero-America were selected in English, Spanish, and Portuguese. The publications that were excluded included those on protocols related to randomized controlled trials, studies on validation and cultural adaptation of instruments for stigma assessment, systematic reviews, meta-analyses, and studies related to common mental disorders and infectious diseases (Figure 1).
Two authors from the present study conducted independent searches and reviewed the abstracts for each publication in order to select those studies that met the inclusion criteria and discard those that met the exclusion criteria. In case of any discrepancies regarding adherence to the criteria between the authors, the opinion of a third expert evaluator was considered for arbitration.
The information was arranged in a descriptive database developed in Excel® with the purpose of being evaluated and refined by the authors in case of duplicate results. A synthesis of the study was performed, which included the country in which the research was conducted, the approach used, the type of study, the type of population, the number of participants, the strategy and duration of the intervention, and follow-ups (if any). The results for the analysis of each category are shown in Table 1.
Table 1 Summary of anti-stigma intervention studies in mental health conducted in Ibero-America during 2007-2017
| Year | Journal | Country | Article | Focus | Type of study and design | Type of population | Sample (n) | Intervention Strategies | Duration | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | Frontiers in Psychology | Spain | Stigma-Stop: A Serious Game against the Stigma toward Mental Health in Educational Settings | Quantitative | Experimental Randomized control clinical trial | High school students | 484 experimental group 68 control group | Education (videogame) | Medium-term (one weekly session for 3 months) | No follow-up |
| 2017 | Frontiers in Psychology | Spain | Effectiveness of the “What’s Up!” Intervention to Reduce Stigma and Psychometric Properties of the Youth Program Questionnaire (YPQ): Results from a Cluster Non-randomized Controlled Trial Conducted in Catalan High Schools “ | Quantitative | Quasi-experimental Clinical Trial by Cluster Non-randomized | High school students | 261 experimental group 132 control group | Education (information) Social Contact | Medium-term (Between 5 and 9 weeks) | No follow-up |
| 2017 | Revista Portuguesa de Enfermagem de Saúde Mental | Portugal | Fight against Stigma Program: results obtained in the training of mental health professionals | Quantitative | Quasi-experimental Pre - Post (One sample) | Professionals | 46 | Psychoeducation | Short (2 hours) | No follow-up |
| 2016 | Revista Asociación Española de Neuropsiquiatría | Spain | Effectiveness of an intervention of the community social support team in the psychosocial functioning of people with SMD | Quantitative | Quasi-experimental Pre - Post (one sample) | Mental health service users | 275 | Psychoeducation Multidisciplinary psychosocial intervention | Long-term (3 years) | Nine months |
| 2016 | World Journal of Psychiatry | Spain | Effectiveness of an intervention to reduce social stigma toward mental illness in adolescents | Quantitative | Experimental Randomized control clinical trial | High school students | 128 experimental group 152 control group | Education Video (documentary) | Short-term (one week) | One month after |
| 2015 | European Psychiatry | Spain | Impact of the OBERTAMENT mass media campaign on the levels of stigma among the population of Catalonia, Spain | Quantitative | Quasi-experimental Survey | General population be- tween 15 and 45 years | 1019 | Massive campaign | Medium -term (2 months) | Between 9 and 12 months |
| 2015 | Thesis | Spain | Modification of stigma associated with mental illness: evaluation of an intervention in compulsory secondary educational institutes in Navarra | Quantitative | Experimental (Thesis) Randomized control clinical trial | High school students | 106 experimental group 79 control group | Education information + Indirect contact | Long-term (6 months) | One week after |
| 2014 | Psicoperspectivas. Individuo y Sociedad | Spain | PsychoED: An online and community alternative for psychoeducation in schizophrenia | Quantitative | Quasi-experimental Combination | Families of people with schizophrenia | Traditional intervention 11 Online 7 Control 9 | 1. Traditional psychoeducation 2. Psychoeducation online | Long-term (9 months) | No follow-up |
| 2013 | World Journal of Psychiatry | Spain | Intervention for reducing stigma: Assessing the influence of gender and knowledge | Quantitative | Quasi-experimental | High school students | 28 women 34 men | Education information + Indirect contact (Experiences of mental health service users on video) | Short-term (2 weeks) | One month follow-up Six months follow-up |
| 2012 | Journal of Human Growth and Development | Brazil | Mental health awareness action in schools | Quantitative | Quasi-experimental Pre - Post (One sample) | High school students | 26 | Education (mental health promotion) | Short (2 sessions) | No follow-up |
| 2012 | Revista Portuguesa de Enfermagem de Saúde Mental | Portugal | Mental Health program on stigma: Effects of direct and indirect strategies on stigmatizing attitudes | Quantitative | Quasi-experimental Pre - Post (two samples) | High school students | Group 1: 437 Group 2: 298 | 1. Anti-stigma campaign (dissemination of information) 2. Education and contact | Medium-term 3 months | No follow-up |
| 2009 | Social Psychiatry and Psychiatric Epidemiology | Chile | Effects of a psychoeducational intervention program on the attitudes and health perceptions of relatives of patients with schizophrenia | Quatitative | Experimental Randomized control clinical trial | Informal caregivers | 18 experimental group 23 control group | Psychoeducation Family intervention | Medium-term (one weekly session for 18 weeks) | No follow-up |
| 2007 | Quality of Life Research | Chile | Effectiveness of a psychoeducational intervention for reducing burden in Latin American families of patients with schizophrenia | Quantitative | Quasi-experimental Pre - Post (two samples) | Informal caregivers | 22. experimental group 23. control group | Psychoeducation Family intervention | Medium-term (one weekly session for 5 months) | Five months |
| 2017 | eduPsykhé | Spain | “Inclúyete”: Socioeducational and inclusive program in people with severe mental students from the Universidad de Almería | Qualitative | Exploratory | Undergraduate students, general population | 200 | General information | Medium-term (a course per semester) | No follow-up |
| 2015 | Revista de la Facultad de Ciencias Médicas | Chile | Development of an intervention to reduce self-stigma in outpatient mental health service users in Chile | Qualitative | Feasibility study | Mental health service users | 80 | Group Psychoeducation | Medium-term (one 90 minute session for 10 weeks) | No follow-up |
| 2014 | Revista Colombiana de Psiquiatría | Argentina, Chile, Ecuador, Venezuela, Costa Rica, México, Uruguay, Colombia and Spain | “Accepting demented minds.” Opinion Group, information and support group on stigma of mental illnesses on Facebook | Qualitative | Group case study | Mental health service users and families | 764 | Education information + videos + comments | Long-term (3 years) | Follow-up at 6 months Follow-up at 30 months |
| 2012 | Arteterapia: Papeles de arteterapia y educación artística para la inclusión social | Spain | A visit against stigma and pro prevention in a treatment unit for serious mental illness | Qualitative | Group case study | Nursing Assistant students | 30 | Psychoeducation Direct contact | Short (one day) | Not reported |
| 2008 | Ciência, Cuidado e Saúde | Brazil | capacitação e a gestão de equipes do PSf para a atenção psicossocial: um estudo de caso | Qualitative | Case Study | Professionals and Mental health technicians | 66 | Education (training) | Medium-term (3 months) | No follow-up |
For the analysis of quantitative research, the Cochrane review methodology was employed for the experimental and quasi-experimental studies using the risk of bias tool 2.0 (RoBtool 2.0) 34 and the Risk of Bias in Non-Randomized Studies of Interventions (Robins-I) tools 35. The assessment categories for both the tools corresponded to "low risk," which refers to high-quality studies comparable to a controlled clinical trial; "moderate risk," which refers to studies that offer solid evidence, but are not comparable to a controlled clinical trial; "serious risk," which refers to studies that have some methodological problems; and "critical risk," which refers to studies that have several problems and their results are not useful 34,35. These tools also provided an overall evaluation of the quality of the study and demonstrated that studies with a critical risk of bias should be excluded from a meta-analysis, warning about the limitations of studies with a serious risk of bias 35.
The parameters used in the evaluation of quasi-experimental studies were divided into three domains 35), as given below:
Pre-intervention:
Confounding variable: this refers to the effect of a variable on the intervention that needs to be examined with stratified or regression analysis.
Selection of participants based on the inclusion and exclusion criteria.
Intervention:
Classification of interventions based on the definition of the program or strategy used.
Post-intervention:
Deviations in the treatment, which is related to changes produced in the participants as a result of contamination between the groups.
Incomplete data, which corresponds to the effect of data lost in the results after analyses.
Measurement of the outcome, which refers to the use of reliable tools to evaluate the effectiveness of the intervention.
Selection of the outcome, which is determined from the estimation of the effect of the intervention.
In the case of experimental studies, the criteria for confounding and selection of participants were not used because the randomization process minimizes the risk of bias 34. For this review, quantitative studies that met the quality criteria were characterized as having a description of a central hypothesis based on the effect of the intervention to reduce stigma, describing the intervention, presenting conclusions about the effect of the intervention, or being able to determine the effect from the data presented. In order to evaluate the quality of qualitative studies, the caspe methodology was used and the following criteria were considered 36: The presence of a clearly defined topic such as interventions to reduce stigma in any of its manifestations; relevance of the method used to answer the question of interest, description of the relationship with the objective of the research; and the usefulness of the results in a Ibero-America framework, considering the reproducibility of the study in different social and cultural contexts 37.
Results
The systematic search for information across the six databases yielded a total of 750 publications, of which 230 repeated studies were excluded. We eliminated 215 studies that were conducted in countries other than Ibero-America, thereby 305 studies met the eligibility conditions. We discarded 287 studies that did not involve interventions and mainly corresponded to studies related to stigma in infectious diseases such as HIV, Hansen's Disease, or tuberculosis (n = 196), studies on scale validation and cultural adaptation (n = 24), pharmacological treatments (n = 18), and meta-analyses or systematic reviews (n = 49). Finally, a total of 18 studies were selected that met the inclusion criteria, including 10 from Spain 38-47, 2 from Portugal 48,49, 2 from Brazil 50,51, three from Chile 52-54, and one multicenter study coordinated from Colombia 55.
The types of studies that predominated were quantitative ones (n = 13), of which nine corresponded to quasi-experimental studies 38-40,44,48-51,54, and four to experimental studies 41,43,47,53. Out of the four studies with a qualitative approach, three corresponded to case studies using a group approach 56: The first one involved information strategies through the use of social networks 55, the second and the third used a direct contact strategy between the students and the mental health service users 45,46, and the fourth included the development of a training program for professionals 51. Finally, one study analyzed the reliability and safety conditions of an intervention to be used later in an experimental setup 52.
Out of all the studies reviewed, five fully complied with the quality characteristics that indicated a low probability of bias in the research 40,43,47,53,54. On the other hand, the principal source of bias in the quasi-experimental studies corresponded to the predominance of convenience samples, and the exclusion of randomization for the assignment of the control group when included. Previous studies have shown that gender can be a confounding variable for the results of interventions because women demonstrate a greater reduction in stigma 23. Accordingly, seven studies out of those reviewed considered this variable in their analyses 38-43,49. Table 2 summarizes the criteria for evaluating the quality of the studies.
Table 2 Quality analyses of the quantitative studies (Robins-I and ROBtool 2.0)
| Study | Pre-intervention | Intervention | Post-intervention | ||||
|---|---|---|---|---|---|---|---|
| Bias due to con- founding* | Bias in selection of participants into the study* | Bias in classification of interventions* | Bias due to deviations from intended interventions* | Bias due to missing data* | Bias in measurement of outcomes* | Bias in selection of the reported result* | |
| Stigma-Stop: A Serious Game against the Stigma toward Mental Health in Educational Settings | Moderate | Low | Ni | Low | Moderate | ||
| Effectiveness of the “What’s Up!” Intervention to Reduce Stigma and Psychometric Properties of the Youth Program Questionnaire (YPQ): Results from a Cluster Non-randomized Controlled Trial Conducted in Catalan High Schools | Low | Low | Low | Low | Low | Low | Moderate |
| Fight against Stigma Program: results obtained in the training of mental health professionals | Moderate | Critical | Ni | Ni | Ni | Serious | Ni |
| Effectiveness of an intervention of the community social support team in the psychosocial functioning of people with SMD | Low | Moderate | Low | Low | Low | Low | Low |
| Effectiveness of an intervention to reduce social stigma toward mental illness in adolescents (Cluster test)* | Low | Low | Low | Low | Low | ||
| Impact of the OBERTAMENT mass media campaign on the levels of stigma among the population of Catalonia, Spain. | Low | Low | Low | Low | Low | Low | Low |
| Modification of stigma associated with mental illness: evaluation of an intervention in compulsory secondary educational institutes in Navarra (doctorate thesis)* | Low | Low | Low | Low | Low | ||
| PsychoED: An online and community alternative for psychoeducation in schizophrenia | Moderate | Moderate | Low | Low | Moderate | Low | Low |
| Intervention for reducing stigma: Assessing the influence of gender and knowledge | Low | Moderate | Low | Moderate | Low | Low | Low |
| Mental health awareness action in schools | Ni | Ni | Ni | Ni | Ni | Serious | Ni |
| Mental Health program on stigma: Effects of direct and indirect strategies on stigmatizing attitudes | Low | Low | Moderate | Low | Serious | Serious | Serious |
| Effects of a psychoeducational intervention program on the attitudes and health perceptions of relatives of patients with schizophrenia* | Low | Low | Low | Low | Low | ||
| Effectiveness of a psychoeducational intervention for reducing burden in Latin American families of patients with schizophrenia | Low | Low | Low | Low | Low | Low | Low |
* Criteria used for randomized clinical trials, does not include the pre-intervention phase.
NI: No Information.
Regarding the qualitative publications, the studies clearly identified interventions to reduce stigma as the central theme with specific groups such as mental health service users 52,55, undergraduate students 45,46, and mental health professionals 51. All these studies determined the coherence between the method and the proposed objective by adopting an exploratory or descriptive approach. In addition, concerning the reproducibility criteria, these studies were feasible and relevant in the socio-cultural context to be repeated in Ibero-America. Table 3 summarizes the quality characteristics of these studies.
Table 3 Quality analyses for the qualitative studies (caspe)
| Defined topic | Relevance of the Method | Versatility of the results (reproducibility in Ibero-America) | |
|---|---|---|---|
| “Inclúyete”: socioeducational and inclusive program for people with severe mental disorders and students at the University of Almería | The authors raise the barrier effect that stigma produces in people with severe mental disorders. This affects the exercise of rights, the enjoyment of community services and the establishment of meaningful social relationships. They consider it necessary that people with a clinical diagnosis of SMD can participate in the designed interventions so that they can relate their experience in the first person, in a close way, transmitting their feelings and concerns in a realistic way. | The study is descriptive and indicates various experiences of general training in various areas where users with a SMD diagnosis participate together with the student and general population. | The experience is replicable; it is aimed at direct contact through which awareness of mental health is favored. The socioeducational activities strategy is simple and easy to implement in higher education environments. |
| Development of an intervention to reduce self-stigma in outpatient mental health service users in Chile | The authors found that self-stigma leads to social exclusion and had a negative impact on the quality of life for people with SMD. They also concluded that in Latin America there is too little information related to anti-stigma interventions, which is why it is not possible to reach conclusions about the effectiveness of these interventions. | The study identified conditions for safety and feasibility of an intervention based on psychoeducation and recovery. From the qualitative analyses, the participants highlighted an increase in self-confidence and the use of anti-stigma strategies in their daily life. | The intervention corresponded to a pilot study. The authors emphasized the characteristics of reproducibility for other Latin American countries since the interventions can be developed from the activities established in mental healthcare programs. |
| “Accepting demented minds.” Opinion Group, information and support group on stigma of mental illnesses on Facebook | The authors identified the consequences of stigma and prejudice in people with mental disorders, their families, and professionals who provide mental health services. The study examined the practicality of using social networks to disseminate information, facilitate social interaction and discussion of experiences, and also to find support. | The study is of an exploratory nature and offers information about the characteristics of using social networks, the profile of the users associated to the intervention, and the topics of greatest interest. | The study is reproducible to the extent that it uses a mechanism to provide information based on a widely accepted worldwide network. The intervention is cost-effective, safe, and encourages the participation of diverse populations. |
| A visit against stigma and pro prevention in a treatment unit for serious mental illness | The authors found that prejudices and negative attitudes are frequent in nursing assistant students. Therefore, direct contact and psychoeducation were strategies that reduced stigma toward people with serious mental disorders. | The study was based on group experiences and analyzed the views of nursing assistant students and mental health service users. The study was able to identify the representations of stigma and their relationship with empowerment and psychosocial rehabilitation. | This strategy to reduce stigma is low cost, which is advantageous when combined with professional practices. |
| A capacitação e a gestão de equipes do PSf para aatenção psicossocial: um estudo de caso | The authors propose the need to do a critique of the predominant use of the biomedical model in mental health care. They emphasized that the attitudes of professionals cause an impact in the attention they provide in psychosocial programs. | The study is of an exploratory nature and is based on assumptions of historical dialectical materialism. It identifies the influence of external factors in the implementation of psychosocial care programs. | The study can be replicated in Ibero-America countries taking into account the tendency of reforms in mental health care. Criticism concerning the biomedical model become the foundation for the transformation of attitudes, promote intercommunication with the members of the community, and implement co-responsibility in the interventions. |
The target population of the interventions corresponded mainly to high school students (n = 7), followed by family members and caregivers (n = 3), users of mental health services (n = 3), professionals (n = 2), general population (n = 1), mixed population-undergraduate students and general population (n = 1), and nursing assistant students (n = 1). The samples sizes were variable, for example, one of the experimental studies involved a total of 41 relatives 53, whereas the other two were conducted on a larger population of students (280 and 185 subjects) 41,43. Regarding the quasi-experimental studies, the sample size was <100 subjects in five of the studies 42,44,48,50,54; while the remaining four studies had a sample size of 265-1019 38-40,49. The majority of the interventions of the reviewed studies were based on psychoeducation (n = 7) 39,44,47,48,52-54, education (n = 4) 41,50,51,55, both education and contact (n = 5) 38,42,43,46,49, both psychoeducation and contact (n = 1) 45, and one was based on a massive campaign (n = 1) 40. All of the studies reported the duration of the intervention. Some were classified as short-term, which according to Yamaguchi are those that were conducted in a period of <1 month 23; 7 of the studies fit this description 41-43,45,48-50. Other interventions were medium- and long-term, which according to Mehta are those conducted between 1 and 6 months and >6 months, respectively 57; 8 studies were medium-term 38,40,46,47,51-54, and three were long-term 39,44,55. A total of 11 studies were performed pre- and post-tests to determine the effect of the interventions 38,39,41-44,47,49,50,52,53, and only 33.3% of the studies reviewed reported some type of follow-up after the intervention 38,40,41,43,54,55.
The studies done with high school students demonstrated effectiveness and showed statistically significant differences between pre- and post-interventions. However, the effect size was small, and differences were noted according to the gender. The studies by Andrés-Rodríguez et al. and Martínez-Zambrano et al. concluded that, in women, stigma decreased more toward people with SMD, and these results were related particularly to stigma subdomains such as authoritarianism and socially restrictive attitudes 38,42. Furthermore, de Simón-Alonso reported that women had more fear and less tendency to blame people with SMD 43. Finally, the study performed by Cangas et al. reported that, in the experimental group, the preconceived idea of people with SMD being dangerous was low 47.
Studies that involved family members and caregivers included measures of effect related to stigma by association. In this case, the feelings of shame and anger on the loss of social status due to the disorder were important reasons for the interventions. A study conducted by Gutiérrez-Maldonado et al. identified changes in affective attitudes (p = 0.006), cognition (p = 0.001), and behavior (p = 0.005), indicating that caregivers learned how to act, express their feelings, and think in a positive and flexible manner regarding the disorder 53,54. Soto-Pérez, on the other hand, studied the effect of an online intervention on the level of knowledge about schizophrenia in relatives of people with this diagnosis in Spain 44. Their results indicated that caregivers increased their knowledge about the causes of the disorder (p = 0.013), the treatments (p = 0.032), the family roles (p = 0.014), and the prodromes (p = 0.009). Furthermore, Cárdenas-Mancera et al. conducted an intervention using a social network site with a follow-up on the participation of mental health service users and family members on an online platform, but did not detect any direct measure of effect 55. They concluded that association to a network helps educate the population about diagnosis, treatment options, and psychosocial support mechanisms aimed at people with SMD. However, the abovementioned two studies did not include information about how education affects the negative self-perception of the caregiver.
The majority of the studies that involved professionals and nursing assistant students were characterized by the use of qualitative methods; therefore, the effectiveness was evaluated from the perception of their experiences. For example, Oliveira et al. concluded that work training is a factor that favors the comprehensiveness of care and helps professionals promote autonomy of people with mental disorders. Their results indicated that, after a training process, attitudinal changes occurred in professionals that improved communication with mental health service users and their families 51. In addition, a study on awareness and direct contact performed in psychosocial rehabilitation programs in Spain identified attitudinal changes toward people with serious mental disorders in a group of nursing assistant students 45. The results demonstrated that the establishment of interaction strategies could modify attitudes and prejudices such as rejection and beliefs about danger and encouraged tolerance, expression of feelings, and recognition of individual capacities of people with SMD. Barrantes et al., on the other hand, developed a quasi-experimental study in Portugal that involved a training program aimed at reducing preconceptions toward people with mental disorders, and they evaluated stigma as a dependent variable in the following nine domains: responsibility, grief, irritation, danger, fear, help, coercion, segregation, and avoidance 48. Their results demonstrated differences only in the avoidance domain, which revealed significant changes between the average baseline values and the average value obtained after the intervention (17.17 ± 5.42 vs 13.52 ± 5.37; t = 2.791; gl = 71; p = 0.007). However, they suggested that strategies to reduce stigma should be implemented in several areas such as educational institutions, workplaces, social health institutions, and even the media.
A study conducted in Spain by Ballesteros and Bertina evaluated a community intervention that involved multidisciplinary activities, intervention at home, and social support 39. The interest of the research group was focused on the impact of social and occupational functioning with the perception of stigma being a secondary variable that was determined from the decrease in feelings of low self-esteem and the deterioration of self-concept. They reported moderate effect sizes for the evaluated areas using the World Health Organization Disability Assessment Schedule (WHODAS II), which incorporates questions concerning perception of other people's attitudes toward people with SMD in the domain of society participation. The study reported that mental health service users perceived a decrease in negative attitudes toward themselves after the intervention (the effect size was 0.31). Furthermore, these results remained constant after 3 years of association with the program, with a reported effect size of 0.32.
In Chile, Schilling et al. developed an intervention to reduce the impact of self-stigma on the users of outpatient healthcare centers 52. Preliminary results indicated that these users increased their self-confidence and used the strategies to reduce stigma. In addition, their data highlighted the importance of family participation, friends, the support of professionals, along with the search for help to reduce self-stigma. Moreover, the users valued intervention strategies that incorporated psychoeducation and a narrative approach. An intervention using social networks conducted by Cárdenas-Mancera et al. included users of mental health services from nine Ibero-America countries. Their results revealed that the formation of an opinion group promoted the development of discussion sessions that debated problems associated with mental disorders, including stigma. The study also reported that the topic that received the greatest number of interventions was stigma, which was acknowledged through 15 shared publications that talked about mental disorders, and that, on a monthly average, received comments or socialization of articles from at least two mental health service users 55.
Rubio-Varela et al. analyzed the impact of the OBERTAMENT campaign in Catalonia (Spain), a study aimed at the general population using mass media such as television and internet. The results of the study indicated that 11% of the population spontaneously recalled the campaign, but only 0.8% remembered that it was related to stigma and discrimination toward people with mental health problems. Accordingly, the reported effect sizes were medium and low. For example, the effect size was low for the benevolence subscale, whereas medium effect sizes corresponded to maintaining a relationship with a friend who develops a mental disorder (d = 0.39) and living with someone with a mental disorder (d = 0.27) 40.
Discussion
This is one of the first reviews to systematically compile data on interventions to reduce stigma in Ibero-America. The main objectives of this review were to describe the characteristics and main results of interventions using quality assessment and a risk of bias profile for each study. We analyzed 18 studies conducted in Ibero-America aimed at reducing stigma toward serious mental disorder. Quantitative studies using mainly a quasi-experimental design (n = 9) predominated over qualitative studies (72.2% vs 27.8%). In the case of qualitative studies, three corresponded to group case studies, one study offered information on the feasibility and safety conditions of a pilot intervention of an experimental study, and another one described the development of a program to promote social inclusion of people with SMD to avoid attitudinal barriers. It is therefore important to highlight the notorious lack of studies related to interventions to reduce stigma toward serious mental disorders in Ibero-America. Furthermore, an important gap was noted in the research conducted between high-income countries, mainly in English-speaking and Ibero-America countries 17,23.
Regarding the first objective and in relation to the level of quality determined by applying the Robins-I and ROBtools 2.0 tools, we noted that a quarter of the quantitative studies failed to satisfy the quality criteria. The main weaknesses recorded corresponded to the absence of information for the overall quality level of the studies, and, in studies that included this information, the quality levels showed a probability of serious or critical risk of bias, which would exclude them from any review process 34,35. However, due to the lack of research on the subject, we included all the studies in the present review to assess the quality so as to establish a baseline that will guide future researches 34,35. Notably, all studies with serious or critical risk of bias were conducted using a quasi-experimental design. The implementation of these studies has been widely developed in the field of social sciences because of their relevance; however, they have increased in the area of health due to their possible application in real life, unlike in experimental studies. The interest in using this type of research to summarize scientific data has increased because the external validity has improved with due consideration to the influence of variables that are difficult to isolate, such as the culture and motivation 58. Although the use of a quasi-experimental design may offer advantages in terms of implementation of the interventions, the results have limitations, especially when determining significant findings that lead to establishing possible causal relationships 58. Insufficient information on the quality of interventions to reduce stigma in Ibero-America reveals the need to develop new research that complements the data obtained until date; thus, being able to guide the decision-making step for public policy 59.
As for bias in the studies, the most frequent bias recorded was during the selection of participants. For example, the source of the sample was not reported in detail in one-third of the quasi-experimental studies 39,42,44. However, previous studies indicated that this type of a bias is common, necessitating the consideration of planning an intervention based on this design 60. It should be mentioned that there was a heterogeneity of interventions in terms of content and strategies and their applications, duration, and evaluation of the results and follow-ups; these last two aspects were related to the presence of bias post-intervention. Moreover, in two-thirds of the reviewed studies, serious biases were noted in the outcome measurements because of insufficient information to estimate the effectiveness of the intervention 48-50. A recurrent problem was noted since it was indicated in a previous review 23. There were only two quasi-experimental studies that reported sufficient information to classify them as low risk of bias for the three dimensions of pre-intervention, intervention, and post-intervention 40,54.
More importantly, the studies focused on relevant populations, for example, students, family or informal caregivers, the general population, mental health service users, and professionals, which is in agreement with the majority of researches that focuses on high school and university students followed by mental health service users, family members, and professionals 17,61,62. Unlike researches conducted in other countries, the low number of studies conducted in Ibero-America with the general population remains notable 17. The reason for this is most likely related to the fact that mass campaigns are expensive and require institutional support. Unfortunately, these conditions are not always present in Latin American countries since the resources allocated to mental health are usually low 63.
Concerning the samples in the studies we reviewed, they were mainly for convenience, and the largest sizes were in studies with students, similar to that in other countries 8,41,43,57. Meanwhile, the sample sizes for intervention with mental health service users and family members were reduced, perhaps due to the restrictions related to ethical criteria, access to health services, and/or motivation of the participants 8,10. Therefore, these results demonstrate the need to concentrate efforts on the design of protocols with larger and more representative samples 34,35. Hence, it is important to carefully consider the ethical guidelines established in each country when developing the recruitment process 64.
In the present review, we identified seven short-term, eight medium-term, and three long-term interventions; however, the duration of the intervention was not related to its effectiveness. These results coincide with those presented in a review by Yamaguchi et al. that demonstrated that interventions with different durations can have similar effects 23. On the other hand, Mehta et al. indicated that the data on the effectiveness of interventions is precarious since the results are only favorable for short-term durations, which necessitates follow-up studies to establish the effectiveness of long-term interventions 57.
Concerning the second objective, the heterogeneity of the implementations for the interventions makes it difficult to evaluate their impact. In the present review, the majority of the interventions that used a combination of education and contact strategies were effective, albeit with a low effect size 17,61. Out of the different intervention techniques applied, direct and indirect social contact demonstrated better results when compared with interventions such as education 23,65. Hence, interaction with people with a mental disorder has been documented as a strategy that produces changes in attitudes and social distance 61. However, Gronholm et al., Yanos et al., and Gerlinger et al. indicated that this type of strategy could increase its effect when combined with some type of an education approach 61,62,66. Indeed, the use of strategies involving multiple mechanisms of social contact have been suggested for results, such as recovery 67.
Here, we identified medium (d = 0.42) and high (d = 0.82 and 0.85) effect sizes in three studies that implemented the psychoeducational strategies. However, these studies were characterized by having small sample sizes 44,53,54. Thus, Mehta et al. concluded that the effect size varies between a medium effect for an increase in knowledge (d = 0.54) and a low effect for a decrease in stigmatizing attitudes (d = 0.22) 57. In case of studies included in the present review, the results were not sufficiently detailed to determine the extent of the effect of the interventions. In some cases, there was insufficient data presented, which made it difficult to reach a conclusion in favor of any specific strategy. Nevertheless, it is important to acknowledge that efforts are being made in Ibero-America to reduce stigma toward people with SMD. However, there are only substantial differences related to the development and impact of interventions between Spain, Portugal, and Latin America, which seems to be related to the health aspects of these countries. In Ibero-America, a process of psychiatric reform was performed, which included the concern and fight against stigma in different manners. In Spain, for example, there are campaigns aimed at the general population that are constantly working to raise awareness about stigma and ways to reduce it 18,40. Similarly, of the studies reviewed, quantitative studies predominated, in which 2 randomized controlled trials stood out along with a quasi-experimental study with a low probability of bias 40,41,43. Portugal has very similar characteristics to Spain in terms of the psychiatric reform processes, but there was less evidence found on issues related to stigma reduction in mental health in the former 31. In Latin America, the process is disparate; however, it is important to highlight the advances that are being made to reduce stigma in some countries in the area. In the case of Chile, for example, the approach to this topic was defined as a priority in the Mental Health Strategic Plan. It was declared that "by the year 2020, at least 50% of the healthcare services must implement a plan of dissemination and support for the exercise of rights and anti-stigma" 68. This plan involves the incorporation of a transversal anti-stigma vision as a public policy guideline in mental health that responds to the needs of the population with SMD and their families, similar to that in Argentina, Brazil, and Colombia 24,69-71. However, it is necessary to reinforce these advances to reduce the current gap in the medical care and treatment of people with SMD. Accordingly, one of the most relevant ways is to collect reliable information in order to evaluate, compare, and replicate successful experiences that are well adapted to the cultural and social conditions of each country and which improves the quality of life for users of mental health services and their families 8,14,52.
This review is a first step toward the systematization and quality assessment of research in stigma reduction in Ibero-America. Our analyses facilitate the recognition of those aspects that should be incorporated in the future studies in order to reduce possible biases. In addition, the information presented here is expected to be useful toward establishing a baseline to help determine the influence of contextual factors in the occurrence of stigma in diverse populations. Furthermore, an aspect to consider for both future reviews and programs toward reducing stigma corresponds to the need for the development of operational definitions for the duration of the intervention. In the present review, we identified a predominance of medium-term interventions (44%). However, for new protocols, it is crucial to implement mechanisms that identify the differences between the duration time and the follow-up time, with these elements being assumed as independent parameters that would expedite the organization of activities, final results, and effectiveness of the intervention 17,57.
The present review reveals limitations that prompt caution when it comes to interpreting the results while highlighting insufficient information regarding interventions to reduce stigma in Ibero-America and the heterogeneity of the populations at which they are directed as well as the strategies and mechanisms employed. Unfortunately, this lack of information complicates the development of methodological approaches to measure the global effect.