Introduction
Approximately, 1.9 billion adults are currently overweight (body mass index (BMI) 25 to 29.9 kg/m2) and a further 650 million are obese (BMI >30 kg/m2) (Mahadevan & Ali, 2016; West, Caterini, Banks, & Wells, 2018; World Health Organization, 2018). Ranking second only to smoking as a preventable cause of death, obesity (OB) contributes to over 300.000 deaths per year (Abdelaal, le Roux, & Docherty, 2017; Allison, Fontaine, Manson, Stevens, & VanItallie, 1999). OB is also associated with a wide range of medical and psychological sequelae, eating disorder behaviors such as binge eating and subsequent impaired health-related quality of life (HRQoL) (Pagoto, 2011; Reichborn-Kjennerud, Bulik, Sullivan, Tambs, & Harris, 2004; Vetter et al., 2011).
It is well known that OB and certain medical comorbidities are associated with adverse neurocognitive outcome (Cook et al., 2017; Hou et al., 2019). Neuropsychological investigations of patients with medical diagnoses including hypertension, diabetes, and obstructive sleep apnea have demonstrated deficits across a variety of cognitive domains, including attention, processing speed, memory, and executive functioning (EF) (Manschot et al., 2006; Ostrosky-Solís, Mendoza, & Ardila, 2001; Salorio, White, Piccirillo, Duntley, & Uhles, 2002). Within the domain of the relationship between cognitive abilities and weight problems, particular attention has been paid to impairments in EF (Cabas, González, & Mendoza, 2018; Groppe & Elsner, 2017).
EF is believed to reflect effortful cognitive control that serves to manage multiple basic cognitive processes in order to achieve goal-directed behaviors (Alvarez & Emory, 2006; Etnier & Chang, 2009). It also refers to a broad range of self-regulatory processes that enable the control of thoughts, actions, and emotions (Nelson & Luciana, 2008) through set shifting, working memory (WM) updating, and inhibition (Miyake et al., 2000). Findings appear to partly depend on the particular tasks used. However, there is a consensus on the association between OB and impaired task performance on various measures of EF in adolescents and adults. Furthermore, current literature lacks a systematic review about the relationship between ED and OB.
For instance, a meta-analysis and review identified 72 studies—with 4904 overweight/obese participants (Yang, Shields, Guo, & Liu, 2018). It was found that obese participants showed broad impairments on EF, including inhibition, cognitive flexibility, WM, decisionmaking, verbal fluency, and planning. Overweight participants only showed significant deficits in inhibition and WM.
Another review was aimed at systematically investigating the evidence suggesting that obese individuals demonstrated impaired performance on behavioral tasks examining EF abilities (Fitzpatrick, Gilbert, & Serpell, 2013). Twenty-one empirical papers were identified, and the results were considered in relation to different EF domains. This review suggests that obese individuals show difficulties with decision-making, planning and problem-solving when compared to healthy weight controls, with fewer difficulties reported on tasks examining verbal fluency and learning and memory.
Method
A three-step methodological approach was used to acquire a deeper understanding of the relationship between executive dysfunction and obesity. Firstly, a bibliometric analysis shows the evolution, main journals, and researchers of the topic. Secondly, the Tree of Science (ToS) is used to show a chronological review that provides a general description of the roots and current perspectives of the state of literature. Finally, clustering analysis of the co-citation network was employed to identify the different perspectives of the topic and a datamining with the titles in order to confirm the subtopics. Finally, the three main processes are explained in the subsequent paragraphs.
Step 1: Bibliometric Analysis
A bibliometric analysis was made to identify the importance of the research topic: executive dysfunction and obesity in the current literature (Zupic & Čater, 2015). Sinab database from Universidad Nacional de Colombia has been used to track studies about the relationship between ED and OB. Then, the indexed Web of Science database was selected to identify articles that describe keywords as ED and OB. That’s why the search equation (SE) used is TOPIC:(executive dysfunction) AND TOPIC: (obesity) from January 2001 to January 2019. This is a similar approach used by other researchers (Vallaster, Kraus, Merigó, & Nielsen, 2019). The search yield a total of 222 results that matched the criteria above and no paper was removed manually to improve the accuracy of the outcomes analyzed using graph theory.
Step 2: Chronological Literature Review
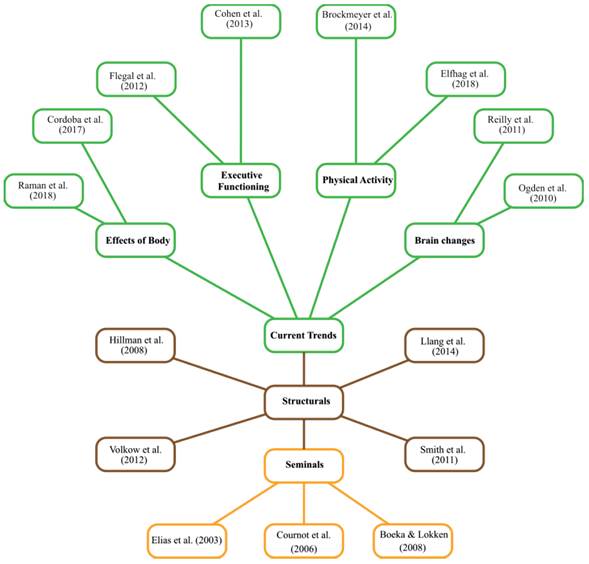
Articles that fulfilled the requirement above were then loaded in the website Tree of science (TOS) (Figure 2) (Robledo, Osorio, & López, 2014). ToS allows to build and understand the theoretical framework from the initial search in Web of Science. This algorithm is based on the graph theory where studies are represented as nodes and citations as links. So, every node is a knowledge unit in the network. The most important nodes are detected by their location, this is determined by the links that connect other nodes (Hirsch, 2005). In that sense, articles located in the roots are seminal references about ED and OB. Studies from the trunk are structural articles. Finally, the leaves are articles that represent current theories.
Step 3: Co-citation Analysis
The bibliometrix package in R-Cran was used to convert the txt file from Web of Science to a two column excel file and create the co-citation network (Aria & Cuccurullo, 2017). At the end of this process, an algorithm to find the main clusters was executed (Blondel, Guillaume, Lambiotte, & Lefebvre, 2008). In order to confirm the topics of the perspectives, we conducted a data mining analysis with wordcloud r package (Fellows, 2012) using the words from the titles of the papers. Finally, the main papers were selected according to the indegree, out degree, and betweenness metrics as it is explained in another study (Zuluaga et al., 2017).
Results
Rationale of Research in Obesity: A BibliometricAnalysis
Research databases show an evolution of the number of papers per year available in WoS on obesity and executive dysfunction research topics. The first publica tion, according to WoS data was in 2006. From this moment on, the number of papers has grown on an annual percentage rate of 25.31%.
Table 1 provides an overview of the most important journals according to their number of papers in the search. This table presents the journal of appetite as the most influential in this topic with 12 articles that were cited 362 times, and the journal is in a Q1 quantile. The rest of the journals are in quantile Q1 showing the quality of the research topic. Additionally, their IF is greater than 1and the Journal obesity has more important papers according to the number of citations received (>50). This rationale confirms the importance of the area.
Table 1 The most Important Journals of Obesity According to the Number of Published Papers
| Journals | Papers | Quantile | IF | TC | >50 |
|---|---|---|---|---|---|
| Appetite | 12 | Q1 | 1.44 | 362 | 2 |
| Obesity | 9 | Q1 | 2.06 | 209 | 3 |
| Plos One | 5 | Q1 | 1.16 | 209 | 1 |
| Journal of the International Neuropsychological Society | 4 | Q1 | 1.41 | 32 | 0 |
| Others | 47 | - | - | - | - |
Note. IF Impact Factor of 2017 taken from scimago; TC: Times Cited; >50: Number of papers with >50 citations. Based on Web of Science database.
Table 2. presents the most influential researchers of executive dysfunctional and obesity. According to the results, professor John Gunstad is the researcher with more papers and with an h-index of 34. Also, with the most important production according to TC and the number of papers cited more than 25 times. Although doctor Crosby has the best h-index (91), his research is focused on statistics and eating disorders. This metric provides that executive dysfunctional and obesity is not only a popular topic but also the researchers behind it are important.
Table 2 The most Productive Researchers in ES
| Researchers | Papers | H. Index | TC | >50 |
|---|---|---|---|---|
| John Gunstad | 22 | 34* | 650 | 7 |
| Mary Beth Spitznagel | 14 | 36** | 524 | 5 |
| Ross D. Crosby | 10 | 91** | 85 | 2 |
| James E. Mitchell | 10 | 58* | 120 | 3 |
* h-index was taken from Web of Science
** h-index was taken from Google Citation
Note. TC: Times Cited; >50: Number of papers with >50 citations. Based on Web of Science database
Chronological Evolution: A Tree of Science Perspective
Seminal works are articles that initially presented an idea of great importance or influence within a particular discipline. A group of articles that introduce the relationship between ED and OB will be presented (Figure 1).
One study examined neuropsychological performance in a clinical sample of obese patients (Boeka & Lokken, 2008). Individuals seeking surgical treatment of OB (N = 68) were administered cognitive tests as part of a standard pre-surgical evaluation. Results indicated significant differences in performances of obese individuals on tests of EF (planning, problem solving, mental flexibility) in comparison to normative data. No significant differences emerged between obese patients with and without co-morbid medical conditions of hypertension, type II diabetes, and obstructive sleep apnea on the neuropsychological tasks specific to EF. Taken together, these results provide further evidence of specific cognitive dysfunction in obese individuals.
The purpose of another work was to examine the combined effects of OB and hypertension on cognitive functioning among community-dwelling older adults who had not experienced clinical stroke, dementia, or cardiovascular disease (CVD) (M. F. Elias, P. K. Elias, Sullivan, Wolf, & D’Agostino, 2003). OB and hypertension are well-established risk factors for CVD in the general population. There were four important findings in this study: (1) significant effects of hypertension and OB on tests of learning and memory were observed for men, but not for women; (2) OB and hypertension were associated with lower cognitive functioning in late middle-aged and elderly men, independent of other common CVD risk factors; (3) OB and hypertension had common effects on specific tests of memory, thus suggesting that pathophysiological mechanisms by which they affect cognition may be similar; (4) among men, the adverse effects of OB and hypertension are cumulative with respect to deficit; the presence of both risk factors results in more cognitive deficit than the presence of either or none.
Finally, a research hypothesized that mid-life OB may modulate the impact of conventional cardiovascular risk factors (CVRF) on cognitive impairment (Wolf et al., 2007). They tested this hypothesis in the community-based Framingham Offspring Study sample. Midlife measures of central OB (Waist-hip ratio (WHR) in the uppermost quartile Q4) and of hypertension (Blood Pleasure 140/90 or use of anti-hypertensive medication) were each significantly related to poorer performance on EF & visuomotor skills (Trails B, Visual Reproductions-Immediate and Delayed Recall). Further, the relation of hypertension to neurocognitive performance was significantly modified by WHR; hypertension was not associated with neurocognitive performance in WHR Q1-Q3 but was associated with a marked adverse performance in Q4 WHR. Neither hypertension nor OB was individually or synergistically related to verbal memory (immediate or delayed recall).
When it comes to articles from the trunk of the tree, it is all about shaping the theory on the relationship between ED and OB. One of the studies examined the relationship between OB, EF, disinhibition, and brain volumes in relatively healthy youth (Maayan, Hoogendoorn, Sweat, & Convit, 2011). Participants included 54 obese and 37 lean adolescents. Participants received a cognitive battery, questionnaires of eating behaviors, and magnetic resonance imaging (MRI). Neuropsychological assessments included tasks targeting frontal lobe function. Eating behaviors were determined using the Three Factor Eating Questionnaire (TFEQ), and structural MRIs were performed on a 1.5 T Siemens Avanto MRI System (Siemens, Erlangen, Germany) to determine brain gray matter volumes.
Relative to lean adolescents, obese participants had significantly higher ratings of disinhibition on the TFEQ, lower performance on the cognitive tests, and lower orbitofrontal cortex (OFC) volume. Disinhibition significantly correlated with BMI, Stroop color-word score, and OFC volume. However, this is a cross-sectional view that does not allow to comment on clear causality.
Previously, another article had been published, it examined the association between BMI, regional volume differences in gray and white matter measured by MRI, and cognitive functioning in older females (Walther, Birdsill, Glisky, & Ryan, 2010). Participants included 95 community-dwelling older females (ages 52-92 years) who underwent extensive neuropsychological testing and high-resolution MRI scanning. Higher BMI was associated with decreased gray matter volumes in the left orbito-frontal, right inferior frontal, and right precentral gyri, a right posterior region including the parahippocampal, fusiform, and lingual gyri, and right cerebellar regions, as well as increased volumes of white matter in the frontal, temporal, and parietal lobes, even when hypertension was considered. Compared to normal weight women, obese women performed lower on tests of EF. Smaller gray matter volume in the left orbitofrontal region was associated with lower EF. Additionally, despite the lack of significant group differences in memory and visuomotor speed, gray and white matter volumes predicted performance on these measures.
Similarly, a study also explored neuropsychological performance of adolescents with excess weight (n = 27, BMI range 24-51 kg/m2) vs. normal-weight adolescents (n = 34, BMI range 17-24 kg/m2). This EF battery included WM, reasoning, planning, response inhibition, flexibility, self-regulation, and decision-making tasks (Verdejo et al., 2010). They also aimed at exploring personality traits of impulsivity and sensitivity to reward. Results showed significant differences between groups on indexes of inhibition, flexibility, and decision-making (excess-weight participants performed poorer than controls), but not on tests of WM, planning, and reasoning, nor on personality measures. Moreover, regression models showed a significant association between BMI and flexibility performance. These results are indicative of selective alterations of particular components of EF in overweight adolescents
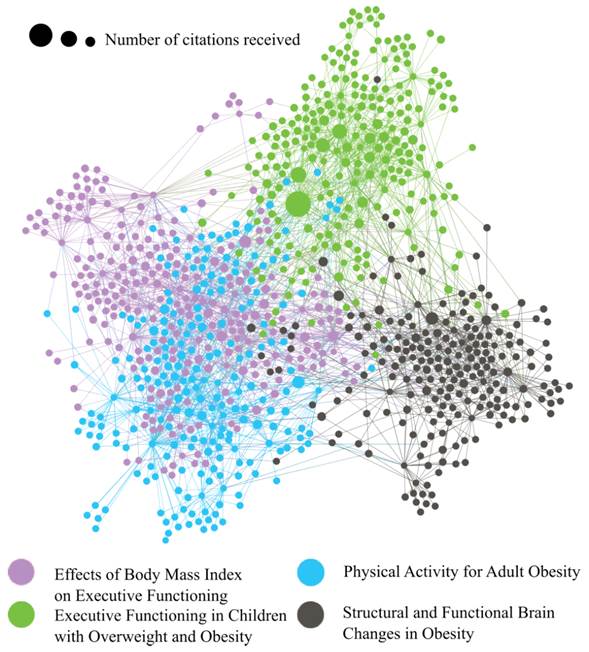
Finally, articles located in the leaves are new perspectives, they show higher density in the network due to the fact they are subthemes about the relationship between ED and OB. Results show four research lines: (1) effects of body mass index on executive functioning, (2) executive functioning in children with overweight and obesity, (3) physical activity for adult obesity and (4) structural and functional brain changes in obesity.
Perspectives of SE: A Co-citation Analysis
Figure 2 presents a co-citation network according to the search explained in the methodology section. Dots represent papers and the links among them the citations or references, and the software to create the visualization was Gephi (Bastian, Heymann, & Jacomy, 2009). The visualization suggests four clusters that represents 54.74% of the whole network and the remaining 7 clusters are below to 10%. The remaining part of this section proceeds with the construction of the four main perspectives.
Effects of Body Mass Index on Executive Functioning.
A research wanted to determine whether OB, estimated according to BMI, waist circumference, and body fat and abdominal fat assessed using dual-energy X-ray absorptiometry (DEXA), was associated with cognitive performance (Smith et al., 2014). BMI, waist circumference, body fat, and abdominal fat were assessed using DEXA. Cognitive performance was assessed using a comprehensive neuropsychological battery. When categorized using BMI, overweight individuals had higher global cognitive function and EF scores than normal weight individuals. This relationship did not differ according to sex. When categorized according to DEXA, there were no relationships between body fat and cognitive function in the whole group, but women in the middle 0.35 (0.15); P = .01) and highest tertiles (0.37 (1.5); P = .01) of DEXA body fat had better EF than those in the lowest tertile (0.90 (0.15)).
Men in the middle tertile of DEXA body fat had significantly better EF and memory than those in the lowest tertile. BMI had greater power to predict EF than DEXA body fat. No significant associations were found between cognition and estimates of abdominal adiposity.
A similar study investigated the relationship between adiposity and cognitive functioning in heart failure (HF) for each sex, despite observed sex differences in HF prognosis (Hawkins et al., 2014). This study tested the hypothesis that greater BMI would be associated with poorer cognitive functioning, especially in men, in sex-stratified analyses. A neuropsychology battery tested global cognitive function, memory, attention, and EF. Composites were created using averages of age-adjusted scaled scores. According to regression analysis, BMI did not predict memory (P= .69) or global cognitive functioning (P= .08). In women, greater BMI was not associated with any cognitive variable (all P> .09). Higher BMI was associated with lower attention (B = -0.18; P= .009) and EF (B= -0.13; P= .043) in male HF patients, especially those with severe OB. These patients may therefore have more difficulties with the HF treatment regimen and may have lower outcomes.
Recently, one more work used functional connectivity magnetic resonance imaging (fcMRI) to examine: (1) the relationship between BMI and functional brain connectivity; and (2) the mediating role of functional brain connectivity in the association between baseline BMI and change in cognitive function over a 12-month period (Hsu et al., 2015). It was conducted a 12-month, prospective study among 66 community-dwelling older adults, aged 70 to 80 years, who were categorized as: normal weight (BMI from 18.50 to 24.99); overweight (BMI from 25.00 to 29.99); and obese (BMI ≥ 30.00). At baseline and 12-months, three executive cognitive processes were measured: (1) response inhibition; (2) set shifting; and (3) WM. Obese individuals showed lower task-related functional connectivity during finger tapping in the default mode network (DMN) compared with their healthy weight counterparts (p < 0.01).
A similar work correlated two independent measures of body composition-i.e., BMI and body fat percent (BFP)-with structural and functional neuroimaging data obtained from a cohort of 32 neurologically healthy adults (Figley, Asem, Levenbaum, & Courtney, 2016). Whole-brain voxel-wise analyses indicated that higher BMI and BFP were associated with widespread decreases in gray matter volume, white matter volume, and white matter microstructure (including several regions, such as the striatum and OFC, which may influence value assessment, habit formation, and decisionmaking). Moreover, closer examination of resting state functional connectivity, white matter volume, and white matter microstructure throughout the DMN, executive control network (ECN), and salience network (SN) revealed that higher BMI and BFP were associated with increased SN functional connectivity and decreased white matter volumes throughout all three networks (i.e., the DMN, ECN, and SN).
Taken together, these findings: (1) offer a biologically plausible explanation for reduced cognitive performance, greater impulsivity, and altered reward processing among overweight individuals, and (2) suggest neurobiological mechanisms (i.e., altered functional and structural brain connectivity) that may affect overweight individuals’ ability to establish and maintain healthy lifestyle choices (Figley et al., 2016).
Executive Functioning in Children with Overweight and Obesity.
One of the most relevant studies in children examined whether children differ in their performance on a battery of EF tasks depending on their weight status (underweight, normal-weight, overweight), and investigated the longitudinal cross-lagged associations between EF and BMI (Groppe & Elsner, 2017). Hot EF (delay of gratification, affective decision-making), cool EF (attention shifting, inhibition, WM updating), and BMI were assessed in 1.657 German elementary-school children, at two time points, approximately one year apart. Overweight children exhibited a lower performance in attention shifting t1: p < .01, t2: p < .01, WM updating t1: p = .01, t2: p < .01, and affective decision-making abilities t1, p = .02 when compared to normal-weight children. Unexpectedly, they did not show any deficits in inhibition t1: p = .73, t2: p = .51 or delay of gratification t1: p = .32, t2: p = .90. EF levels of underweight children did not differ significantly from those of normal-weight children at both time points: attention shifting: t1: p = .14, t2: p = .09; WM updating: t1: p = .36, t2: p = .94; inhibition: t1: p = .32, t2: p = .12; delay of gratification: t1: p = .41, t2: p = .96; affective decision-making: t1: p = .18, t2: p = .85. Furthermore, poor attention shifting and enhanced affective decision-making predicted a slightly higher BMI one year later, and a higher BMI also predicted lower attention shifting and WM updating one year later. This latter association between BMI and subsequent EF scores, however, diminished when controlling for socioeconomic status.
One more work backs up these results, it aimed to investigate the differences in neuropsychological test performance of Turkish and adolescents with OB and healthy peers. (Bozhurt, 2017). This study included 147 children and adolescents ranging in age from 8 to 16 years. Participants were administered depression, anxiety inventories and a neurocognitive test battery (memory, psychomotor speed, processing speed, reaction time, complex attention, EF, cognitive flexibility). Findings suggest that the mean scores of cognitive domains of obese patients were found to be statistically significantly lower than those of the control participants (p< 0.001). The mean anxiety inventory scores of the participants with OB were found to be higher than the control participants (p<0.05).
Physical Activity for Adult Obesity.
Research has shown that obese individuals have cognitive deficiencies in EF, leading to poor planning and impulse control, and decision-making difficulties. An intervention that could help reduce these deficits and in turn help weight loss maintenance is physical activity (Fellows & Schmitter-Edgecombe, 2018).
One study aimed to investigate the executive profile in OB and morbid obesity (MO), and to explore the role of physical activity (PA) and irisin (hormone associated with some of the positive effects of PA). 114 participants were included (21 OB, 44 MO and 49 healthy controls-HC) in the study and assessed with the Wisconsin Card Sorting Test, Stroop Color and Word Test, and Iowa Gambling Task (Fagundo et al., 2016). Results showed a similar dysfunctional profile on Decision-making in OB and MO compared with HC. Thus, no specific neuropsychological profiles between OB and MO could be clearly observed in the study sample. However, a negative correlation was found between irisin and executive functioning. These results show a specific executive profile in OB and a relevant and negative modulation of irisin on executive functioning. Although irisin might be a promising target for the treatment of OB, its effects on cognition might be considered when thinking about its therapeutic use.
Another research examined the impact of a 30-min bout of moderate-intensity aerobic exercise on EF among adults with overweight/obesity and type 2 diabetes mellitus (T2DM), employing a widely used experimental paradigm (Vincent & Hall, 2017). Thirty adults with overweight/obesity and T2DM were randomly assigned to moderate (30% maximal heart rate reserve) and minimal (r.p.m. 30-50; workload 5) intensity aerobic exercise. Pre-exercise to post-exercise changes in Stroop interference and Go/No-Go scores (inhibitory control) were compared across conditions. Primary analyses revealed no overall effect of exercise condition on changes in inhibitory control performance. Post-hoc moderation analyses indicated that Stroop interference scores were reduced, following moderate exercise among female participants and among those who were more physically active. This study revealed no reliable benefit of acute aerobic exercise for overweight and obese individuals living with T2DM overall.
Structural and Functional Brain Changes in Obesity
One of the first studies on this matter investigated how lean and overweight/obese (OO) adults differed in their food choices and how brain structure and cognition may be associated with those choices (Cohen, Yates, Duong, & Convit, 2011; Spencer, Korosi, Layé, Shukitt-Hale, & Barrientos, 2017). As part of an ongoing study on diabetes and the brain, participants had routine blood work and a research MRI, received a battery of neurocognitive tests, and were instructed to keep a 3-day food diary. The lean group ate more high-quality foods and less low-quality foods compared to the o/o group. In the OO group, high quality food choices were associated with orbitofrontal cortex volume. The lean group performed better than the OO group on neurocognitive measures of executive function, and on attention and concentration tasks such as the Digit Symbol Substitution Test. Taken together, these preliminary data suggest that in obesity, poor food choices are associated with frontal cognitive impairments that may be the result of decreases in OFC volume.
Later, one more work examined associations of empirically derived cardiovascular disease risk factor domains with cognition and brain structure (Gonzales et al., 2017). 124 adults underwent neuropsychological and cardiovascular assessments and structural MRI. Principal component analysis of nine cardiovascular disease risk factors resulted in a four-component solution representing 1, cholesterol; 2, glucose dysregulation; 3, metabolic dysregulation; and 4, blood pressure. Separate linear regression models for learning, memory, EF, and attention/information processing were performed. Findings suggest that higher blood pressure was associated with poorer learning (B = −0.19, standard error = 0.08; p = .019), memory (B = −0.22, standard error = 0.07; p = .005), and EF performance (B = −0.14, standard error = 0.06; p = .031), and lower cortical thickness within the right lateral occipital lobe. Elevated glucose dysregulation was associated with poorer attention/information processing performance (B = −0.21; p = .006).
The most recent work on this subtheme to date aimed to determine the effects of OB on white matter microstructure and potential implications for cognition in a large cohort of healthy adults (Dekkers, Jansen, & Lamb, 2019; Zhang et al., 2018). 1.255 participants (50% females, 19-80 years, BMI 16.8-50.2 kg/m2) with diffusion-weighted magnetic resonance imaging at 3T were analyzed. Tract-based spatial statistics (TBSS) probed whether BMI and WHR were related to fractional anisotropy (FA). Results showed that higher BMI and higher WHR were associated with lower FA in multiple white matter tracts (p < 0.05, FWE-corrected). Besides, obesity was linked to poorer EF and lower processing speed through lower FA in callosal and associative fiber tracts (99% (CI) > 0.
Conclusions
According to the three-step methodological approach used in this article, the main goal has been achieved. Four perspectives have been identified: effects of body mass index on executive functioning, executive functioning in children with overweight and obesity, physical activity for adult obesity and structural and functional brain changes in obesity. Research focused on the first perspective found that higher BMI was associated with lower attention and EF in male HF patients, especially those with severe OB. These patients may therefore have more difficulties with the HF treatment regimen and may have lower outcomes (Hawkins et al., 2014). Studies on executive functioning in children with overweight and obesity mention that overweight children exhibited slightly poorer attention shifting, WM updating, and affective decision-making abilities as compared to normal-weight children. On the other hand, post-hoc moderation analyses have indicated that Stroop interference scores were reduced, following moderate exercise among female participants and among those who were more physically active. Finally, preliminary data suggest that in obesity poor food choices may be associated with frontal cognitive impairments that may be the result of, or contribute to, decreases in OFC volume (Cohen et al., 2011).
This review article has also found that patients with obesity have a lower performance in executive functioning tasks than healthy individuals. However, overweight patients only had important deficits in working memory and inhibition tasks. Several studies have found that there are not significant differences in cognitive flexibility, Decision-making, verbal fluency, and planning. Likewise, few studies have compared healthy and obese patients in verbal fluency and planning tasks so that it can be stated that there are not significative differences between groups. On the other hand, neither age, nor gender moderate the effects of obesity in executive functioning.
It has also been found that difficulty maintaining weight loss and difficulties adjusting and adhering to post-bariatric lifestyle changes have been used as evidence to support the idea that individuals with executive functioning difficulties may have a propensity to become obese (Boeka & Lokken, 2008). Others have suggested that making good food choices in modern life requires forethought, planning and good self-regulation in order to avoid overeating (Davis, Patte, Curtis, & Reid, 2010; Duchesne et al., 2010). These are skills which require good executive functioning abilities and so there is a suggestion that impaired executive functioning leads to obesity via poor food choices. This idea might also fit with the findings from the current review that distinctions between obese and non-obese individuals tends to occur on tasks measuring planning, problem-solving and decision-making, abilities needed to make good food and lifestyle choices.
One of the limitations of previous studies which explored the association between weight status and cognitive function was using BMI as the only obesity index (Oliosa, Zaniqueli, Alvim, Barbosa, & Mill, 2019). Instead, body fat percentage has been suggested as a better overall body obesity, predictor than BMI. This is because BMI as a measure of overall obesity does not account for varying proportions of fat, bone and muscle mass (Nooyens et al., 2007). Furthermore, it has been shown that the association between body fat percentage and BMI is different among different ethnic groups (Deurenberg, Yap, & Van Staveren, 1998), and body fat percentage is a better predictor of metabolic risk factors than BMI in children and adolescents (Oliosa et al., 2019).