1. Introduction
The Social Determinants of Health (SDH) are all those conditions (events, characteristics or other definable entities) that directly or indirectly influence the life course, the health of individuals and inequalities and inequities in health (Lema-Anón. 2020). Moreover, depending on their action and interaction between different levels of organization, they establish the health status of individuals and their population groups (Lema-Anón. 2020). That is why it can be said, in a broad sense, that they serve to understand the causes of problems and understand them in the context of different political, economic, social and cultural circumstances, which is relevant both in the practice of public health and in the interventions derived in the framework of public policies and possible essential actions from macro and microterritories.
Currently, the persistent and complex reality of social inequities and their determining role in the health status of individuals, families and communities has made the debate on social justice a central issue in the framework of public health. That is why, around this topic, the academic and political world orbit to elucidate the determining factors in the appearance of diseases for population groups, where it becomes clear that the most deficient health conditions are found in the excluded and vulnerable sectors (Pinones-Rivera, Liberona-Concha and Leiva-Gómez, 2021).
This social approach and its determinant relationship in health conditions, has been addressed by the World Health Organization (WHO, 2018) in different assemblies and communiqués, including the Declaration of Alma-Ata (PAHO,1978). the Ottawa Charter (PAHO, 1986). the Declaration of Adelaide (1988) the Declaration of Sundsvall (OMS. 1991). the Declaration of Jakarta (WHO, 1997), the Fifth World Conference on Health Promotion in Mexico (WHO, 2000) and the Bangkok Charter (WHO, 2005); and the formation of the Commission on Social Determinants of Health (2009), whose report recommended improving the living conditions of the population worldwide, combating the unequal distribution of power, money and resources, as well as frequent measurement and analysis of this problem, for which purpose the effects of interventions by both public and private entities should also be evaluated.
In order to contribute to the last recommendation of the SHD Commission, it is necessary to have instruments that allow showing plausible results based not only on the diagnosis, but also on the possible population changes originated from the policies, so the objective of this work is to analyze the scientific evidence on the instruments used for the measurement of the Social Determinants of Health. Given the intention of promoting sustainable, healthier, fairer and more inclusive societies as a guiding principle of public health, the need arises to measure, monitor and analyze the Social Determinants of Health (Mújica and Moreno, 2019), which is why this practice is considered a systemic task that provides real information on the situations, becoming a tool that allows to generate capacity for action to pursue this purpose.
Through an integrative documentary review, we sought to learn about the research conducted, the instruments and means used, among others, and thus have a theoretical basis to define objects of study, develop hypotheses, establish relationships between studies, categorize variables and identify gaps to contribute to the advancement of this objective, thus, its results become input for professionals from different disciplines and researchers interested in this field of public health.
2. Method
An integrative documentary review was carried out of publications in scientific journals that evidenced the measurement of the SDH, taking the proposal of the Commission on Social Determinants of Health as the basis for the consolidation of the SDH to be included in the instruments.
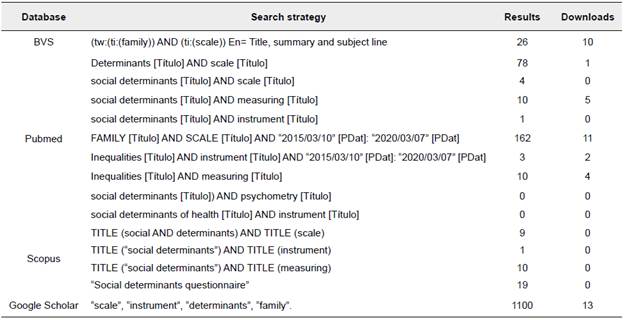
For the identification and selection of articles, a search of scientific literature was carried out in the specialized databases of the Virtual Health Library (VHL), Pubmed, Scopus, and the Google Scholar search engine. The process used the Boolean operator AND and the keywords "social determinants of health", "instrument", "scale", "evaluation", "tool", "measuring", "monitoring", "psychometry", "Determinantes Sociales de la Salud", "instrumento", "escala", "evaluación" y "herramienta", which were verified in the thesauri DeCS and MeSH (see Table 1).
Inclusion criteria were established as follows: year of publication between 2010 and 2020 (2 years after the publication of the SSD Commission), English, Spanish or Portuguese language; availability of full text access and publication in journals indexed or approved in the PUBLINDEX bibliographic index (Colombia)1. Exclusion criteria were defined as gray literature documents and those articles with unvalidated questionnaires, reflection or thematic review on the SDGs.
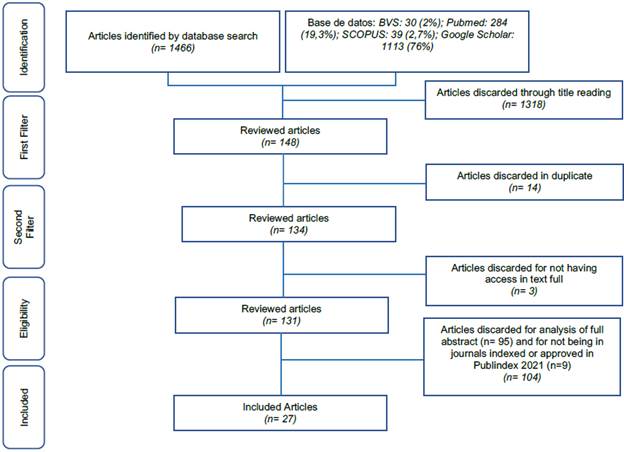
A total of 1466 articles related to the object of the search were found with the highest number of results in Google Scholar (76%) (see Figure 1). In a first filter based on reading the title, 1318 were discarded because they were considered irrelevant to the object of the study, leaving a total of 148 manuscripts for the second phase. On the other hand, 14 duplicate articles and 3 articles were excluded because they did not have access to the full text.
The information of the remaining 131 was consolidated in an Excel matrix, in which the following variables were analyzed: title, database, journal, authors, abstract, year of publication, country, language, query link, method, population and relationship with the DSS in terms of their measurement as official surveys, indicators or validated instruments. Similarly, in the last filter, 95 articles were discarded after analysis of the complete abstract and 9 because they were not found in PUBLINDEX I 2020. Finally, the review was carried out with 27 manuscripts that met the inclusion criteria.
The analysis of the information from the articles was carried out with the ATLAS.Ti version 9 software, licensed by the Library Center of the University of Caldas. For the coding of the data, some preliminary categories were considered that guided the process as they were considered fundamental in the research process: health condition and population to which the research was directed, type of research, methodological process of measurement, instruments and their validation (psychometric tests and statistical measures). source of consultation of the information. indicators.
For the development of the research, the ethical parameters of Resolution 8430 of 1993 (Ministry of Health, 1993) and the Declaration of Helsinki (World Medical Association, 2017) were adopted. Ethical endorsement was also obtained from the Faculty of Health Sciences of the University of Caldas (Act 001 of February 17, 2021).
3. Results
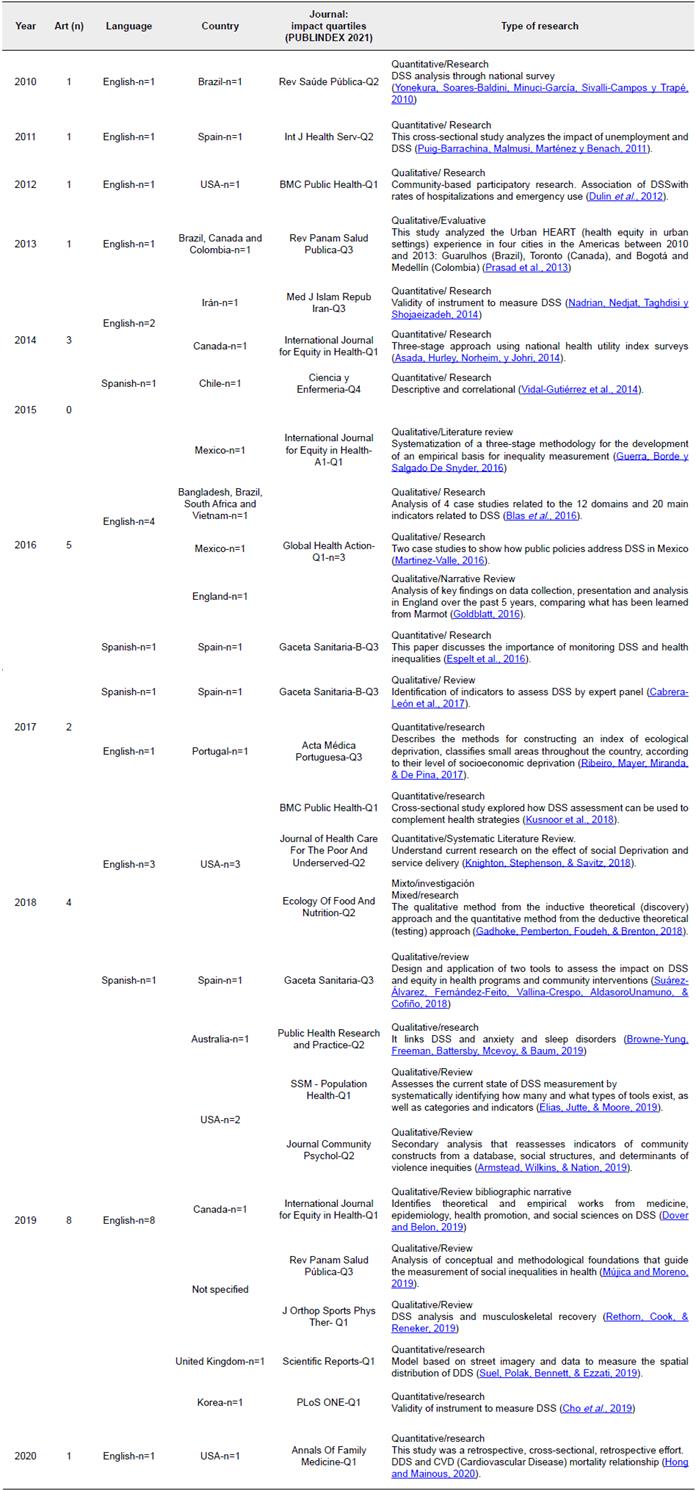
The year 2019 saw the highest number of publications (n=8), English the predominant language (n=22) and the USA (n=7) the country with the most publications, followed by Spain (n=4) (see Table 2).
According to the approach and type of study, quantitative (n=12), qualitative (n=14) and mixed (n=1) perspectives were found. The former analyzed indicators, domains, tests, validations; while the latter focused on tools, content analysis (conceptual) and methodological foundations of DSS measurement. In contrast. research results manuscripts predominated (n=15), followed by systematic, thematic, narrative, narrative bibliographic reviews (n=11) and an evaluative study (n=1) (see Table 2).
The age groups in which the instruments have been most commonly applied are 18 years and older, followed by the age groups 15 and 24 years, 20 and 64 years, 25 and 64 years, 22 and 70 years, and for general population (Browne-Yung, Freeman, Battersby, Mcevoy, & Baum, 2019; Hong & Mainous, 2020; Knighton, Stephenson, & Savitz, 2018; Prasad et al.. 2013; Ribeiro, Mayer, Miranda, & De-Pina, 2017; Suel, Polak, Bennett, & Ezzati, 2019; Suárez-Álvarez, Fernández-Feito, Vallina-Crespo, Aldasoro-Unamuno, & Cofino, 2018). Regarding health conditions, it was found that the instruments were applied to consultants with no diagnosis (n=3), high burden of cardiovascular comorbidity (n=2), anxiety disorder (n=1), healthy population (n=11) and no specific information (n=10). The settings in which the measurements were taken were clinical (health posts), institutional (educational centers, universities, homes) and community (canteens, neighborhoods).
Seventy percent of the manuscripts were published in journals with a high impact factor in quartiles Q1 and Q2; 26% and 4% were found in Q3 and Q4, respectively, according to the STI Specialized Journal Indexing and Approval System (Publindex-2020).
4. Instruments
Table 3 (see Annexed A) shows the 27 instruments identified in 19 articles, while the remaining articles do not explicitly refer to them. It can be seen that only four of them originated in the Latin American continent (14.8%). The country where the largest number of instruments was generated was also the United States (n=8), followed by Canada (n=4), Spain (n=3) and Mexico (n=2). With respect to language, it is possible to observe a low presence of instruments originally written in Spanish (22%), while 74% were in English.
It was found that the social determinant of health most frequently evaluated was the health system (70%), followed by education (63%) and, in third place, economic income and housing (55%). In relation to occupation, 40% of the instruments measured it, as well as public policies, which were included as a SDH in 11% of the instruments.
Determinants such as age, gender and ethnicity were assessed in 41%. Socioeconomic stratum was not directly assessed in any of the instruments in this review. Although the instruments focus on measuring both categories of determinants, the structural determinants are analyzed to a greater extent, estimating a ratio of 2:1 with respect to the intermediate determinants.
Regarding the form of application, 44% of the questions were asked in a mixed form (closed, open, Likert-type and/or dichotomous); 19% were Likert-type; 11% and 7% were closed and dichotomous, respectively, and in five instruments the way of asking questions was not explicit (19%). Of the 27 instruments identified, 20 were available. On the other hand, 21 instruments reported information on their validation process, 85.7% reported validity data. One of the instruments reported substantial adaptations for its use (see Annexed A).
5. Discussion
Health inequities are also present in so-called first world countries such as the USA and Spain. However, they are much more evident in third world countries, especially in Latin America, Asia and Africa. From the findings of this documentary review, it is evident that in Latin America the measurement of SDH has been limited, which implies that it is necessary to have monitoring and analysis instruments for decision-makers, since this is a fundamental process in the provision of resources and generation of capacities aimed at addressing the specific health problems of the populations. In this sense, Mejía and Lachaud (2020) state that it is necessary to have tools to identify health and social needs.
In the present review, the environments in which the instruments were most frequently applied were community and institutional, especially in the healthy population. On the other hand, they were infrequently applied in that population that had a specific diagnosis, in this regard, Balhara and Irvin (2020) highlight the environment and community participation are a learning that transforms the DSS, serving as a lens to examine biases, which allows a positive impact on the context of the social problems faced by people, along with exposure to realities that are often invisible in clinical settings.
Consequently, the measurement of SDH in various frameworks requires the approach of knowledge about the health conditions of the general population in its historical, social, cultural and political context, as well as the need to expand these conditions with the use of strategies based on the interpretation of data and indicators to develop adequate and appropriate recommendations that favor interventions and contribute to the strengthening of social inclusion and health for all, in accordance with the fundamental right to health regulated in Colombia (Congress Of Colombia- Law 1438, 2011).
One of the population groups in which less work was found were children, although they have been the subject of extensive action by the State, evidenced in the National Policy on Children and Adolescents 2018-2030 (Colombian Institute of Family Welfare, ICBF, 2018) and different programs that favor their development and care. such as Maternal and Child Care, FAMI Homes, Community Welfare Homes (Aranda-Aranda, 2018), Comprehensive Care Program for Colombian Youth, Profamilia Youth Network (2021). In this regard, it is noted that objective data can be obtained on the DSS in this population, which in the future will allow monitoring how the implementation of these concrete actions is related to the results, by making possible work on the DSS that has an impact on their projection under the framework of social justice (Janus, Reid-Westoby, Raiter, Forer, & Guhn, 2021 ).
In this regard. Hommes, Drees, Geffert, Philipsborn and Stratil (2020), highlight how "most references on early childhood focus on physiological and pathological development patterns or on the long-term preventive effect of vaccines" (p. 5); denoting little analysis of the social and economic determinants that influence child development, these exclusively biomedical reasons do not comprehensively address the causes that explain their health conditions, so the problems are perpetuated over time with partial solutions.
On the other hand, since 1974, attention has been drawn to the relevance of factors other than the health system as determinants of health status (Lalonde, 1981), and it was found in this review that some aspects of the health system are the most frequently measured, leaving aside others that are relevant for the performance of HSS evaluations. It should be noted that health not only takes precedence as a biological good/aspect, focused only on the salutogenic well-being of the population, but also as "a social structure and related factors" (Cho. Lee. Lim and Lee. 2020. p. 9), which constitute mediating factors between the balance between inequalities and contribute to a more comprehensive society.
In this aspect, the importance of complementing information on the health system with information on social aspects is highlighted. as Downward, Rasciute and Kumar (2020) state, when they refer that it is necessary to implement "longitudinal data, fixed effects controls and instrumental variables estimation" (p. 6), to address health as a social determinant, and not only based on social aspects, given that the relationship between both -health and society- allows defining to what extent health investment generates better collective results in the communities.
This review found that education was the second most evaluated determinant in the instruments identified. In this regard, Broch, Lisboa-Riquinho, Becker-Vieira, Roese-Ramos and Aparecida-Gasparin (2020) associate illiteracy with precarious living conditions and poverty, since the lack of opportunities, mainly reflected in insufficient economic income, leads to a disadvantage that affects health conditions. Likewise, education affects the social position of an individual, and this in turn determines the distribution of health and well-being in the population (Mújica and Moreno, 2019). Under these conditions, education is constituted as a strength of society, by allowing to guide the disposition of power, wealth and resources, whose distribution under conditions of equitable access allows the constitution of more inclusive, equitable and healthy societies.
The results show how individual income is considered within the DSS addressed in the instruments, being a condition that helps define the socioeconomic level and is related to the economic and social factor, while determining aspects such as the neighborhood where the person lives, belonging to a low, medium or high socioeconomic stratum, which is closely related to the characteristics and possibilities of education, access to health, family history, prestige, political power and others (Agualongo-Quelal and Garcés- Alencastro, 2020). Returning to the above, Cho. Lee. Lim and Lee (2020). state that "income is the representative index and a factor that decides socioeconomic status, and the lower the income level, the more difficult it is to pay attention to health" (p. 9). To this extent, it can be considered that the absence of income is an important cause of social inequality, to which is added the distribution - deficient and scarce - of access to social services and productive resources, which become insufficient employment opportunities, deplorable salaries and concentration of power and wealth towards the most favored (Arias-Ramírez, Sánchez-Hernández and Rodriguez-Morales, 2020).
Occupation is closely related to income, which is why it is considered a key element for building social capital and enhancing the development of social skills (Asokan et al.. 2020).That is why the association between the type and condition of work with health status has been studied and is part of the report of the WHO Commission on Social Determinants of Health (Matilla-Santander and Martínez-Sánchez, 2018). Jobs with low wages, unstable, without normative regulation, with precariousness in aspects of job security, are associated with worse health conditions, problems in mental health status, suicidal thoughts and actions, as well as threats on food security (López-Ejeda, Vargas and Marrodán, 2020). In contrast. in the present review, occupation was not a DSS included in all the instruments used.
From another perspective, the present review did not find allusion to the socioeconomic stratum determinant in a direct way, so it is not associated with variables such as biological, physiological and environmental mechanisms and how these variables affect the life course and is especially relevant in health outcomes (Davies et al.. 2019). Similarly. Cho et al (2019) assert that to overcome persistent inequalities in the health sector, universal health coverage is not enough, but rather policies and programs that improve socioeconomic status as a causal determinant of health are needed. This is demonstrated in that countries such as China have shown public health problems such as multimorbidity, which are more prevalent in elderly men from lower socioeconomic strata (Zou, Wang, Bhura, Zhang, & Tang, 2020). As a consequence of the above, social class has been used as a resource to classify the population and make health inequalities visible, but rarely to understand the social processes of causality that help explain health outcomes that are products of complex interactions (Wami et al.. 2020).
It should be noted that living conditions do not depend only on a specific determinant, such as race, but are influenced by a set of determinants such as ethnicity, socioeconomic status, values and culture, becoming factors that show the need to assume the diversity and heterogeneity involved in these variables and their impact on health (Assari & Caldwell, 2018). Ethnic, racial and gender differences are structuring axes of social inequality and inequity in health in regions such as Asia, Africa and Latin America; shaping structural disparities of well-being, in aspects as important as recognition, autonomy and full enjoyment of rights of women compared to men and of Afro-descendant and indigenous communities in relation to the rest of society. These inequalities are sometimes reinforced in the different stages of the life cycle and interact with geographic asymmetries, making them relevant to issues of social inclusion and equity (ECLAC. 2021).
The findings show that DSS such as age, gender and ethnicity, which have been considered as a cause of inequities throughout history, have been measured very little in comparison with the other determinants. This is supported by previous studies such as that of Young et al. (2020), in which the lack of reviews on specific data on these topics (race, ethnicity, age), as well as on the implications of socioeconomic status, is evident, since these determinants are considered difficult to measure in a comparable manner between countries. It is therefore not surprising that very little related research is available compared to studies that focus on inequalities associated with wealth, education or employment (Victoria et al.. 2019).
In this regard, several of the declarations of the WHO international conferences on health are reiterative in the urgency of modifying economic and political structures to reduce health inequities and approach the goal of health and well-being for all (González-Rojo, Álvarez-Dardet and López-Fernández, 2018). Governments, through their political- economic decisions, positively or negatively impact health inequity (Gómez, González, & Ramirez, 2019), so these aspects should be objectively measured as a baseline to have a clear notion of their effect. The DSS could become a starting point to establish not only variables but also associated factors that have an international and historical application.
6. Conclusion
Measurement should focus on diagnosing, describing, analyzing and proposing responses to problems of individual, family and community impact that can be expressed in public policies. The scientific evidence analyzed made it possible to identify that there is no homogeneity in the different instruments used to evaluate the Social Determinants of Health, which is why some fundamental conditions that would explain inequalities and inequities are not included.
In order to carry out comprehensive analyses and comparisons, it is not possible for this approach to continue to be partial, which leads to the need for the design of generic instruments to measure both the structural and intermediate dimensions and thus become international guidelines for their evaluation.