1. Introduction
Tuberculosis (TB) represents an important cause of morbidity and is one of the ten leading causes of mortality in the world. Until the appearance of the coronavirus (COVID-19), it was the main cause of mortality caused by a single infectious agent, above HIV/AIDS (WHO/WHO, 2021). The 30 countries with the highest TB burden accumulate almost 90% of global cases each year, associated with conditions of poverty. People with TB often experience economic problems, vulnerability, marginalization, stigma, and discrimination (WHO/WHO, 2020).
With the onset of the COVID-19 pandemic at the beginning of 2020, the provision of TB-related services changed due to confinement measures, the population's fear of being infected in health services, and the redirection of medical personnel towards the attention of the pandemic. The pandemic has reversed years of global progress in the fight against TB, and, for the first time in more than a decade, TB deaths have risen. Approximately 1.5 million people died from TB in 2020, including 214,000 HIV-positive people, while in 2019, there were 1.2 million HIV-negative and 209,000 HIV-positive people (WHO/ WHO, 2021).
Diagnoses also dropped. Country notification decreased from 7.1 million in 2019 to 5.8 million in 2020. Likewise, there was a 21% drop in the provision of TB preventive treatment from 3.6 million in 2019 to 2.8 million in 2020. In addition, the number of people treated for drug-TB resistance fell by 15%, from 177,000 in 2019 to 150,000 in 2020. According to WHO projections, the number of people who develop TB and die could be much greater in 2021 and 2022. In addition, the impact of the pandemic on the economy and poverty levels represents more than a lost decade, which will contribute to increasing the social determinants of TB (WHO/WHO, 2021 ).
TB continues to be a public health problem in the Americas region, with 290,000 cases in 2019 of all forms of the disease. Despite the slow decline in deaths in recent years, the incidence continued to rise slightly. Information on preventive treatment remains limited, and treatment outcomes do not show favorable changes. The TB situation in the region reflects the persistence of social conditions and risk factors that directly affect vulnerable populations (PAHO, 2021).
In Colombia, in 2020, 11,390 people were infected with the disease, of which 10,632 were new cases, 65% were men, 12.5% were under 15 years of age, and 12.8% had coinfection with HIV. It occurs more frequently in the urban area with 86%, and in terms of vulnerable and risk populations, 7.0% of the cases correspond to people deprived of freedom, 3.9% are indigenous, 3.3% are Afro-Colombians, 3.1% are homeless, 2.1% are health workers and 1.4% come from abroad (INS, 2021).
In the municipality of Cali in 2020, 911 people entered the program, of which 89% were new cases, 71% were men, 2% were under 15 years of age, and 9% had coinfection with HIV. Most of the cases occurred in the urban area, with 96%, and in relation to vulnerable populations, 11% correspond to people deprived of freedom, 0.3% indigenous, 13% Afro-Colombian, 5% homeless, 0, 4% health workers and 2% migrant population (Secretaría de Salud Pública Municipal de Cali, 2021).
The general panorama shows the persistence of TB as a serious public health problem associated with social vulnerability and the current situation resulting from the pandemic; it also shows setbacks in some achievements and processes of TB prevention and control. It is recommended to continue studying the social conditions that influence the contagion and that affect treatment success. Regarding this, in Colombia, the Strategic Plan called "Towards the end of TB 20162025" (Min. Salud de Colombia, OPS, OMS, 2016) proposes to characterize the most affected populations, overcoming the monitoring of the program's macro indicators. It also delves into the characterization of the people most affected by TB at the territorial level: who they are, where they live, and what determinants affect their health conditions. This will make it possible to develop differential actions and prioritize interventions according to specific needs.
Following this approach, a research project was developed in 2020, whose purpose was to characterize the social vulnerability of people affected by TB in Cali - Colombia, belonging to the cohort of patients of the year 2018. The characterization was carried out through a mixed study based on the AVEO model (Assets, Vulnerability, Opportunity Structure) that analyzed social vulnerability based on the relation between the people's assets and liabilities and the opportunities offered by the context (Kaztman and Filgueira, 1999). This article presents the main results, triangulating the quantitative and qualitative results.
2. Methodology
The research had a mixed design that combined quantitative and qualitative components. It is part of explanatory studies that seek to deepen quantitative findings through qualitative techniques (Hamui-Sutton, 2013). First, a structured instrument was applied whose purpose was to characterize, from a multidimensional perspective, the conditions of social vulnerability of people with TB and later, based on focus groups and interviews, to understand, from their voices, how these conditions of social vulnerability are articulated with the disease.
The population that responded to the survey was people registered in the TB patient database of the Municipal Health Secretariat (2018 cohort: 754 people), over 18 years of age, residents, and treated in Cali. All the people who could be contacted and agreed to participate were surveyed, a total of 136, corresponding to 18% of the cohort. The exclusion criteria were presenting an altered state of consciousness at the time of data collection, being homeless, being deprived of liberty, being institutionalized in a psychiatric center, and having died.
The survey was designed based on validated instruments, making questions related to the AVEO theoretical model in different dimensions, namely, sociodemographic, biological, psychosocial, socioeconomic, environmental, and cultural (Golovanevsky, 2007). The assets, liabilities, and structure of opportunities were assessed in each question. Items for the sociodemographic, biological, and psychosocial vulnerability characterization were taken from Colombian population surveys: National Health 2007, Longitudinal Social Protection 2012, and Integrated Household 2013. From the document "Survey to determine direct and indirect costs due toTB and to estimate proportion ofTB-affected households experiencing catastrophic total costs due to TB," questions were asked to characterize the clinical approach to the pathology. Items related to the environmental, psychosocial, and socioeconomic dimensions of vulnerability were selected from the "Social Risk Survey" and, finally, from the "BARCAS 2011 Social Capital Barometer" were included items related to the psychosocial vulnerability, environmental and cultural dimensions. Some items of the instrument addressed questions with two temporalities: 1) during TB treatment and 2) in the time window of data collection.
After the instrument design, the pilot test was carried out with people who were part of the population, but not of the sample, adjustments were made, and its application was carried out. The survey lasted an average of 60 minutes after the presentation of the study, resolution of doubts, and signing of informed consent. Due to typical situations of the pandemic and its management, in those cases in which the face-to-face meeting was not possible, the computer/cell phone-assisted modality was used to collect the data, a situation in which the informed consent was previously sent in Google forms format for approval.
Initially, an exploratory data analysis was carried out to observe each variable behavior and identify extreme values and missing values. Subsequently, the absolute and relative frequencies of the categorical variables were determined, and measures of central tendency and dispersion were estimated as Mean ± Standard Deviation of the numerical variables. The analyzes were developed using Stata 16 ® and IBM SPSS 24 ® software.
In the qualitative component, an individual interview, a group interview, and a focus group were conducted to present the results of the survey, discuss them, and increase them by the participant's experiences. These were selected among the respondents, considering differential characteristics related to the socioeconomic level and their health system affiliation. A focus group was carried out with seven people and an interview with two people from socioeconomic strata 1, 2, and 3 (lower), with subsidized healthcare coverage or without healthcare coverage (without payment capacity and subsidized by the State). The individual interview was conducted with a person from a higher socioeconomic stratum, belonging to the contributory healthcare regimen (with payment capacity).
The focus group and the interviews were carried out in places agreed upon by the participants after applying the informed consent, and with a duration of 2 hours. They were conducted by a research team professional who was accompanied, in the case of the focus group, by other members of the team, who had the role of observers, reporters, and technical support, all with experience in the technique. Each focus group and the interview were recorded, transcribed, and processed using the Ethograph V6 software, according to the categories initially defined and those that emerged in the process.
The collected information was integrated for qualitative processing. The thematic content analysis technique was used, which consists of an interpretation of the collected information, identifying what was explicitly verbalized and the meanings and senses of what was said by the participants (Díaz-Herrera, 2018). Initially, the recording units corresponding to text fragments in which an idea related to the research objectives is communicated were identified. These units were located in units of broader contexts based on the dimensions defined in the quantitative component that allowed their understanding in terms of meanings (Aigneren, 1999; Minayo, 2012). Finally, the triangulation of qualitative and quantitative data was made, suggesting hypotheses around the explanations and interpretations of the findings. To do this, the researchers held multiple meetings to discuss the results based on the categories of the AVEO model and other studies on the subject.
The study was classified as minimal risk, with approval by the Institutional Committee for the Review of Human Ethics -CIREH of the Universidad del Valle, with record number 019-020.
3. Results
The main quantitative and qualitative results are described by demographic, biological, socioeconomic, psychosocial, and habitat dimensions, at the end of which a summary table of assets, liabilities, and structure of opportunities is presented.
Demographic Dimension
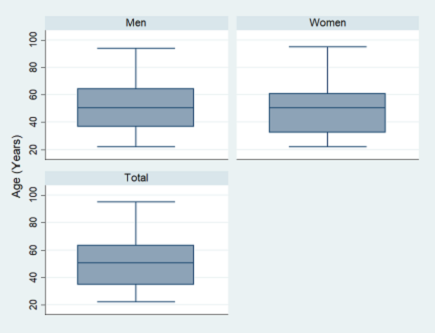
The studied population had a median age of 50 years, 62% were women and the majority were affected by TB at productive working ages (see Figure 1). Of the total, 40% reported not belonging to any ethnic group, 32% recognized themselves as Afro-Colombian, and 15% as indigenous. Regarding marital status, 43% were single and 43% were married or in a common-law marriage.
Biological dimension
84% of the participants were bacteriologically diagnosed with pulmonary TB, of which around 12% reported having a susceptibility test, about 1% were resistant to rifampicin and 7% had TB/HIV coinfection (See Table 1).Arterial hypertension followed by diabetes, asthma, and HIV were the most common comorbidities. About 7% report kidney disease without treatment.
Table 1 Clinical features of participants in a study on vulnerability to TB, District of Santiago de Cali Colombia 2021.
| Variable n=136 | n | % | |||
|---|---|---|---|---|---|
| TB type | |||||
| Pulmonary confirmed by bacteriology | 115 | 84,5 | |||
| Pulmonary not confirmed by bacteriology | 2 | 1,5 | |||
| Extrapulmonary | 19 | 14 | |||
| Diagnostic site | |||||
| Clinic | 34 | 25 | |||
| Private clinic | 69 | 50,8 | |||
| Public hospital | 29 | 21,3 | |||
| Other | 4 | 2,9 | |||
| Diagnosis by smear sputum microscopy | 104 | 76,5 | |||
| Diagnosis by swab microscopy | 9 | 6,6 | |||
| Diagnosis by culture | 33 | 24,3 | |||
| Diagnosis by molecular test | 5 | 3,7 | |||
| Diagnosis by another bacteriological test | 15 | 11 | |||
| Susceptibility testing | |||||
| Yes | 16 | 11,8 | |||
| No | 97 | 71,3 | |||
| NK/NA | 23 | 16,9 | |||
| Susceptibility determined by Molecular test | 1 | 0,7 | |||
| Susceptibility determined by LPA Line Probe Assay | 1 | 0,7 | |||
| Susceptibility determined by Culture | 7 | 5,2 | |||
| Classification according to susceptibility test | |||||
| Drug resistant to rifampicin | 1 | 0,7 | |||
| Sensitive | 5 | 3,7 | |||
| HIV Status | |||||
| Positive | 9 | 6,6 | |||
| Negative | 118 | 86,8 | |||
| The test has not been carried out | 2 | 1,5 | |||
| NK/NA | 7 | 5,1 | |||
Source: TB Vulnerability Study Database, 2021
According to the reports, there was clarity about how TB transmission occurs, which denotes an understanding of the origin of the disease, but they cannot clearly identify when and how they were infected. They identified interaction with vulnerable populations and attendance at hospital centers as the main routes of infection. They say: "I think that I got infected taking care of my grandfather in hospitals" (Focus group 2). It was easier for them to trace the possible contagion when it came from one of the relatives, however, the chain of contagion was not clear. They commented: "First, my brother started, who knows, since he is mentally ill, surely he went to receive a letter... and there are many sick people... they surely infected him" (Focus group 1).
The majority manifested delays in the diagnosis. They reported a succession of medical consultations motivated by symptoms such as cough without adequate resolution. This is indicated by the following statement: "Everything went wrong with the health insurance company; I had a bad cough and they sent me syrups" (Focus group 2). Another testimony refers that the treatment of comorbidities did not allow a diagnosis of TB: "I also suffer from hypertension and whenever I went with breathing problems, they treated me for hypertension and I did not go for hypertension, I had to argue ugly with the doctors" (Focus group 2). Another person says: "I was on dialysis three days, and then I came out with the disease... they did many tests and did not find anything, they ruptured me on all sides, they thought that were the lungs, one thing and another, in the end, they did the last tests and found it was tuberculosis" (Focus group 2).
Once diagnosed, most of them received convenient care for approximately six months of treatment (adherence) and ended successfully, that is, healed. It is mentioned: "They told me that I was receiving treatment at the Comuneros health center, which is a special health center for that; there is a doctor in charge of everything related to lungs and those diseases; I left in his hands, and he was a very good doctor" (Focus group 1). Another participant adds: "I was in treatment, great nurses, without complications, they treated me very normally, they told me: Don Luis, take your medicines that you will be better, I was improving... " (Focus group 2).
Some people stated that the treatment was very strong. They presented adverse effects, a situation that worsened due to the symptoms of the disease. This led to a reduction in their everyday life activities, along with psychosocial disturbances. In this regard, they mention: "I had a fever, vomit, headache at all times, after more or less three months I could not walk, I was sick in bed, I did not eat, it was very difficult" (Focus group 2).
Regarding comorbidities, they identified not having a chronic disease or not being a smoker as an advantage in dealing with TB. They say: "There they ask you, are you hypertensive? No. Are you diabetic? No. Better! Even I have never smoked, it is the greatest advantage that non-smokers can have, those who have smoked" (Focus group 1). Those affected by TB and who have comorbidities have stronger symptoms and experience a greater deterioration in their health. One participant pointed out: "It was in 2018, but around June or July that tuberculosis started, there were seven months of treatment here, plus three that I spent in that clinic receiving dialysis" (Focus group 3).
Table 2 shows the assets, liabilities and opportunity structure of the biological dimension.
Table 2 Summary of assets, liabilities, and structure of opportunities, demographic, and biological dimension
| Assets | ● Have treated/controlled comorbidities |
| Liabilities | ● Ethnicity and the female gender as a proxy for conditions of social disadvantage |
| ● Singleness (reduces financial and emotional support). | |
| ● Older age increases the probability of comorbidities | |
| ● Living with few people during treatment (reduces support networks) Physical deficiencies that limit daily performance | |
| ● Untreated comorbidities (hypertension, diabetes, HIV, kidney disease, etc.) | |
| Opportunity structure | ● TB care programs for people with or without ability to pay |
Source: self-made
Socioeconomic Dimension
The education level mainly achieved was high school (45%), followed by the elementary school (40%). 19% of people had technical, technological, and professional studies, while 4% indicated they had no level of education. Around 92% of them were not studying, considering that they are not of age to do so, education costs, lack of money and time.
In relation to the system by which they received health services, half of them were affiliated to the contributory healthcare system (they contributed based on their monthly income or are beneficiaries of someone who does). A little over 43% received healthcare coverage through affiliation to the subsidized regime (public resources for people classified as poor and extremely poor), and 4% were not affiliated.
Regarding the socioeconomic stratum where they resided, 89% lived in socioeconomic strata 1, 2, and 3, with stratum 1, that is the lowest, being the most representative with 34% of participants. They answered that they did not work during the treatment; some of them were looking for work and studying. They were occupied primarily in household activities, and secondly in independent work as "self-employed" (See Figure 2).
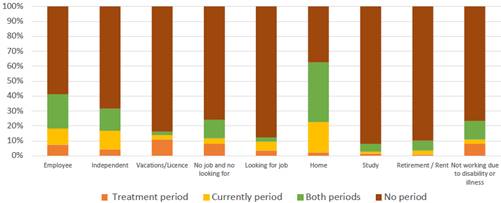
Source: TB Vulnerability Study Database, 2021
Figure 2 Frequency by types of occupations in participants in a study on vulnerability to TB, District of Santiago de Cali - Colombia 2021.
Half of the respondents were heads of the household, with economic responsibilities for support and income after and during treatment below the current legal monthly minimum wage (approximately $US 250), and around 15% received financial help from their partner or children to their subsistence. 47% considered that had no possibilities to access credit and 87% did not have credit cards. 38% lived in rental and about 20% and 10% received subsidies from State programs at the time of the survey and during the treatment, respectively.
Regarding goods and services available now and during treatment, around 70% did not have their own home in both and natural gas. Around 14% reported not having a refrigerator or stove, 47% did not have internet and 66% did not have a computer in any period. Approximately, 20% had means of transportation for their trips in the two periods.
In the reports, the advantage of having an employment contract at the time of acquiring the disease was evidenced as an asset, since it offered an income while they were unable to work due to the disease. Even those who were diagnosed at the end of a labor contract had health coverage and subsisted with the settlement. They say: "Since I was already leaving the company, they gave me the settlement and we bought food with that" (Focus group 1).
The possibility of contributing to the pension system and of having it for patients and their family members is also an important asset since it allowed them to have resources for care and to cover the out-of-pocket expenses associated with TB treatment. In an interview, one participant says: "Yes, I achieved the required time and weeks, and I am waiting for them to state the pension payment to start receiving it. On that side, thank God we do not have a lack of money, we have sustained ourselves (...) My wife has been the head of the household, she had a higher income, she was always with a work contract and now she receives her pension payment" (Individual interview).
Since most of the participants performed manual occupations with low income, family support networks were assets that allowed them to meet economic needs during the disease. An interviewee tells: "My brothers were aware of what I need for my son, if he needs something for school, until I could go back to work, and then I had to help again" (Focus group 1). Another identified asset was homeownership since it covers a basic need for shelter and protection, reduces costs and is a source of extra income. In this regard, they comment: "Fortunately, I received income from a room that I rent in my house, and that helped me a little for utilities" (Focus group 1).
In contrast, and operating as liabilities, the fact of not having a job or working in the informal sector evidenced levels of social and economic insecurity during treatment since, on occasions, they had to do odd jobs, even if they were sick, and use savings (in a few cases generally rare) or financial support from families. This situation put at risk the treatment since, if they were not living close to the health institution where they took the medication, the constant displacement implied an expense that many could not afford, as reported in the following testimony: "As I lost my job, it affected my transportation, I moved to a place closer to not pay for transportation" (Focus group 3).
A consequence of unregulated hiring is the lack of protection that the worker has at the time of acquiring the disease. Layoffs without guarantees of social protection were narrated: "I was sick, and they fired me. The company told me not to work anymore, they fired me, and I stayed at home, which made me even more depressed" (Focus group 3). Another situation that can increase the social vulnerability of patients and their families is related to employment opportunities after finishing treatment. Some participants managed to join the labor market, however, under disadvantageous conditions, for example, hourly work. In other cases, they had to change jobs due to fear of stigmatization and threats of dismissal. Concerning this, they say: "If you tell me that it came out positive, you have to leave, because here you are not going to infect your co-workers" (Focus group 1).
Table 3 presents the assets, liabilities and opportunity structure of the socioeconomic dimension.
Table 3 Summary of assets, liabilities, and structure of opportunities, economic dimension.
| Assets | • Belonging to any of the General Health and Social Security System regimes |
| • Living with few people during treatment (reduces contagion) | |
| • Living in socioeconomic strata 4, 5, 6 | |
| • Have your own and/or family home | |
| • Having utilities in home | |
| Liabilities | • Living in socioeconomic strata 1,2,3. |
| • Low levels of education | |
| • Unemployment during TB treatment | |
| • Not working due to disability or illness | |
| • The person with TB is the bread earner of household expenses | |
| • Low access to credit - Credit cards | |
| • Low access to State subsidies | |
| • Low access to internet and computers at home | |
| • Not having your own transportation | |
| Opportunity structure | • Almost universal coverage in the General Health and Social Security System |
| • Weakness of the labor market to absorb labor force | |
| • Provision of healthcare services to consult for health problems | |
| • Almost universal coverage of utilities |
Source: Self-made
Psychosocial and Habitat Dimensions
While men reported a higher frequency of living with two people currently and during treatment, in women the frequency decreased from more than three to one and two people currently. Nearly 77% of those surveyed cohabited with children and permanent partners in both periods. Regarding sharing a room with other people, no significant differences were found, in both periods they reported sleeping alone or with another person.
During the treatment, there was a suspension of the consumption of psychoactive, with subsequent minor relapse in the consumption of marijuana, amphetamines, opiates, tranquilizers, and hallucinogens. 13% had at least one member of the family who consumes tobacco, alcohol, and other psychoactive substances, while during the treatment the proportion of participants in this situation was close to 12%. On the other hand, the proportion of participants who consume tobacco and alcohol increased since the end of treatment, from 6.6% to 7.4% for tobacco consumption and from 0.7 to 21% for alcohol consumption.
High ratings of satisfaction with life were reported, slightly lower during the treatment period.Also, a weak support network of close friends and family, despite maintaining regular communication with them (See Table 4). 13% of the participants perceived discrimination during treatment, mainly attitudes of contempt and rejection, exclusion from family gatherings, and verbal aggression. The people that generate said discrimination were mainly health professionals, co-workers, and family members.
Table 4 Social aspects and life satisfaction of study participants on vulnerability in TB, District of Santiago de Cali - Colombia 2021.
| Variable n=136 | Me | IQR |
|---|---|---|
| Relatives with whom they maintain regular communication (excluding cohabitants) | 4 | 2 - 6 |
| Relatives with whom they have a close relationship | 3 | 1 - 5 |
| Number of friends they have | 2 | 0 - 5 |
| Current life satisfaction (Likert 10 pts) | 9 | 8 - 10 |
| Life satisfaction during treatment (Likert 10 pts) | 7 | 5 - 10 |
Me: Medium; IQR: Interquartile range Q1-Q3 Source: TB Vulnerability Study Database, 2021
16% participated in religious organizations during treatment to date, to a lesser extent in sports-recreational spaces, health organizations, and professional associations. A high proportion of the participants was satisfied with their parks, green areas, and, in general, public spaces close to where they reside. They indicated that they were satisfied with the offer of health institutions, food supply, and recreation centers, but less satisfied with the offer of cultural centers. Slightly more than two-thirds of the participants (78%) have not been victims of crime, however, around 75% rated insecurity as moderate to very serious. About 90% do not perform or did physical activity, they visited recreation parks or parties and discos.
In interviews, they pointed out that TB entered their lives but symptoms, medication effects, and physical and social limitations were variable. They highlighted the psychosocial impact of this disease related to depression, sadness, and isolation. They described it as limiting, causing great physical deterioration, life-threatening, and stigmatizing. This is described in one of the testimonies: "I turned completely yellow, it itched, I had spots on my skin, and I had moments of depression because I couldn't eat, I vomited everything I ate, and since I lost my job, I also had problems affording transportation cost" (Focus group 2).
They recognized that the formalization of the diagnosis marked a turning point in their lives from which they experienced alteration of the daily "normality". They emphasized the feeling of fear due to the severity and effects of the disease, surprise, and a certain shame for what TB represents socially. Also, the fear of transmitting it to others; physical and social isolation, and emotional damage. Some stopped their regular interactions and leisure activities because of the risks of exposure to environmental conditions related to the weather or because of exposure to other risks such as tobacco or alcohol, which increased the feeling of isolation. In one of the testimonies, it is stated: "I couldn't go out at night, I couldn't do that. I managed to do everything until 5:00 p.m., and that's it. Those places have a nocturne atmosphere, I couldn't drink a single wine" (Focus group 1).
However, with the beginning of treatment, they experienced a progressive improvement until it ended, and "normality" returned, that is, the development of work, family, and social activities and relationships without restrictions or fears. The following testimony describes this: "Once the treatment begins, the symptoms decrease and when the doctor told me that I was better, I went on a bicycle for the medication" (Focus group 1). They added sports practice or physical activity as reinforcement to improve the physical and emotional condition and as a sign of recovery.
In general, they felt well treated as patients and individuals by the health personnel. Although some health professionals took distancing and protection measures with masks, others did not. In either case, people affected by TB recognize the importance of precautions and, although the extreme protection measures of health personnel made them feel uncomfortable, they were aware of the risk to which medical staff was exposed.
In some cases, they felt that the health personnel did not adequately attend their demands and needs. Both during follow-ups and in emergency consultations, when they expressed the adverse effects of the medication, the answer was: "You should continue taking it." One participant commented: "A friend worked at a clinic that was not covered by my health insurance company. The doctors were very attentive there, they even treated me for free. A doctor told me I should stop taking the medication and go to the emergency room, but the health insurance company wanted me to continue taking it, although it made me feel sick" (Focus group 2).
Concerning the personnel of the TB Program of the Municipal Health Secretariat, their home visits to clarify doubts about the management of possible infections, the management of air and light in the home, and certain care and personal protection mechanisms, stood out. In addition to clarifying doubts and breaking down myths, the visits helped them to assume a less restrictive care and practices, which meant an emotional stimulus to continue the treatment and gradually overcome the disease. One participant commented: "When they performed the public health visit to me, congratulated me because I had many windows through which air entered and that is what they asked for the most (...) After they told me that I was healed, they visited two times more, I showed them the exam that everything was fine and that's it until now, they haven't come back" (Focus Group 2).
In the families and their closest relationships, they felt a mixture of fear for the risk of infecting someone, awareness of the care assumed or required, and attitudes of distancing, solidarity/support, and rejection. The surprise of getting the disease was accompanied by shame for suffering it, especially due to the meanings associated with TB and social rejection, which made it more difficult to emotionally handle intra-domiciliary isolation, the separation of personal utensils, social isolation and deal with comments and attitudes of rejection. In this regard, someone said: "At home, my sister told me "Oh no, separate your spoon and your plate and your glass and try not to go into the kitchen here because we can get infected". Another person said: "My sister, who is healthy, and her husband too, told me: Oh no, I'm not going back there until you're healed" (Focus group 1).
Others stated that the emotional and economic support of their families was decisive to overcome the disease and the effects of treatment. The following stories give an account of some experiences: "They gave me a room and my mom slept on the couches with my dad there. At night the cough was so tremendous that she couldn't stand it, during the day she was normally." He adds: "I have received a lot of support from my brothers and my mother (...) They have always had the opportunity to give me money, pay my rent, buy me food if I need something or pay my transportation me because from where I live it is hard for me because I spend about 70,000 Colombian pesos a week" (Focus Group 2).
Some persons faced the disease and treatment alone due to the fact of living alone and without emotional support to deal with complications related to TB and other diseases. One of the participants pointed out: "In 2017 I was in treatment for six months, and want to give me that again, as I live alone and my children abandoned me, as I have four surgeries, I am full of surgeries and I'm scared because I live alone, thank God I have my house, I live on the second floor, but alone. The women I've had, robbed me so I'm scared because I live alone, and I suffer a lot from suffocation, so I need this oxygen bullet" (Focus group 2).
Regarding the neighbors or close people, two positions were found: one that remains silent and does not make the disease public, and another that talks about the subject regardless of the reactions. First, they feel ashamed of having the disease and of what others think. Second, they consider that talking about it or simply not hiding what was happening is a way of dealing with the disease. Those who opted for the latter, found support and encouragement, as indicated in this testimony: "The first persons I told were the neighbors: I have this and this... Someone told me: 'It already gave me (He said) I was not scared, that was before when they sent you to a town, to a farm so that nobody would notice. That already gone out of style, it is a disease like the flu, and it already has treatment. So, you have to take good care of yourself'. The neighbors took care of me; they asked me how I was doing" (Focus group 1).
In general, the feeling of isolation, stigma, and finger-pointing disappears as the treatment progresses, the symptoms are reduced, and the physical condition improves: the effects of the medication decrease, people gain weight, the cough disappears, and it is possible to stop using masks permanently. This modifies the personal attitude towards being sick with physical and emotional limitations and reduces the feeling of being judged and considered a risk for others.
Those people who belonged to social and religious organizations before being affected by the disease, see their participation in these limited by the symptoms and the risk of transmitting it. To protect themselves from accusations and avoid contagion, they distanced themselves from the meetings, avoiding direct contact, and refusing to share what was happening to them. This is described in a testimony: "I did go to church, but on those days, my sister told me not to go out because I would infect people there, so I had to stay at home" (Focus group 1).
Regarding the surrounding where they lived, they mentioned three relevant aspects: mobility and connectivity with other parts of the city, security, and the availability and use of green areas.
Regarding the surrounding where they lived, they mentioned three relevant aspects: mobility and connectivity with other parts of the city, security, and the availability and use of green areas. Regarding transportation to attend medical institutions daily to take the medications, at the beginning of the treatment, they did it accompanied or in public transportation due to the adverse effects of medications. However, as the weakness and discomfort decreased, they used bicycles or walked until the delivery site. They did not refer to security problems that prevented them from moving, although they did mention concern about the lack of money for transportation. In general, they did not identify insecurity as a barrier to accessing treatment or going to follow-ups.
The participants affirmed the availability and use of green or recreational areas in their neighborhoods, but with restrictions due to insecurity. This story shows the experience of one of them: "In my neighborhood, there is a park and there is recreation for children, but it is difficult because sometimes there are gun-fights or people go to take drugs, so it is very bad, just yesterday a boy was killed in the park" (Focus group 2).
Table 5 presents the assets, liabilities and opportunity structure of the psychosocial and habitat dimensions.
Table 5 Summary of assets, liabilities and structure of opportunities, psychosocial and habitat dimensions.
• Source: Self-made
4. Discussion
Based on the findings described, it is possible to identify how social vulnerability is configured in people affected by TB, through the interaction between the components arranged in the AVEO model. The analysis is presented along with the theoretical model that supports the research, and the main findings related to assets, liabilities and the structure of opportunities are discussed.
4.1. Assets
Assets correspond to tangible or intangible resources available to an individual or their close networks, allowing them to take advantage of opportunities, access goods and services, or obtain satisfaction to deal with social, biological, and psychological effects of TB, as well as maintain treatment until its successful completion. They will also be understood as capacities, in the sense that allow the mobilization of other resources/assets (Golovanevsky, 2007).
The fact of not using psychoactive drugs during TB treatment constitutes an asset that reduces biological and psychosocial vulnerability. In terms of plausible relationships, reducing, abandoning, or suspending psychoactive drug consumption increases the probability of treatment adherence, since it reduces dependence on psychoactive substances and possible abandonment of treatment due to problematic consumption. Likewise, it lessens the effects of poor nutrition or underfeeding, having a positive impact on the immune system and reducing the adverse effects of medications. On the other hand, it helps to avoid exposure to overcrowded spaces where psychoactive drugs are consumed, breaking or weakening the TB transmission chain.
This interpretation is consistent with some evidence. Studies describe psychoactive substance use and the adverse effects produced by this type of substance as determinants of abandoning TB treatment, in addition to other socioeconomic and sociodemographic conditions, including poverty, unemployment, low level of education, and being in extreme ages (under 15 years old and over 54 years old) (Culqui et al.. 2012; Culqui, Grijalva, Reategui, Cajo and Suárez, 2005; Muture et al., 2011; Liefooghe, Suetens, Meulemans, Moran and Muynck, 1999; Galván and Santiuste, 1998). However, although some studies find relations between those two aspects, others do not, such as the one developed byAnduaga et al., (2016).
In short, it is important to recognize the complexity and multidimensionality associated with the use of psychoactive substances and social vulnerability. In a systematic review, diverse results are shown concluding that the relationship between PAS consumption and the adherence and success of TB treatment is determined by multiple factors such as the type of substances, the time of consumption, the psychological and social effects of the substances consumed, and the ease and costs of accessing them, the frequency of use, and the psychosocial and socioeconomic conditions of people affected by TB, among other aspects. Differences were even found between active and latent TB (Carpio-Chanamé, Lindo-Cavero, Salguero-Alejos & Torres-Chala, 2021 ).
The knowledge that people affected by TB acquire about the disease through assertive communication with health personnel and the awareness of the seriousness that it represents for them and the people around them, is an asset since it favors adherence to treatment (Arriola et al., 2011, De Albuquerque et al., 2007; Morsy, Zaher, Hassan, & Shouman, 2003) and self-care and care of others. In a study, it was found that not having or receiving information about TB from health personnel caused the symptoms of the disease to be confused with another type of respiratory disease, which led people to take various alternatives, including not adhering to treatment (Zavala-Espinoza, De Jesús-Alejandro, Patrón De Treviño, and Cantú-Martínez, 2004). In this sense, the person affected by TB must understand that the disease is curable since in this way there is a greater probability that they will continue treatment (Sumartojo, Geiter, Miller, and Hale, 1997).
The information and understanding of the disease additionally reduce the adverse emotional effects generated by isolation, attitudes of rejection, and the separation of elements of daily use. This effect can be positively increased if the family or those who cohabit with the patient are adequately informed and sensitized. This shows the need for health services and health authorities to establish communication channels with people with TB and their families about the characteristics of the disease, the way to take the medications, possible side effects, and the risks of becoming infected or getting sick in domestic spaces (Heredia-Navarrete, Puc-Franco, Caamal-Ley & Vargas-González, 2012).
The use of isolation areas for patients in homes and reducing the number of people with whom they maintain close contact are also assets that lessen the chain of contagion. However, studies show that it is important, especially for those who live with few people, to maintain permanent communication, since the social representations of TB as a stigmatizing disease, the refusal to talk about it, and the lack of communication with family and friends, predispose abandonment or non-adherence to treatment (Orozco, Hernández, Usta, Alean & Camargo, 1998).
The support networks or social capital of people affected by TB to face the emotional, physical, and economic effects of the disease reduce vulnerability and increase the abilities of individuals and their families to maintain treatment, deal with the emotional and economic impact and achieve a successful treatment. These supports provide affection, help, a positive image, and information, operating as essential mediators in coping mechanisms for dealing with the disease (Yanguas & Leturia, 2006).
Along the same lines, aspects that favor adherence to treatment and help to deal with the disease are identified, including collaboration in daily care, that is, help for waste disposal, ventilating the home and giving good lighting, and isolation. In the same way, economic support, in terms of expenses for food, medicines, and transportation (Castro-Galarza, Cama-Cristóbal, and Fernández-Honorio, 2020). In emotional terms, the accompanied visits to healthcare centers and the demonstrations of affection are also identified. Other research shows that family support provides confidence and motivation to complete treatment and seek recovery, as well as to return to daily life (Quevedo-Cruz, Sánchez-Requín,Villalba-Porras, & Velásquez-Carranza, 2015).
On the other hand, the fact that a high percentage of people affected by TB, being from social stratum 1 and 2 and without having a job, are linked to the contributory regime system (have health insurance coverage) is an asset, since it allows them or their family members to access health services and it also indicates that someone in the family is linked to the formal labor market. The latter reduces vulnerability and improves the conditions to deal with the economic effects and out-of-pocket costs of treatment and reduces the anxiety and anguish due to lack of work, particularly when the disease restricts work possibilities.
Some studies show that having health insurance reinforces patient's adherence and continuity of the treatment, since it eliminates the costs of medicines and follow-up visits. Despite this, people may incur additional personal and/or family expenses, both medical and non-medical (Martínez et al., 2017; Jackson, Sleigh, Wang, & Liu, 2006). The literature shows that financial support from the family reduces the probability of abandoning the treatment, as well as the economic impact produced by out-of-pocket expenses for food, transportation, or medical costs (Castro Galarza et al., 2020), as well as the time that patients and their families stop receiving income due to the inability to work caused by the disease, its care and its risks (Kemp, Mann, Simwaka, Salaniponi & Squire, 2007).
4.2. Liabilities
Liabilities correspond to material and immaterial barriers to the use of certain resources, and their existence prevents or limits the use of opportunities or the accumulation of assets (Kaztman and Filgueira, 1999). The accumulation of liabilities or a greater weight with respect to assets has negative effects on adherence to treatment, and on the overcoming of biological, psychological, social, or economic adverse effects, affecting the success of treatment.
In this study, the mean age of the participants was 50 years, with a higher proportion of men, while the report ofTuberculosis Colombia 2017 (INS, 2017) coincides with sex but differs with the mean age since the population more affected was older than 65 years old. In likeness to the WHO (WHO, 2020) and to (André et al.. 2020), the results in relation to age presume a labor affectation due to the productive age in which they are. In addition, it may have greater physical involvement as a result of the pathophysiological changes and the deterioration of the immune protection that occur in older people. Consequently, recovery may be slower and have greater side effects from the medications (Salgueiro, 2002).
Ethnicity and gender can operate as a liability. In more than 50% of surveyed respondents, a predominance of Afro-Colombian and indigenous ethnic groups was identified, mainly women. This fact can indirectly show inequalities and structural vulnerabilities of gender and ethnicity expressed in disadvantages. Studies show exclusion conditions in access to education, decent employment, access to credit, and cultural and recreational services, among others, which increase for women (Salgueiro, 2002).
On the other hand, although it was found that social networks are assets, the absence of those negatively affects the management of the disease in daily life to fulfill economic needs, have emotional support or carry out daily activities (Castro Galarza et al.. 2020).The number of cohabitants, marital status, and the number of dependents brings us closer to recognizing this situation, which constitutes a liability due to the possibility of increasing the vulnerability of those affectedcby TB.
Likewise, perceptions and experiences of discrimination increase vulnerability due to their effects on mental health. Self-confinement, isolation, and the fear of being recognized as infected, as a result of the stigma of the disease, reduce the possibilities of interaction, coinciding with what Ugarte-Gil (2009) calls "social death" because it closes the possibility of integrating into society.
In this study, more women than men reported a decrease in the number of cohabitants during and after treatment. In addition, singleness was predominant in almost 52% of affected women. Being single at a mean age of 50 can represents loneliness, and although low dependency would be expected, very few of the surveyed population worked during and after treatment. Some women receive less family support, as Romero (2004) shows, who found that women were rejected by their husbands, and did not receive social, moral, or economic support from their relatives, leading them to abandon treatment. If living alone is added to all of the above, this group of situations suggests an important relationship between the lack of family support networks and socioeconomic deprivations, increasing social vulnerability.
In the socioeconomic dimension, two situations that can potentially become liabilities are identified: the first, belonging to low and very low socioeconomic strata, and the second, having a subsidized health regime since it includes the poorest population without the ability to pay. Most of them do not have their own home or motor vehicles, they do not have access to revolving bank loans, nor do they have technological goods or connectivity. This significantly affects access to communication and information about tuberculosis and its treatment (Tenelema, Alvarez & García-Pena, 2018) and reduces the chance of people with TB and their families to deal with the economic costs resulting from adverse health conditions, as well as the costs and economic effects directly related to TB and its treatment.
In families with these characteristics, which also earn their income through informal jobs, the family vulnerability increases given the inability to work caused by the disease, the time required to fulfill the treatment, and, in some cases, the transportation costs. Ugarte-Gil (2009) shares these findings, mentioning that tuberculosis is strongly related to poverty with characteristics such as overcrowding in homes, difficulties with transportation, and the need to work, resulting in abandonment or irregular treatment. Poverty is presented as a factor for abandoning treatment and with the increase in multidrug resistance.
The condition of social vulnerability is reflected in people with TB who do not have formal jobs and experience layoffs while they have the disease, which significantly affects their family and personal economy, and their mental health. There is also evidence that they need to go out to work despite their illness and frustration due to the lack of income to support themselves financially during treatment. Additionally, very few manage to obtain State economic subsidies despite their condition of poverty.
People affected by TB, given their prevailing condition of poverty, should have access, beyond health insurance subsidies, to other social protection strategies recommended for populations with greater social vulnerability, such as food baskets, conditioned economic subsidies, and others that facilitate access to healthcare, education for work, public housing programs and other complementary welfare services (Hargreaves et al.. 2011 ; Sann, 2011;WHO, 2012). For their part, those who have access to formal employment but live in conditions of poverty should receive an expansion of social protection services, at least during the illness.
Concerning education, more than a third of those affected by TB have significant educational backwardness and the vast majority are between no studies and up to secondary school. This situation constitutes an important liability for them. It has a proven relationship as a factor that increases the risk of suffering from the disease and abandoning treatment since it determines the occupational position, the type of employment relationship, generally in the informal sector, the level and frequency of income, and access to benefits of working protection. In this regard, Lozano et al. (2009) mention that tuberculosis predominates in strata with low education, which usually determines employment, housing conditions, and access to utilities and personal care. |
Various studies have shown the relationship between the dimensions of social vulnerability and the incidence of TB, especially in human capital, work and income, not only in the general population but also in the most vulnerable groups (Lapsin et al.. 2020), as well as the relationships between housing conditions, tobacco consumption, economic and sociodemographic factors, and well-being conditions (Trivianita, Marsisno, and Wilantika, 2019).
Being a structural and permanent situation also increases the vulnerability of affected people, the same factors are still present and are even exacerbated during the disease, and remain after it, causing little adherence to treatment or abandonment of this, consequently, relapses, worsening of the health condition and even death.
Regarding health, the results confirm what other studies have found. TB itself constitutes a major health impact on the people who suffer from it, due to its disabling power and the side effects of treatment. Additionally, due to its consequences on mental health derived from stigma, discrimination, fear, isolation, and permanent stress, even more so when people cannot access job opportunities to satisfy basic needs, as a result of physical disability as well as discriminatory practices. Additionally, the presence of comorbidities is added. Among the co-morbidities, some of them such as HIV bring an additional burden that enhances the negative impact on various spheres of life of patients and their families.
Finally, in the environmental dimension, the perception of insecurity constitutes a liability for affected people since it can generate barriers to using different resources, for example, to trust in the treatment, as it affects free mobility, reduces social interaction, and causes stress which affects the quality of life of people.
4.3. Structure of opportunities
Concerning the structure of opportunities, three fundamental areas generate support for the protection, attention, and care of people with TB, by generating resources or enabling the use of those available, these are the State, the civil society, and the market. In the first group, the provision of basic health services was identified, which is available from the Political Constitution of Colombia and is evident in the health coverage of 95% of the participants. This reflects a positive element in the structure of opportunities since other studies have shown an increase in the probability of TB infection in populations without the availability of said services (Cardoso et al., 2017).
On the other hand, the low availability of the Internet in the population, both during treatment and currently, allows reflecting on the digital divide that becomes even more relevant at present given the changes in educational and work practices that are supported more and more in the use of the Internet. This tool constitutes a means of production and flow of information related to the health of great importance for people with the disease and their carers (Tenelema et al., 2018), and therefore, the lack of connectivity represents a weakness in the structure of opportunities to face the disease. On the other hand, the Integral Social Security System incorporates a model in which social assistance is especially relevant in vulnerable populations; for that reason, it is important the finding that 20% of affected people currently receive State economic support and, of greater concern, that only 10% received it during treatment. This reveals a weakness in the structure of opportunities to face the various circumstances since economic support has shown to be useful in cases that are difficult to manage, improving adherence to treatment (Chirico et al.. 2018).
Meanwhile, through the General System of Social Security in Health, health insurance is guaranteed to around 95% of the participants, belonging to the contributory and subsidized regime. This system covers health contingencies for the most vulnerable, the possibility of family coverage for both health regimes, which generates relevant support for the use of health services that contribute to dealing with the disease.
Both the conditional transfer programs and the health insurance models that generate support alternatives for people affected by tuberculosis constitute fundamental elements to comply with the second pillar of the END TB Strategy, in the component of social protection, relief of poverty, and actions on other determinants of TB. With this, it intends to generate a structure that facilitates the compensation and financing of the economic burden associated with the disease and supports to deal other circumstances such as interruption of studies, loss of employment, or divorce that may occur as a result of the disease (WHO, 2015).
The institutional existence of a TB program for the identification, treatment, and follow-up of people with TB is part of the support emphasized by the participants, from the health professionals belonging to the program, the availability of information, and the accompaniment to face the disease.
The elements described above are consistent with what was stated by Cabrera-Pablo, Pría-Barros, Perdomo-Victoria and Ramis-Andalia (2018) about the basic elements of the availability of health services for the population with tuberculosis, including the perception of society and people with a TB diagnosis on the quantity and distribution of said services, the geographical location, the time services take to reach the institutions, the infrastructure, technologies, and human resource capacities. Likewise, acceptability, which is related to lifestyles and the link established by the user with the provider.
Regarding the labor market, it is clear that contemporary changes in the world of work reflect a reality that embodies job insecurity and flexibility (Castel, 2004 Sennett, 2006). In the Colombian case, this situation is also reflected in working informality according to the measurement carried out by the National Administrative Department of Statistics -DANE, informality was 47.4% for the first moving quarter of 2021. In addition, unemployment for the month of April 2021 reached a rate of 15.1%. This context denotes a weak structure of opportunities given the impossibility of the labor market to absorb the labor force, a situation that can increase when the subjects have a health condition such as tuberculosis.
In this study, although it was not possible to trace in detail if the precarious working conditions lead to the origin of the disease, it was possible to identify some related variables, such as belonging to the health subsidized regime that could be associated with working informality, unemployment, low income, and even low educational levels. In addition, it was found that having tuberculosis affects the chance of continuing with working life, but also due to social insecurity denoting informal employment relations that do not guarantee employment permanence and that, on occasions, ignorance and stigmatization related to the disease generates layoffs, affecting the living conditions and well-being of patients and their families. This finding is related to the study by Needham, Bowman, Foster and Godfrey-Faussett (2004), in which they found that people with tuberculosis lose working hours, which can result in decreased wages or dismissals and represent a significant reduction in family incomes.
5. Conclusions
The results show a vicious circle between social vulnerability conditions and tuberculosis since people with the highest levels of social vulnerability are those who experience life situations that predispose the development of the disease, as well as they are the most affected in all dimensions of their existence by the disease, increasing or maintaining their levels of vulnerability. This shows the dialectical nature of the biological, psychological, economic, and social dimensions in the production of the disease and, consequently, the need to articulate TB programs based on clinical and pharmacological support, other psychosocial and socioeconomic strategies that must be implemented in vulnerable populations to prevent/ eradicate TB, as well as for its treatment.
The liabilities, assets, and structure of opportunities must be seen as chains rather than independent variables, whose relationships and interactions must be analyzed in specific contexts to carry out interventions relevant to each reality. In this study, two axes of production or reduction of social vulnerability linked to TB treatment are identified. On the one hand, the labor market and social protection networks guarantee permanent jobs and decent income that affect direct and indirect out-of-pocket expenses linked to treatment, as well as the personal and family economic impacts resulting from suffering from and receiving TB treatment, even more so when there are comorbidities. On the other hand, family, community, and institutional support networks offer support for the care of people with TB and its comorbidities, allowing them to face the fact of suffering from TB and their treatment, additionally offering them financial support when required.
Social vulnerability offers a multidimensional interpretive framework to manage TB at the population level as well as to increase the comprehensiveness of care for people who suffer from it. Applied to large population groups, this framework makes it possible to identify groups that experience differential conditions of deprivation, fragility, and social disadvantage on which it is necessary to implement general programs and other specific ones that improve living conditions in general and attend specific needs and reduce or eradicate TB or other diseases associated with high levels of social vulnerability, exclusion, and poverty. At the same time, it offers evidence on key dimensions on which to intervene to increase the effectiveness of TB programs. That is to say, at both levels of intervention the participation and articulation of multiple sectors are required as from actions exclusively focused on the provision of health services it is impossible to achieve the required comprehensiveness.
It is recommended to articulate the TB programs of the healthcare institutions with other care mechanisms for vulnerable populations, such as community kitchens, foster homes, and listening stations. Likewise, focus the actions to capture respiratory symptoms, sample taking, and follow-up to treatment in spaces and populations that experience situations of social vulnerability, such as the population deprived of freedom, homeless people, and homes in which people live in conditions of overcrowding such as tenements houses and irregular settlements where migrants, displaced populations or homeless people live