Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Universitas Medica
Print version ISSN 0041-9095On-line version ISSN 2011-0839
Univ. Med. vol.59 no.1 Bogotá Jan./Mar. 2018
https://doi.org/10.11144/javeriana.umed59-1.refr
Artículos originales
Characterization of Refractive Errors in a Population of Children from 2 to 14 Years of Age in Bogotá, Colombia
1Estudiante de tercer semestre de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia
2Profesor asistente de la Facultad de Medicina, Pontificia Universidad Javeriana
3Estudiante de quinto semestre de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia
Introduction:
Refractive errors can have important repercussions in the performance of an individual, especially in the pediatric community.
Objective:
To determine the prevalence of refractive errors within a sample of 112 children between the ages of 2 and 14 from the Colegio La Candelaria in the city of Bogotá.
Methods:
Cross-sectional study that evaluated through visual acuity, ocular motility, ophthalmoscopy, retinoscopy, and subjective exam, the visual capacity of the children in question.
Results:
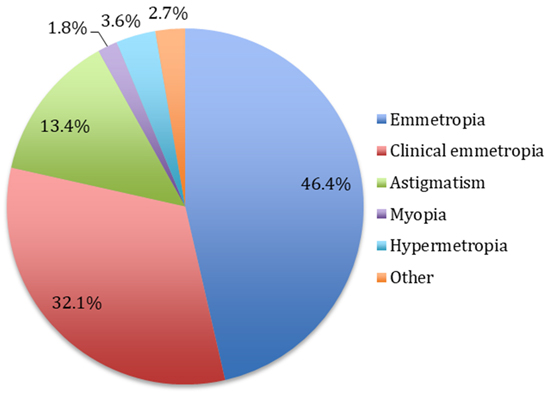
We found a prevalence of refractive errors of 18.8% where 13.4% represented astigmatism, 3.6% hypermetropia and 1.8% myopia.
Discussion:
These results were compared with those exposed on a thesis performed in 1973 by which patients with similar conditions were tested. In this study, the refractive errors were of 30.48%, a difference that can be explained by variations in population characteristics. Lastly, it arises the need of screening in other communities.
Keywords astigmatism; hypermetropia; myopia; prevalence; children
Introducción:
Los defectos refractivos pueden repercutir de manera importante en el rendimiento de un individuo, sobre todo en la población pediátrica.
Objetivo:
Determinar la prevalencia de defectos refractivos en una muestra de 112 niños entre los 2 y los 14 años del Colegio La Candelaria, en la ciudad de Bogotá.
Métodos:
Estudio de corte transversal que valoró, por medio de la agudeza visual, motilidad ocular, oftalmoscopia, retinoscopia y examen subjetivo, la capacidad visual de los niños en cuestión.
Resultados:
Se encontró una prevalencia de defectos refractivos del 18,8 %, dentro de la cual el 13,4 % representaba astigmatismo; el 3,6 %, hipermetropía, y el 1,8 %, miopía.
Discusión:
Se compararon los resultados con aquellos de una tesis realizada en 1973, donde se estudiaron pacientes en condiciones similares. En esta, la prevalencia de defectos refractivos fue del 30,48 %, diferencia que se podría explicar por la variación de características poblacionales. Por último, se plantea la necesidad de tamizaje en otras comunidades.
Palabras clave astigmatismo; hipermetropía; miopía; prevalencia; niños
Introduction
The eye is an essential organ for our relationship with the environment. It is responsible for capturing light stimuli and converting them into electrical impulses that are transported to the brain to provide information on aspects such as size, shape, color and texture of objects around us, in addition to the distance at which they are located. Also, it is a complex component of the human body, in terms of structure and function that can be affected by a large number of problems.
These problems include refractive errors, which are “very common eye disorders, in which the eye cannot clearly focus the images” on the retina (1). These defects can have an important impact on the visual sphere of an individual and, therefore, on the deterioration of his/her productivity, regardless of the stage of life in which the person is (2). In view of this, and given the fact that “of the 100 million visually impaired people in the world, four out of five have a cause that can be treated to restore their vision,” being the refractive errors the most common cause, it is important to prevent the consequences of not managing these type of errors (3). Thus, the term prevention is understood as measures designed to mitigate the consequences of a disease once it has been established (4).
Among the most common refractive errors are myopia, hypermetropia and astigmatism. Myopia is an error in which light rays that come parallel from infinity focus before the retina when the accommodation is at rest (5). In hypermetropia, the light rays that come parallel from infinity focus behind the retina when the accommodation is at rest and, depending on the degree of the defect and other characteristics, it can produce blurred vision of close objects (6) Finally, in astigmatism, light rays that come parallel from infinity focus on more than one point of the retina when the accommodation is at rest.
On the other hand, we must take into account other terms, such as emmetropia and clinical emmetropia, since they are the other variables in which people are classified when generating an assessment of visual capacity. An emmetropic eye is one that achieves a visual acuity of 20/20 without an associated refractive error, and a clinically emmetropic eye is one that, despite having a refractive error, has a visual acuity of 20/20 and the error is categorized as physiological. This occurs because “it is normal that children at birth have a certain degree of hypermetropia and that in the first years the power of the eye changes to achieve emmetropia. This process is known as emmetropization” (7).
One of the groups that has been affected the most by these problems is the pediatric population, due to the fact that various pathologies and defects often develop since childhood, altering visual acuity and therefore), disrupting therefore the learning process and the cognitive development of children 1 (8,9). For this reason, it is important to mention that, according to the Ministry of Social Protection, in 2001, and the National Survey of Risk Factors for Chronic Diseases 1998, 50% of the child population had refractive errors in Colombia. Additionally, in 2007, the World Health Organization attributed 18-20% of refractive errors to myopia, 5% to hypermetropia and the rest to astigmatism (3).
Taking into consideration the above, it is very useful to establish the prevalence of refractive errors in a sample of the Colombian pediatric population, with the purpose of performing preventive measures through an early diagnosis and a subsequent timely treatment. In order to achieve this goal, a team was formed with volunteers from the Angie Báquiro student group and doctors from the Hospital Universitario San Ignacio.
Angie Báquiro is a non-profit group conformed by young people from the Pontificia Universidad Javeriana. One of its programs is “Lessons for Life” and its objective is to promote personal care and the adoption of healthy habits to improve the quality of life of boys and girls from the city of Bogotá. Since 2014 through the COCOS project, “Lessons for Life” focuses on the population group between 2 and 14 years of age, of socioeconomic strata 1 and 2 at La Candelaria Educational Institution.
Therefore, this population was selected in order to determine the refractive status and visual capacity of the children included within the sample and to determine the prevalence of refractive and visual alterations, in order to compare this population with others throughout history and establish approximations regarding the causes of the differences observed. In addition, the purpose of this study is to propose the necessary solutions required to improve the performance, learning and integral development of affected children in this and other communities.
Methods
This cross-sectional, observational-descriptive research study 2 was carried out by means of an ophthalmology brigade carried out on June 4th, 2016 (10). This event attended a sample of children that was obtained by an open call through which the students of the educational institution interested in the campaign could sign up. The inclusion criteria were: being within the age range of 2 to 14 years, that their families were informed by the La Candelaria Educational Institution about the brigade, having signed up for it and being present the day it was carried out.
An ophthalmologist, an ophthalmologist-optometrist, an ophthalmology resident and fourteen undergraduate students of medicine from the Lessons for Life Group participated, which allowed the methodology of the campaign to be satisfactorily carried out. They effectuated the procedures to assess the condition of the children, by means of:
Anamnesis. A questionnaire was conducted using a system of specific and direct questions about the personal and sociodemographic data of children, their health background, emphasizing on their ophthalmological and optometric history, and information about other systems.
Physical exam. The height and weight of the children were measured and an external examination of the eye was performed by means of a detailed visualization, looking for any abnormality that could cause a decrease in the visual acuity or a loss of it.
Visual acuity without correction. Through an examination the patient’s visual capacity was measured, first evaluating the right eye, then the left eye and, finally, using both at the same time, without optical correction (glasses or contact lenses) (11). It was measured at six meters with Snellen optotypes. It is the visual acuity with which the patient arrives.
Glasses in use. In case that the patient possessed glasses, the diopters of the latter were measured through lensometry. Posterior to this, how much did the visual acuity of the patient correct while wearing the lenses was measured.
Ocular motility:
Ductions: An examination of the muscles of a single eye (monocular movements): adduction, abduction, supraduction, infraduction, incycloduction, excycloduction (12).
Versions: An examination of the muscles of the two eyes (binocular movements in the same direction, conjugated gaze): supraversion, infraversion, dextroversion, levoversion (12).
Vergences: Binocular movements in opposite directions: convergence and divergence (12).
Cover test: Observation of the movements of one eye when covering the other for the identification of tropias (constant deviation of the eye) (12,13).
Ophthalmoscopy. Monocular test to determine the condition of the fundus, that is, visualized through the pupil, and the transparent media of the eyeball (cornea, aqueous humor, crystalline, and vitreous humor), the retina and the optic disk (14).
Retinoscopy. Objective exam to “measure the refractive power of the eye by interpreting the light reflected from its retina when illuminated with the retinoscope” (15).
Subjective examination. It is a subjective test that is performed based on the patient’s responses. By means of this the definitive correction is reached.
The data obtained from the physical examination was later used for the tabulation and subsequent general description of the population). The results were tabulated in Excel® and, were also used for the relevant calculations, such as the prevalences of each of the refractive errors in the study.
Results
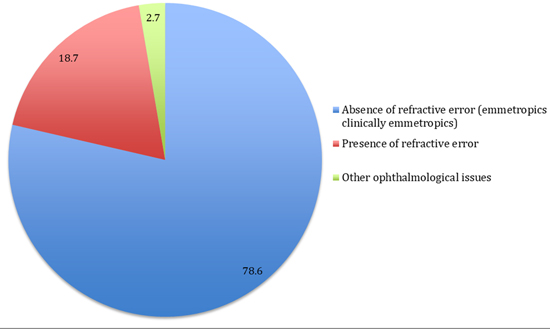
In the ophthalmology brigade, 112 patients between 2 and 14 years of age from the Colegio La Candelaria, from strata 1 and 2 were clinically assessed. Within the sample, a prevalence of refractive errors of 18.8% was found; a prevalence of healthy children in whom no clinically relevant refractive error was identified of 78.6%, and a prevalence of children with other ophthalmological problems not associated with refraction of 2.7% (Figure 1).
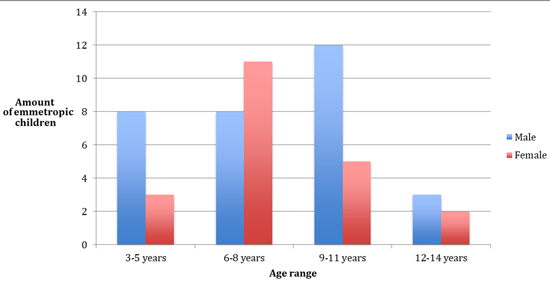
Analyzing the total population, it is important to mention that within the group of healthy children, 46.4% were classified as emmetropic, and 32.1% as clinically emmetropic (figures 2 and 3). Furthermore, the average age within these two groups was very similar, being 7.9 and 7.8, respectively. The classification of clinically emmetropic was more frequent in women (Figure 2).
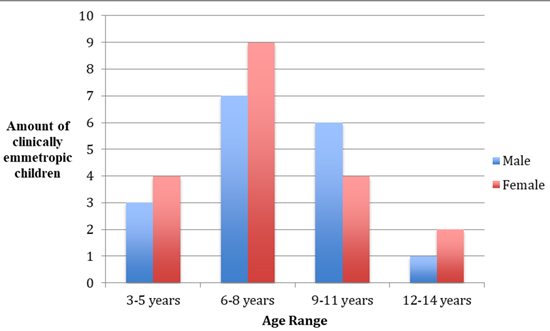
Figure 3 Distribution of clinically emmetropic patients according to gender and age (36 individuals)
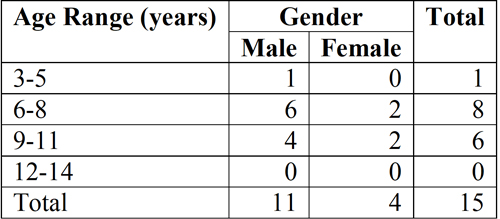
On the other hand, among the people with a refractive error, 13.4% were diagnosed with astigmatism; 3.6%, with hypermetropia, and 1.8%, with myopia (Figure 4). Within the group of those with astigmatism, the average age was 8 years and the proportion of men to women was 1.6:1, being a more common problem in men in the population studied (Table 1). It is important to mention that within the total population, 4 children presented hypermetropia, which were all male and were in the age range of 7 to 12 years. Also, there were 2 girls of 5 and 8 years diagnosed with myopia, and finally 3 children who were grouped within the category of “other ophthalmological diagnoses.”
Discussion
In order to analyze the results of this study, it was proposed to make a comparison with a senior thesis made by two optometrists from the Universidad de La Salle in 1973, which was later confirmed over time (in 1983, with a group of recycling people from Bogotá; in 1984, with a group from the Albergue de Chicalá; in 1985, in the Palermo Sur neighborhood; in 1986, in the city of Leticia, and in 1987 and 1988, in the Chocó Department) (16). This work, entitled Prevalence of Ametropia in School Age, was the first epidemiological profile of refractive errors in Colombia and it evaluated a population with characteristics very similar to ours, which is an important aspect for the comparison of both studies, added to the interesting factor of the difference in time and the changes that this could bring.
The senior thesis assessed the refractive status in a sample of 818 patients between 5 and 15 years of age that fluctuated between socioeconomic strata 1 and 2; individuals in schools with the same characteristics of the institution where our work was carried out.
In the study conducted at the Colegio La Candelaria, a total of 18.8% were found to be ametropic, which was lower, compared to the results of the aforementioned study, where this percentage was 30.48%. The above, considering ametropic individuals as those with a clinically relevant refractive error.
In our study we found that 9.57% of the ametropic individuals had myopia (1.8% of the total sample), while in the study conducted in 1973, the percentage of myopic patients was 50.13% (15.28% of the total sample). Also, it was observed that 19.15% of the ametropic population was hypermetropic (3.6% of the total sample), while in the study performed by the optometrists, the percentage of hypermetropic patients was 44.88% (13.68% of the total). Finally, we found that 71.28% of people with refractive errors in our sample had astigmatism, being the most prevalent refractive error (13.4% of the total sample), which is in line with other studies such as one completed in 2003 by Kleinstein (17), where astigmatism was the most prevalent refractive error in Hispanic patients; while in the study performed by the two optometrists only 4.99% of those affected (1.52% of the total sample) had this diagnosis, being the least prevalent refractive error. On the other hand, in the present study we found that 78.6% of the population was emmetropic; in the study conducted in 1973 this category was found in 35.45% of the sample.
An important aspect is the fact that after the senior thesis was published, other medical brigades were carried out in various populations, always maintaining the similar characteristics in question, and until 1988 very similar results were obtained. Thus, it is interesting to analyze the reason for the change that is currently observed.
The differences exposed can be the result of multiple factors. As one of the main ones, we suggest the increase in both coverage and access to health services in Colombia, as it is an essential factor, due to the difference in time between the two studies. By 2016, more than 90% of the population was affiliated to the health system (18) and, therefore, more periodic ophthalmological/optometric examinations are performed. This does not ensure that the children are given the glasses they need; but they are diagnosed to a large extent. In contrast, in the similar population of the study conducted in 1973 only 0.4% of the myopic patients, 2.4%, of the hypermetropic patients, and 0.73%, of patients with astigmatism, had previous ophthalmological examinations, which allows to infer the coverage status of that time and compare it with the current data. In addition, this shows a great difference that can have an impact on the results, since it is possible that some of the children of the Colegio La Candelaria already had a diagnosis of refractive error prior to the call and for this reason they decided not to participate in the campaign. If so, this could be one of the reasons why the percentages of refractive errors are lower in our study, when compared with the senior thesis, in which there were more children that had never been examined by an ophthalmologist or an optometrist.
On the other hand, there may be different risk factors between the samples and new characteristics inherent to the population, such as nutritional, behavioral, genetic, coverage and health care characteristics, which could have an impact on the results obtained. It is concluded, then, that in the current work there were fewer individuals with refractive errors; however, it is not possible with the present data to affirm that these have diminished in the population, since the population characteristics must have varied from 1973 to the current date. Moreover, it is important to take into account the difference in the samples’ size, since the size of the present study was of 112 children; while that of the senior thesis was 818, this being an important factor in terms of numerical results.
We also compared the results of the present study with others of an international nature. First, the information published in 2007 by the World Health Organization, which attributed 18-20% of the total refractive errors to myopia, 5% to hypermetropia, and 75% to astigmatism (3). That being the case, we obtained a result similar to that of this organization, in terms of astigmatic patients, being around 70% of the percentage of the sample. However, in our case there was a greater number of hypermetropic patients than myopic patients, whilst the results of the World Health Organization were the opposite. In the second place, we compared our results with an article published in 2012 about 1,852 individuals from Gondar, Ethiopia, between 4 and 24 years of age, in which 9.4% had a refractive error and within these, 31.6% were attributed to myopia, 26.4% to hypermetropia in the right eye, and 22.4% to hypermetropia in the left eye (19). This shows that in this population there were fewer refractive errors than in ours and that, as in the results of the World Health Organization, there was a greater prevalence of myopia than of hypermetropia. In 2004-2005, in Maharashtra, India, another similar study was carried out in which 5,021 children from the urban area and 7,401 children from the rural area were examined, and the prevalence of refractive errors was 5.46% and 2.63%, respectively. In the first case, the prevalence of myopia, hypermetropia and astigmatism was 3.16%, 1.06%, and 0.16%, respectively, and in the second, 1.45%, 0.39%, and 0.21%, which shows that their results were inverse to ours, since in our population astigmatism was the most common error, followed by hypermetropia and, finally, myopia (20). The same inverse results were observed in a study in Al-Hasa, Saudi Arabia (21). However, a research such as the one conducted in Dezful, Iran, obtained results similar to ours, since the most prevalent refractive error found was astigmatism (22). Bearing that in mind, we highlight the evident differences observed worldwide.
Finally, we consider it relevant to raise awareness in terms of the need to generate, for other communities, visual acuity screening by means of brigades such as the one carried out, evaluations of the satisfaction of families with respect to their visual health and education in terms of the importance of these periodic evaluations and the management of refractive errors.
Acknowledgements
We thank Dr. Tatiana Urrea and Dr. Álvaro José Mejía, ophthalmologists, for supporting us in the brigade, and Dr. Julio César Castellanos, director of the Hospital Universitario San Ignacio, for allowing us to carry it out. Funding Entity: Hospital Universitario San Ignacio.
REFERENCES
1. Organización Mundial de la Salud. ¿Qué son los errores de refracción? [Internet]. 2009 [Citado 2016 oct 16]. Disponible en: http://www.who.int/features/qa/45/es/ [ Links ]
2. García PE, Mariño SC, Giraldo OL. Caracterización de las condiciones visuales de niños con discapacidad cognitiva, Bogotá. Salud Areandina. 2013;2:44-57. [ Links ]
3. Quintero ML, Díaz ZR. Programa de salud visual en niños entre los 6 y 13 años del área rural del municipio de San Bernardo (Cundinamarca), soportes educativo, asistencial y epidemiológico. Bogotá: Universidad de La Salle; 2008. [ Links ]
4. Sanabria PA. Reflexiones alrededor del concepto de promoción de la salud y prevención de la enfermedad. Rev Fac Med [Internet]. 2011 [citado 2016 oct 16];19(1). Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-52562011000100013 [ Links ]
5. National Eye Institute. Información sobre la miopía [Internet]. 2012 [citado 2016 oct 16]. Disponible en: https://nei.nih.gov/health/espanol/miopia/miopia [ Links ]
6. Clínica Baviera. ¿Qué es la hipermetropía? [Internet]. [citado 2016 oct 16]. Disponible en http://www.clinicabaviera.com/refractiva-hipermetropia [ Links ]
7. Figueroa LF, Molina NP. Errores refractivos en niños de tres a siete años en la localidad de Chapinero en la ciudad de Bogotá. Cienc Tecnol Salud Vis Ocul. 2011;9 55-61. [ Links ]
8. Linares AR. Desarrollo cognitivo: las teorías de Piaget y de Vygotsky. Master en Paidopsiquiatría [Internet]. 2007-2008 [citado 2017 may 20]. Disponible en: http://www.paidopsiquiatria.cat/files/teorias_desarrollo_cognitivo_0.pdf [ Links ]
9. Hernandez CP, Barrera DC, Guiza C, Rodríguez JP, Ludeman WE, Gómez SP. Estudio de prevalencia en salud visual en una población escolar de Bogotá, Colombia, 2000. Bogotá: Instituto Nacional de Salud; 2000. [ Links ]
10. Geneva Foundation for Medical Education and Research. Estudios transversales. Educación Médica [Internet]. 2005 [citado 2017 may 20]. Disponible en: http://www.gfmer.ch/Educacion_medica_Es/Pdf/Estudios_transversales_2005.pdf [ Links ]
11. Martín R, Vecilla G. Agudeza visual. En: Manual de optometría [Internet]. [ citado 2017 may 20]. Disponible en: http://media.axon.es/pdf/80824.pdf [ Links ]
12. Muñoz FJ, Rebolleda G, Del Castillo JM. Práctivas IV: Motilidad ocular extrínseca. Instituto Alcon [Internet]. 2004 [citado 2017 may 20]. Disponible en: http://alexanderospino.com/wp-content/uploads/2013/03/Pract.IV_Motilid.ocul_.extrins._esp.pdf [ Links ]
13. Arroyo ME. Estrabismo [internet]. [citado 2017 may 20]. Disponible en: http://www.amc.org.mx/web2/images/media/enfermedad/2012/estrabismo.pdf [ Links ]
14. Preza L. Oftalmoscopía directav[internet]. Juárez: Universidad Juárez del Estado de Durango [citado 2017 may 20]. Disponible en: http://famen.ujed.mx/doc/manual-de-practicas/a-2016/04_Prac_04.pdf [ Links ]
15. Herranz RM. Retinoscopía [Internet]. [citado 2017 may 20]. Disponible en: http://www.sld.cu/galerias/pdf/sitios/optometria/retinoscopia.pdf [ Links ]
16. Camacho GE, Saavedra L. Prevalencia de las ametropías en la edad escolar. Universidad Social Católica de La Salle; 1973. [ Links ]
17. Kleinstein, R. Refractive error and ethnicity in children. Arch Ophtalmol. 2003;121:1141-7. [ Links ]
18. Agudelo CA, Cardona J, Ortega J, Robledo R. Sistema de salud en Colombia: 20 años de logros y problemas. Ciencia y Salud Colectiva. 2011;16:2817-28. [ Links ]
19. Yared AW, Belaynew WT, Destaye S, Ayanaw T, Zelalem E. Prevalence of refractive errors among school children in Gondar Town, Northwest Ethiopia. Middle East Afr J Ophthalmol [Internet]. 2012 [citado 2017 may 20];19(4):372-76. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519123/#ref6 [ Links ]
20. Padhye AS, Khandekar R, Dharmadhikari S, Dole K, Gogate P, Deshpande M. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol [Internet]. 2009 [citado 2017 may 20];16(2):69-74. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813593/ [ Links ]
21. Wadaani FAA, Amin TT, Ali A, Khan AR. Prevalence and pattern of refractive errors among primary school children in Al Hassa, Saudi Arabia. Glob J Health Sci [internet]. 2013 [citado 2017 may 20];5(1):125-34. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4776961/ [ Links ]
22. Norouzirad, R, Hashemi H, Yekta A, Nirouzad F, Ostadimoghaddam, H, Yazdani N, et al. The prevalence of refractive errors in 6- to 15-year-old schoolchildren in Dezful, Iran. J Curr Ophthalmol [internet]. 2015 [citado 2017 may 20];27(1-2):51-5. Disponible en: http://www.sciencedirect.com/science/article/pii/S2452232515000098 [ Links ]
Received: December 10, 2016; Accepted: August 25, 2017











 text in
text in