Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Universitas Medica
versão impressa ISSN 0041-9095versão On-line ISSN 2011-0839
Univ. Med. vol.59 no.1 Bogotá jan./mar. 2018
https://doi.org/10.11144/javeriana.umed59-1.letc
Artículos originales
Knowledge, Practices, Attitudes and Opinions of the Health Personnel of the Department of Pediatrics of a University Hospital in Colombia about the Limitation of Therapeutic Effort in Children
1Profesora asistente, Hospital Universitario San Ignacio-Departamento de Pediatría, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia
2Profesora asociada, Hospital Universitario San Ignacio-Departamento de Pediatría, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia
3Pontificia Universidad Javeriana, Bogotá, Colombia
4Médica residente tercer año de Pediatría, Pontificia Universidad Javeriana, Bogotá, Colombia
5Médica residente tercer año de Pediatría, Pontificia Universidad Javeriana, Bogotá, Colombia.
Introduction:
Concepts like Limitation of Therapeutic Effort (also known as End of Life Care [ELC]) are vital for daily practice.
Objective:
To identify the knowledge, practices, attitudes and opinions about ELC in a Pediatric service.
Results:
121 surveys (80% of the population) were evaluated. 96% of the people know the term ELC, 91.5% have been in contact with at least one case, but only 25% consider having received training in the subject during their training, in 86% of cases the decision to ELC was taken in a multidisciplinary meeting or in conjunction with the family.
Conclusions:
Respondents are familiar with the term ELC, very few were trained during their training. We consider it necessary to develop educational tools and support with regard to pediatric palliative care for health personnel in charge of pediatric patients.
Keywords palliative; knowledge; passive euthanasia; end of life care
Introducción:
Conceptos como limitación del esfuerzo terapéutico (LET) son de vital importancia para la práctica diaria.
Objetivo:
Identificar conocimientos, prácticas, actitudes y opiniones sobre LET en un servicio de pediatría. Método: Estudio observacional descriptivo de corte transversal. Encuesta estructurada.
Resultados:
Se evaluaron 121 encuestas (80 % de la población). El 96 % de las personas conocen el término LET, el 91,5 % ha estado en contacto con al menos un caso, pero solo el 25 % considera haber recibido capacitación en el tema durante su formación; en el 86 % de los casos la decisión de LET se tomó en junta multidisciplinaria o en conjunto con la familia.
Conclusiones:
Las personas encuestadas están familiarizadas con el término LET; son muy pocas las que recibieron capacitación durante su entrenamiento. Es necesario el desarrollo de herramientas educativas y apoyo respecto a cuidados paliativos pediátricos para el personal de salud a cargo de pacientes pediátricos.
Palabras clave paliativo; conocimiento; eutanasia pasiva
Introduction
In the model of care of the Pediatric Service of the Hospital Universitario San Ignacio (HUSI), an awareness-raising process has been developed since 2011 on issues related to palliative care and end-of-life dilemmas, such as the limitation of therapeutic effort (LTE), which has generated a process of reflection on the subject in the academic and health care community.
Worldwide, pediatric palliative care is relatively new (1,2,3), and it has increased in recent years, due to the fact that incurable catastrophic illnesses have increased (4). For this reason, in 2000 the Bioethics Committee of the American Academy of Pediatrics published guidelines for the implementation of palliative care in children (5).
Baseline studies have shown that one of the main limitations in the application of palliative care is the lack of education and training about this issue during medical training. Flórez et al. (6) showed that only 13% of pediatric residents and pediatricians have received training in palliative care, and 57.1% have received it through a partner, or through self-learning.
Although there is controversy regarding the term, LTE can be defined as the clinical decision of not initiating or stopping a therapy, treatment or diagnostic means to a patient in whom this does not modify in any way the behavior or the course of the condition, given the irrecoverable conditions of his/her illness and prognosis, and that, on the other hand, can cause him/her more damage or suffering; that is, when the therapeutic measures are considered extraordinary or disproportionate for the objective to be achieved in the particular context of that patient (7,8,9,10). The great confusion that exists between LTE, dysthanasia and orthotanasia, as well as the lack of knowledge of the extent to which it is ethical to limit treatment, what measures we can take and in which cases, leads us to critical, ethical and emotionally very complex situations that hinder decision making.
Several studies have been carried out worldwide to evaluate the importance of education on this topic, and a clear need to receive more training focused on palliative care during the training process has been demonstrated. The purpose of this article is to identify the knowledge, practices, attitudes and opinions on LTE of the health care and academic personnel of the pediatric service of a general university hospital in Bogotá, Colombia.
Materials and Methods
The literature on the subject was reviewed, and then the research group created a survey of 16 structured questions that included social, personal and cultural aspects that seem to influence the decision making on the part of the health personnel who manage patients with catastrophic illnesses.
In the period between July and September 2016, all the staff of the pediatric service were invited to participate, anonymously and voluntarily. In total 121 of 150 eligible people participated.
Data were collected and an independent statistical analysis was carried out using the statistical package R (11), which reports measures of central tendency for quantitative variables, and of frequencies for qualitative variables.
Results
80% of the people who were invited to participate answered the survey. Of 121 participants, 26 (21.5%) were pediatricians, 40 (33%) pediatrics residents, 18 (14.8%) registered nurses, and 37 (30.5%) nursing assistants. The average age of the personnel surveyed was 33 years, with a standard deviation of 7.4 years. Of this group, 84% professed some religion, the most frequent being Catholicism, followed by Protestantism, without encountering other religions. 16.5% declared that they do not practice any religion.
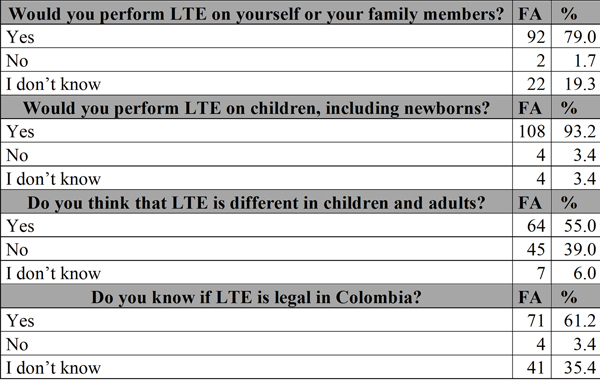
96.7% of people have heard the term LTE. The majority would perform LTE on themselves or their relatives, and consider that it is legal in Colombia and is different in children and adults (Table 1).
Of the 55% of people who considered that there are differences between children and adults, 22% considered that this was due to mental capacity, 26.5% to legal reasons, 58% to life expectancy, and less than 1% for other reasons.
Of the people who knew the term LTE, 91.5% had been in contact with at least one case in which said procedure was performed; in 79% of the cases the decision had been made by a medical team, in 1.9% the decision had been taken exclusively by the treating doctor, and in 1.7% it had been taken by the doctor and the family. Only in 0.9% of the cases the decision had been taken exclusively by the family. 96% of the people surveyed agreed with the decision made, while 4% disagreed.
Regarding the interventions that are part of LTE, the responses were varied: 96.5% of people considered that pain management is part of basic care, even in cases of LTE. Similarly, 98% believe that the dispensation of oxygen is part of this management. Overall, 80% do not think that LTE means stopping all medical intervention (Figure 1).
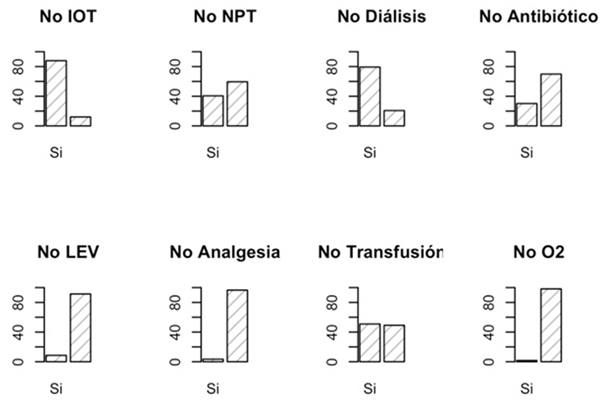
Figure 1 Interventions that are part of the limitation of therapeutic effortIOT: orotracheal intubation; TPN: total parenteral nutrition; LEV: intravenous fluids; O2: supplemental oxygen.
The majority of the respondents considered that the LTE issue is very important, they report having received little training, and all felt that LTE should be included in the training programs (Table 2).
Discussion and Conclusions
Like all human beings, children have the right to live with dignity and to die with the same dignity, since death is part of their lives. Hence, always, and even more in the imminence of death, there must be a broad and open dialogue between the health team, the patient and the parents of the child, so that decisions can be made in favor of the best interests of the minor (12,13).
Some of the factors that had initially been considered could influence end-of-life decision-making were not identified as barriers in this study; for example, religion, since the great majority of respondents professed some religion, which is in keeping with the studies on this subject (14).
The vast majority of the respondents consider the topic of end of life and LTE important; however, they believe that the training that they have received is limited and insufficient. It is therefore essential that in the future this training be included in the undergraduate and graduate programs in the area of health sciences (2,4,15). In Colombia there are few reports on the subject. In 2015, a 2011 report was published (6) that showed that graduate and trainee pediatricians have little knowledge about palliative care (13% of 359 respondents). In 2014, a senior thesis reported that in a children’s hospital in Bogotá, 64.8% of the 85 respondents considered hospital LTE to be important (16). This phenomenon is not unique to Colombia: according to general reports analyzed in the study by Chiu et al. (17), both graduate doctors and medical students consider that they received little training in palliative and end-of-life care.
On the other hand, different teaching methodologies have been studied, among which are: lectures on pain management, conferences with parents of children with chronic diseases or deceased, training seminars about how to give bad news (with a duration of two hours for first-year residents), quarterly case discussions with the ethics group and monthly information sessions for residents during their rotations in intensive care units and pediatric hematoncology (18).
Coverage in palliative and end-of-life care in Colombia is limited, particularly for children, as the number of trained personnel is limited and there are no pediatric palliative care training programs. In the same way, within the medical school curriculum there are no subjects about palliative care for adults or children. In a study conducted in 2014 in Colombia it was found that less than 5% of the undergraduate medicine and nursing programs include palliative care as a specific subject (19), which is in accordance with the situation of the region (20).
This is the first study about knowledge, practices, attitudes and opinions about LTE in the HUSI. Since 2011, there has been an awareness-raising process in this hospital—particularly in the Pediatric Service—and since 2016 the hospital has a pediatrician with formal training in pediatric palliative care.
Although there is a limitation regarding training in pediatric palliative and end-of-life care in children in Colombia, the Department of Pediatrics at HUSI has achieved an awareness about the subject of end-of-life; this has allowed health personnel to recognize that this subject is essential for their professional practice and to consider that it is necessary to increase their formal and non-formal training. The vast majority of the staff has been in contact with LTE cases and has agreed with the decisions taken. According to the data of this study, although there is a lack of knowledge on the subject, this is not a reason to consider LTE as taboo or inappropriate in children.
It will be necessary to evaluate if the members of other departments of the HUSI share the perceptions of the members of the Department of Pediatrics regarding LTE in children; we will also have to explore the attitudes and perceptions of the members of other pediatric departments in Colombian about end-of-life care in children.
Referencias
1. Bogetz JF, Ullrich CK, Berry JG. Pediatric hospital care for children with life-threatening illness and the role of palliative care. Pediatr Clin North Am. 2014;61(4):719-33. [ Links ]
2. Aulino F, Foley K. Professional education in end-of-life care: a US perspective. J R Soc Med. 2001;94(9):472-6; discussion 7-8. [ Links ]
3. Martínez Hernández EB. Panorama actual de los cuidados paliativos pediátricos [internet]. Tesis de diplomado. Asociación Méxicana de Eduación Continua y a Distancia, Guanajuato, México; 2013. Disponible en: http://www.tanatologia-amtac.com/2013. [ Links ]
4. Khaneja S, Milrod B. Educational needs among pediatricians regarding caring for terminally ill children. Arch Pediatr Adolesc Med. 1998;152(9):909-14. [ Links ]
5. American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000;106(2 Pt 1):351-7. [ Links ]
6. Flórez P, Tovar B, León M, Villegas K, Villamizar DdP, Granados CE. Knowledge of pediatric palliative care and perception of barriers by pediatricians and pediatric residents. Medipal. 2015;22(4):127-35. [ Links ]
7. Herreros B, Palacios G, Pacho E. [Limitation of the therapeutic effort]. Rev Clin Esp. 2012;212(3):134-40. [ Links ]
8. Ayestarán MA, Gea LB, Gordon AB, Arruabarrena EC, Otoño LE, Agirre AE, et al. Guía de práctica clínica sobre cuidados paliativos. En: Guías de práctica clínica en el SNS. Madrid: Agencia de Evaluación de Tecnologías Sanitarias del País Vasco; 2008. [ Links ]
9. Eijk WJ. Tratamiento proporcionado y desproporcionado, ensañamiento terapéutico y cuidado paliativo. Dolentium Hominum. 2005;58:79-85 [ Links ]
10. Asociación Médica Mundial. Declaración de Venecia de la Asociación Médica Mundial sobre la Enfermedad Terminal [internet]. 2006. Disponible en: https://www.wma.net/es/policies-post/declaracion-de-venecia-de-la-amm-sobre-la-enfermedad-terminal/ [ Links ]
11. R Development Core Team. R: A language and environment for statistical computing [Internet]. Vienna: R Foundation for Statistical Computing; 2011. Disponible en: http://www.R-project.org/. [ Links ]
12. Soler F, Pedrós F, Marín F, Ania MJ, Cambrón A, Alcázar JD, et al. Los derechos del niño. Revista DMD. 2012;11. [ Links ]
13. Brudney D, Lantos JD. Whose interests count? Pediatrics. 2014;134 Suppl 2:S78-80. [ Links ]
14. Delgado-Guay MO, Chisholm G, Williams J, Bruera E. The association between religiosity and resuscitation status preference among patients with advanced cancer. Palliat Support Care. 2015;13(5):1435-9. [ Links ]
15. Sullivan AM, Warren AG, Lakoma MD, Liaw KR, Hwang D, Block SD. End-of-life care in the curriculum: a national study of medical education deans. Acad Med. 2004;79(8):760-8. [ Links ]
16. González Cruz LR. Consideraciones sobre la limitación del esfuerzo terapéutico (LET) en pediatría [internet]. Bogotá: Universidad Nacional de Colombia; 2014. Disponible en: http://www.bdigital.unal.edu.co/12322/1/luisricardogonzalezcruz.2014.pdf [ Links ]
17. Chiu N, Cheon P, Lutz S, Lao N, Pulenzas N, Chiu L, et al. Inadequacy of palliative training in the medical school curriculum. J Cancer Educ. 2015;30(4):749-53. [ Links ]
18. Michelson KN, Ryan AD, Jovanovic B, Frader J. Pediatric residents' and fellows' perspectives on palliative care education. J Palliat Med. 2009;12(5):451-7. [ Links ]
19. Pastrana T, Wenk R, De Lima L. Consensus-based palliative care competencies for undergraduate nurses and physicians: A demonstrative process with Colombian universities. J Palliat Med. 2016;19(1):76-82. [ Links ]
20. Fortín Magaña M, Gómez Casanovas J, López Saca M. Situación actual de la enseñanza de la medicina paliativa en las universidades de Centroamérica. Educación Médica. 2016. doi: https://doi.org/10.1016/j.edumed.2016.08.00 [ Links ]
Received: March 28, 2017; Accepted: August 08, 2017











 texto em
texto em