Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Universitas Medica
Print version ISSN 0041-9095On-line version ISSN 2011-0839
Univ. Med. vol.61 no.1 Bogotá Jan./Mar. 2020
https://doi.org/10.11144/javeriana.umed61-1.nmar
Articles
Characterization of Pediatric Patients Diagnosed with Post-Infectious Bronchiolitis Obliterans 2600 Meters above Sea Level
1Médica pediatra, Hospital Universitario San Ignacio, Bogotá, Colombia
2Médica pediatra. Magíster en Epidemiología Clínica. Profesora de la Facultad de Medicina, Pontificia Universidad Javeriana-Hospital Universitario San Ignacio, Bogotá, Colombia
3Médica neumóloga pediatra. Profesora de la Facultad de Medicina, Pontificia Universidad Javeriana, Hospital Universitario San Ignacio, Bogotá, Colombia
4Médica pediatra. Magíster en Bioética. Profesora de la Facultad de Medicina, Pontificia Universidad Javeriana-Hospital Universitario San Ignacio, Bogotá, Colombia.
5Médica pediatra. Profesora de la Facultad de Medicina, Pontificia Universidad Javeriana-Hospital Universitario San Ignacio, Bogotá, Colombia.
6Médica pediatra, Pontificia Universidad Javeriana, Bogotá, Colombia.
7Médica pediatra, Pontificia Universidad Javeriana, Bogotá, Colombia.
Aim:
To characterize a group of pediatric patients diagnosed with post-infectious bronchiolitis obliterans (PIBO) at a university hospital in Bogotá.
Methods:
A total of 2,635 PIBO-compatible clinical histories were reviewed. Pre-defined inclusion and exclusion criteria were applied, and 19 cases were retrieved and used to develop an observational, descriptive, and retrospective study.
Results:
The mean age for developing acute lower respiratory tract infection (ALRTI) was 18 months. The average hospitalization was 14.5 days, 21.5 % of patients required attention at a pediatric intensive care unit (PICU), and mechanical ventilation was applied for 10 % of these cases. A total of 30 % of the patients had microbiological isolation, 10.5 % corresponded to a respiratory syncytial virus (RSV), and 5 % corresponded to a mixed isolation (adenovirus and RSV). All patients had chest high-resolution computed tomography (HRCT) scans, which revealed a mosaic pattern of attenuation in 89.4 % of all cases.
Conclusions:
The sample showed clinical and radiological characteristics similar to those described in other case series worldwide.
Keywords hypoxia; newborn; hypothermia; infant; diseases; perinatal mortality
Objetivo:
Caracterizar un grupo de pacientes pediátricos con diagnóstico de bronquiolitis obliterante postinfecciosa (BOPI) en un hospital universitario de Bogotá.
Métodos:
Se revisaron 2635 historias clínicas compatibles con BOPI, aplicando los criterios de inclusión y exclusión predefinidos. Así se obtuvieron 19 casos con los cuales se desarrolló un estudio observacional, descriptivo y retrospectivo.
Resultados:
La edad media de presentación de la infección respiratoria baja grave desencadenante fue de 18 meses, hospitalización promedio de 14,5 días, el 21,5 % requirió atención en la unidad de cuidado intensivo pediátrico, con ventilación mecánica en el 10 % de estos casos. El 30 % de los pacientes tuvo aislamiento microbiológico, el 10,5 % correspondió a virus sincitial respiratorio y aislamiento mixto en un 5 %. Todos los pacientes tuvieron tomografía de tórax a partir del cual se encontró un patrón en mosaico de atenuación en el 89,4 % de los casos.
Conclusiones:
La población de estudio fue semejante en cuanto a las características clínicas y radiológicas descritas en otras series de casos en el ámbito mundial.
Palabras clave bronquiolitis obliterante; pediatría; adenoviridae
Introduction
Post-infectious bronchiolitis obliterans (PIBO) is a rare respiratory condition in children that is responsible for small-airway obstruction. The first description of the histological characteristics of this entity was published by the German anatomopathologist Lange, in 1901. Since that time, new cases have been documented around the world, especially in children who have suffered an episode of severe lower respiratory tract infection (LRTI) at some point in their life, and who subsequently develop a small-airway alteration with chronic respiratory symptoms (1).
The Southern Cone countries, such as Brazil, Argentina and Chile, lead the number of international publications (the largest and only cohort described so far in Latin America was made in Buenos Aires, Argentina, with 58 cases followed for 17 years). Most of these publications agree that the diagnosis of PIBO is based on the correlation of characteristic clinical and radiological aspects found in chest high-resolution computed tomography (HRCT) (1,2,3,4).
In Colombia there is a growing interest in identifying patients with a picture consistent with the diagnosis of PIBO, since it is a poorly understood and underdiagnosed entity. For this reason, this research group designed and developed this descriptive study in a university hospital in Bogotá —a city located 2,600 meters above sea level (m.a.s.l.), latitude 04° 36′ 35″ N, altitude 74° 04′ 54″ W. In this study, a group of PIBO patients treated over a 5-year period was evaluated to identify the variables related to the disease and contrast them with the descriptions made in the literature.
Materials and methods
This was a retrospective study of patients diagnosed with PIBO, evaluated in the Pediatric Pulmonology outpatient clinic and in the Emergency Department and Pediatric Hospitalization service between 2010 and 2014, at the Hospital Universitario San Ignacio (HUSI), located in Bogotá, Colombia.
The project was developed by a group of pediatricians and pediatric pulmonologists, with the support of methodological advisors. An extensive review of the best available literature was also carried out, to define the state-of-the-art of the subject and prepare a preliminary inventory of the most outstanding variables related to the natural history of the disease. The inventory was evaluated by experts and, through a survey with external reviewers (seven Colombian pediatric pulmonologists were surveyed), the variables that would be important to identify in the present study were defined.
After obtaining authorization from the HUSI Bioethics and Research Committee, an advanced search tool was used (Disearch, a search and prioritization software for electronic medical records jointly developed by the Systems Engineering Department of the Pontificia Universidad Javeriana and the Hospital Universitario San Ignacio) sensitive enough to identify possible cases of PIBO in the electronic hospital care database. A search was made with this software between 2010 and 2014, using terms related to possible cases of PIBO in pediatric patients. Search criteria included the code of the International Classification of Diseases 10 for chronic obstructive pulmonary disease, an age range between 0 and 15 years, and keywords such as bronchiolitis obliterans, constrictive bronchiolitis and tomography pattern of mosaic attenuation (suggestive of small-airway alteration characteristic of this disease).
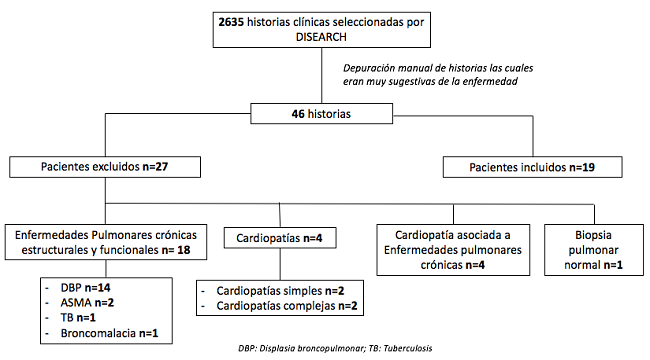
As a result of this initial computer search, 2,635 stories were obtained. These were manually reviewed by pediatric physicians to identify which patients met the diagnostic criteria for the disease. This manual review was done using a checklist that included, in general terms, verification of the medical record suggestive of severe or chronic respiratory disease consistent with the pathology of interest, work diagnoses during hospital events and differential diagnoses evaluated by the treating group, the concept of the Pediatric Pulmonology service, and the results of chest tomography images. Cases in which there was a reasonable doubt in any of these aspects, were carefully analyzed by at least two team members to define whether it was included in the group of short-listed medical records.
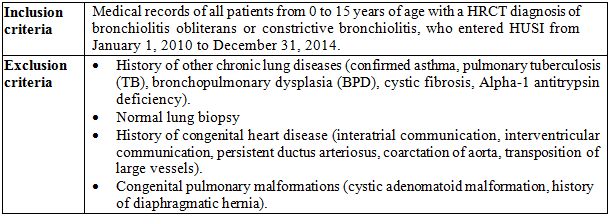
Through this process, 46 cases very suggestive of the disease were found. Two members of the group made a second exhaustive analysis of these medical records to determine if they met the inclusion criteria (Table 1). Cases in which there were doubts were discussed in investigator meetings to resolve the controversy by consensus. Through this process, 27 patients were ruled out, mostly due to a history of heart disease and other chronic lung diseases (Figure 1).
Finally, 19 cases were submitted to final analysis. For each of them, the specific information available in the Integrated Hospital Administration System was reviewed, evaluating the variables proposed by the research group. With this information, an Excel data extraction table was created that subsequently underwent a statistical analysis, using the Stata 13 software. In two cases with missing data, telephone communication was established with family members to supplement the information.
Results
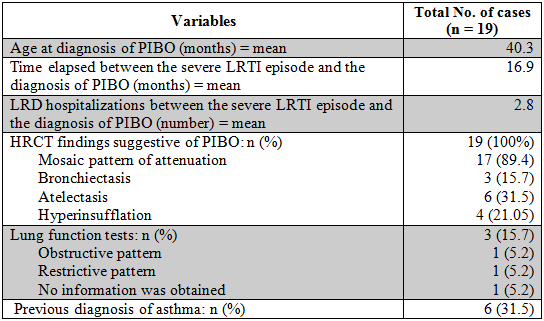
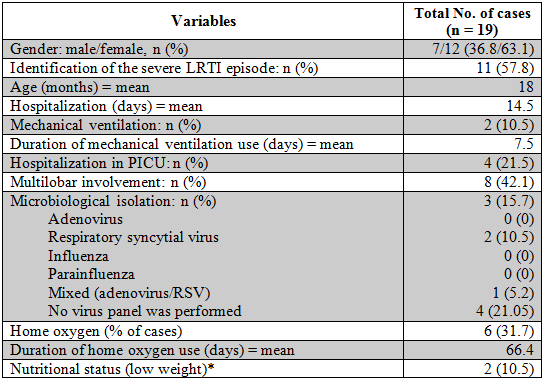
Nineteen medical records of patients who met the inclusion criteria were evaluated, who were treated at least once in the HUSI, in the Emergency Department and Pediatric Hospitalization service, or in follow-up in the Pediatric Pulmonology outpatient clinic (Tables 2 and 3).
Table 2 Variables analyzed during the severe LRTI episode (possible PIBO triggering event)
*Low weight determined by Z-Score less than 2 SD.
The majority of the children studied were females (63.1% vs. 32.8%). Only in a little more than half of the cases (57.8%) was it possible to identify a previous severe LRTI episode as a possible PIBO trigger. It was found that the average age of presentation of this infection was 18 months (interval between 2 and 79 months of age) and that the vast majority (90.9%) presented this episode before 24 months old. The hospital stay for this episode was 3 to 45 days, with an average of 14.5 days, and in 10% of the cases the hospitalization lasted more than 30 days.
The severity of the infection was defined based on three variables: multilobar involvement, hospital stay in a pediatric intensive care unit (PICU), and the requirement for invasive mechanical ventilation. The chest radiograph showed multilobar involvement in 42.1% of the patients; 21.5% of patients required admission to a PICU, and only 10.52% required mechanical ventilation, with an average of 7.5 days of ventilatory assistance.
Microbiological isolation was performed in 30% of patients. It was found that the predominant infection was caused by respiratory syncytial virus (RSV), in 10.5% of cases. Only adenovirus was found as mixed isolation (RSV and adenovirus) in 5% of cases. In 20% of patients, viral isolation techniques were not performed, and in 50% of cases there was no information in the medical record.
It was found that in the majority of patients in whom a severe LRTI was identified, home oxygen was required (31.7%) after the episode, with an average duration of 66.4 days, and the vast majority (80%) used it for more than a month.
Once the PIBO diagnosis was made, the average age at diagnosis was 40.3 months (interval between 4 and 162 months of age), and an average of almost 17 months elapsed between the possible severe LRTI triggering event and the PIBO diagnosis. We also found that in this last period between the triggering infectious episode and the PIBO diagnosis there was an average of 3 hospitalizations for acute respiratory disease. In 31.5% of cases there was a previous diagnosis of asthma.
The most common finding in the chest HRCT was mosaic pattern of attenuation (89.4%), which suggests small airway damage, followed by atelectasis (31.5%) and air trapping (21%). The least frequent finding was bronchiectasis, with 15.7%.
In most cases, lung function tests were not performed (84.5%). In the three cases in which they were performed, no response to the short-acting inhaled β2-agonist was obtained; in addition, a predominant pattern of involvement was not found (33.3% obstructive, 33.3% restrictive, and in 33.3% no information was obtained).
Finally, information was obtained from the medical records on the nutritional status in half of the patients at the time of the severe LRTI. It was found that 22% of them were underweight, and the remaining 80% had an adequate nutritional status.
Discussion
This study is the first publication in Colombia aiming to describe a series of PIBO patients treated in a five-year period at a university hospital in Bogotá. Until the time of writing this article, no other similar publications were known in our country. In Latin America, this entity has only been documented in a series of 58 cases followed for 17 years in a hospital in Buenos Aires (5). There are few reports from other countries, including a series of 31 cases followed for 10 years in Korea and the United States (6), as well as series conducted in Malaysia (7) and China (8) with 14 and 42 cases, respectively.
PIBO is a clinical entity with low global prevalence and probably also in our environment, given that its description has been relatively recent (1,2,3.8). Therefore, its diagnostic approach requires a strong suspicion based on a suggestive medical history and tomographic evidence of characteristic changes of small airway involvement (1,2,3,9).
This research group identified 46 cases of pediatric patients treated in the Hospitalization, Outpatient and Emergency Services, with clinical and radiological criteria highly suggestive of this entity. However, this article described 19 cases that adequately met the selection criteria (most of the excluded cases were related to previous respiratory and cardiac comorbidities). The following discussion is oriented towards two main aspects: first, the characterization of variables related to the probably triggering severe LRTI and, second, the variables related to the subsequent diagnosis of PIBO.
The literature mentions that an episode of severe LRTI during the first 3 years of life has been identified as a possible triggering event (1,2,3,5,7,8,9,10,12). In this cohort, the presentation of the severe LRTI was between 2 and 79 months of age, with an average of 18 months. For this episode, the average hospital stay was shorter than that described in the literature (5,8). It is noteworthy that 10% of our patients needed hospitalization longer than 30 days, a fact that Murtagh et al. (12) report as a risk factor to develop PIBO, with an odd ratio of 27.2 (95% CI: 14.6–50.9). Regarding the severity of the triggering respiratory infection, it was found as risk factors (2) that 20% of patients required management in PICU and 50% of these cases needed an average of 7.5 days of invasive mechanical ventilation.
According to the literature, the infectious agent most frequently associated with the development of PIBO is adenovirus (1,2,6,9,13). Our study found that only 26.2% of patients with severe LRTI had microbiological isolation in respiratory secretion, for whom 10.5% were positive for RSV. Adenovirus isolation was only given in 5.2% of the cases, and was detected together with a case of positive RSV. A limitation of this study was that in 52.7% of the patients no information was found in the medical record regarding a request for microbiological isolation; this could be explained because in the clinical practice guidelines for attention and low respiratory infection and bronchiolitis (14,15,16) it is not considered mandatory to perform it, and for some time it was only processed in reference institutions for epidemiological surveillance.
With respect to the use of supplemental oxygen after the severe LRTI, a document published by the Chilean Society of Pediatric Pulmonology (17) suggests that essential clinical elements are required for the diagnosis of PIBO, such as: persistence of respiratory symptoms, obstructive or mixed symptoms, or hypoxemia between 4 and 6 weeks after the acute event. Therefore, it was relevant that in our cohort 31.5% of patients required prolonged use of oxygen therapy (greater than one month). This fact becomes more important, since this study was carried out in a hospital located at 2600 m.a.s.l., where there is a lower atmospheric pressure and, therefore, greater hypoxemia.
In a Spanish cohort of 22 cases, published by Sardón et al. (10), 63.6% of patients diagnosed with PIBO had at least one hospital admission after an episode of severe LRTI. In our study, patients had an average of 2.8 hospital admissions for exacerbations prior to the confirmation of the PIBO diagnosis. This variable suggests a chronic respiratory condition that should guide the clinician to sharpen his assessment of differential diagnoses. An Argentine publication (2) said that frequent hospitalizations are part of the natural course of the disease, but that both relapses and supplemental oxygen requirements decrease progressively with age.
The latency time between the severe low respiratory infection and the diagnosis of PIBO was 16.9 months. Such a delay is possibly related to the diversity and severity of the presentations of PIBO, and highlights the need to learn more about this entity.
PIBO is a recently described entity that in its initial stages has a clinical presentation similar to that of asthma, as described in other case series (10,17). In our cohort, 31.5% of the patients had a previous diagnosis of this bronchial pathology. This situation may favor the delay in the diagnostic suspicion of PIBO, which can cause confusion in the initial approach of these patients.
The research group evaluated the nutritional status of the children at the time of the severe LRTI episode. Information was obtained from half of the patients; only 22% of them were underweight, and the remaining 78% had an adequate nutritional status. Therefore, it seems unlikely that the nutritional status is a risk factor for developing a low respiratory episode that triggers PIBO, although other studies are required to define this causal relationship.
In this study, all patients had a chest HRCT, which is essential in the diagnostic suspicion of PIBO. The main imaging results were consistent with those described in other publications (2,10,17). 89.5% of our patients presented a mosaic pattern of attenuation in the computed tomography, a finding very suggestive of small airway damage.
Taking into account the age group of our series, a limitation was the technical difficulties for performing lung function tests. For that reason, they were not performed in the majority of cases (84.2%). Only 15% of cases had a spirometry. Although a predominant pattern of involvement was not found, it was found that in no case there was a response to the bronchodilator. This is related to what is described in the literature, which shows a predominance of a severe obstruction pattern with a low response rate to the use of inhaled β2-agonists (5,6,10). In our study we do not have specific data on lung volume or capacity to compare them with the literature that mentions findings consistent with hyperinsufflation and air trapping (4).
Another diagnostic method is lung biopsy, which is indicated only in selected cases, especially when there is a significant diagnostic doubt that other evaluation methods have not clarified (17). However, this procedure is performed rarely due to its invasive nature and the high probability of false negatives due to the heterogeneous pulmonary involvement; only in 30% of cases does the result agree with the clinical and radiological suspicion of PIBO (12). In our study we found a patient with clinical and radiological criteria very suggestive of the disease; for this reason, a lung biopsy was performed, with a normal result (for this reason he was not included in the group for final analysis). The research group considered that although this report did not rule out the diagnosis, he was excluded due to the methodological rigor of the non-inclusion criteria.
Conclusions
The majority of clinical and radiological characteristics of our PIBO patients in a city located at 2600 m.a.s.l. are similar to those described in other case series published in the literature. We expect to have medium-term follow-up data of the population described to assess the disease behavior and the associated lung function variables.
PIBO is a relatively unknown entity with a low prevalence that constitutes a challenge for the clinician. To the extent that clinical suspicion and timely diagnosis can be optimized, the management and follow-up of each case will be facilitated in order to favorably impact the individual prognosis.
It is necessary to develop multicenter research lines in our country that allow following-up a greater number of patients in the medium and long term, which will allow to evaluate in larger samples the main demographic characteristics and the possible predictive variables for the development of this entity and its prognosis.
Referencias
1. Colom AJ, Teper AM. Bronquiolitis obliterante postinfecciosa. Arch Argent Pediatr. 2009;107(2):160-7. [ Links ]
2. Colom AJ, Teper AM, Vollmer WM, Diette GB. Risk factors for the development of bronchiolitis obliterans in children with bronchiolitis. Thorax. 2006;61(6):503-6. [ Links ]
3. Fischer GB, Sarria EE, Matiello R, Mocelin HT, Castro-Rodríguez JA. Post infectious bronchiolitis obliterans in children. Paediatr Respir Rev. 2010;11:233-9. [ Links ]
4. Moonnumakal SP, Fan LL. Bronchiolitis obliterans in children. Curr Opin Pediatr. 2008;20:272-8. [ Links ]
5. Aguerre V, Castaños C, González Peña H, Grenovile M, Murtagh P. Postinfectious bronchiolitis obliterans in children: clinical and pulmonary function findings. Pediatr Pulmonol. 2010;45:1180-5. [ Links ]
6. Kim CK, Kim SW, Kim JS, Koh YY, Cohen AH, Deterding RR, White CW. Bronchiolitis obliterans in the 1990s in Korea and the United States. Chest. 2001;120(4):1101-6. [ Links ]
7. Chan PWK, Muridan R, Debruyne JA. Bronchiolitis obliterans in children: Clinical profile and diagnosis. Respirology. 2000;5:369-75. [ Links ]
8. Li YN, Liu L, Quiao HM, Cheng H, Cheng HJ. Post-infectious bronchiolitis obliterans in children: a review of 42 cases. BMC Pediatrics. 2014;14:238. [ Links ]
9. Colom AJ, Teper AM. Clinical prediction rule to diagnose post-infectious bronchiolitis obliterans in children. Pediatr Pulmonoly. 2009;44:1065-9. [ Links ]
10. Sardón O, Pérez-Yarza EG, Aldasoro A, Corcuera P, Mintegui J, Korta J. Bronquiolitis obliterante. Evolución a medio plazo. An Pediatr (Barc). 2012;76(2):58-64. [ Links ]
11. Champs NS, Lasmar LM, Camargos PA, Marguet C, Fischer GB, Mocelin HT. Post-infectious bronchiolitis obliterans in children. J Pediatr (Rio J). 2011;87(3):187-98. [ Links ]
12. Murtagh P, Giubergia V, Viale D, Bauer G, González H. Lower respiratory infections by adenovirus in children. Clinical features and risk factors for bronchiolitis obliterans and mortality. Pediatric Pulmonol. 2009;44:450-6. [ Links ]
13. Oymak FS, Demirbas HM, Mavili E, Akgun H, Gulmez I, Demir R, Ozesmi. M. Bronchiolitis obliterans Organizing Pneumonia. Respiration. 2005;72:254-62. [ Links ]
14. Colombia. Ministerio de Salud y Protección Social, Universidad de Antioquia. Guía de padres y cuidadores para la evaluación del riesgo y manejo inicial de la neumonía en niños y niñas menores de 5 años y bronquiolitis en niños y niñas menores de 2 años [internet]. Medellín: Universidad de Antioquia; 2014. Disponible en: https://medicosgeneralescolombianos.com/images/Guias_2014/GPC_42_Neumonia_y_Bronquilitis.pdf [ Links ]
15. Ralston SL, Lierthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134:e1474-1502. [ Links ]
16. Friedman JN, Rieder MJ, Walton JM. Bronchiolitis: Recommendations for diagnosis, monitoring and management of children one to 224 months of age. Paediatr Child Health. 2014;19:485-91. [ Links ]
17. Vega-Briceño L, Zenteno D; Comisión Multidisciplinaria para el Estudio de la Bronquiolitis Obliterante, Sociedad Chilena de Neumología Pediátrica, Sociedad Chilena de Enfermedades Respiratorias. Guía clínica para el diagnóstico y cuidado de niños/adolescentes con bronquiolitis obliterante post-infecciosa, 2009. Rev Chil Enf Respir. 2009;25:141-63. [ Links ]
Received: June 10, 2019; Accepted: July 30, 2019











 text in
text in