Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Universitas Medica
versão impressa ISSN 0041-9095versão On-line ISSN 2011-0839
Univ. Med. vol.61 no.4 Bogotá out./dez. 2020 Epub 30-Set-2020
https://doi.org/10.11144/javeriana.umed61-4.mmcm
Original
Manual for Classification of Congenital Upper Limb Malformations in the Fetus or Newborn based on Cadaveric Study
1Estudiante del pre grado en Medicina, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia.
2Profesor asistente del Departamento de Morfología, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia.
3Profesor asistente del Departamento de Morfología, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia.
4Profesora asistente del Departamento de Morfología, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá, Colombia. Investigadora del Instituto de Genética Humana, Facultad de Medicina, Pontificia Universidad Javeriana.
Introduction:
Congenital anomalies of the upper limb in the fetus or newborn include a wide spectrum of clinical presentations based on the penetrance and association between different anomalies. Therefore, their understanding and classification represents a real challenge for health professionals. The importance in understanding upper limb embryonic development events and the formation of its anatomical structures prevails on the fact that it helps to fully understand the classification of congenital limb malformations. Generally, these malformations represent a potential functional loss in the newborn that when timely recognized can be submitted to surgical treatment, obtaining both aesthetic as well as functional satisfactory results.
Methods:
Fetal necropsies including autopsy data with their respective photographic documentation were performed from different Health centers in Bogotá, Colombia from 2012 to May 2019, which led to a review of the literature in this regard, clarifying the diagnostic criteria for congenital abnormalities of the upper limb including only review articles and case reports that facilitate their understanding, definition and classification.
Results:
Seven upper limb malformations are presented, with the elaboration of a manual to guide health professionals regarding diagnosis, timely recognition of congenital upper limb malformations in the fetus and newborn. The manual aims to strengthen malformation recognition for a timely interdisciplinary evaluation.
Discussion:
Congenital upper limb malformations comprise a challenge for health professionals, their understanding must be approached from the phenomena of embryonic limb development to understand, identify anatomical structures and diagnose in a timely manner.
Keywords congenital abnormalities; upper limb; embryonic development; anatomical structures; Swanson modified classification
Introducción:
Las malformaciones congénitas de miembro superior en fetos o en recién nacidos comprenden un amplio espectro de presentaciones clínicas según la penetrancia y asociación entre distintas malformaciones. Entender los eventos en el desarrollo embrionario y la formación de estructuras anatómicas permite evaluar de forma integral la clasificación de las malformaciones congénitas que representan una potencial pérdida funcional, porque al ser reconocidas oportunamente, pueden someterse a tratamiento quirúrgico, para obtener resultados satisfactorios tanto estéticos como funcionales.
Métodos:
La práctica de necropsias fetales con su respectiva documentación fotográfica, más datos de necropsias hechas en distintos centros de salud en Bogotá desde 2012 hasta mayo de 2019, motivó una revisión de la literatura al respecto, a fin de esclarecer los criterios diagnósticos vigentes para las malformaciones de miembro superior. Se incluyeron solamente artículos de revisión y reportes de caso que facilitaran su entendimiento, así como su definición y clasificación.
Resultados:
Se presentan siete casos, con el reconocimiento oportuno de malformaciones congénitas del miembro superior en feto o recién nacido. Para ello se construyó un manual que pretende orientar a profesionales de la salud respecto a su diagnóstico. Lo anterior, con el ánimo de fortalecer la familiarización con dichas malformaciones que derive a una evaluación interdisciplinaria oportuna.
Discusión:
Las malformaciones congénitas de miembro superior comprenden un reto para los profesionales de la salud, y su entendimiento debe abordarse desde los fenómenos del desarrollo embrionario de las extremidades para comprender e identificar las estructuras y diagnosticarlas oportunamente.
Palabras clave anomalías congénitas; extremidad superior; desarrollo embrionario; estructuras anatómicas; clasificación de Swanson modificada
Introduction
Congenital upper limb malformations consist of a spectrum of abnormalities with varying degrees of functional limitation. In many of them it is possible to perform surgery and rehabilitation when they are recognized and corrected in a timely manner. The exploration of major and minor malformations of the upper limb is a challenge for the health professional who performs the newborn’s adaptation and complete physical examination, and also for the person who must thoroughly describe these findings in the fetal necropsy report. In this paper we describe seven cases of congenital upper limb malformations, and in the discussion we present, in the form of a manual (Manual for Classification of Congenital Upper Limb Malformations in the Fetus or Newborn), a compendium of the current diagnostic criteria of upper limb malformations for the health professional who seeks to recognize these malformations in the newborn or in fetuses subjected to necropsies.
In order to understand the classification and spectrum of congenital upper limb malformations, their anatomy and main functions must be taken into account. After describing the anatomical structures, we present the main events in embryonic development associated with the formation of the skeletal elements that allow the normal configuration of the anatomical structures of the upper limb. We describe the epidemiology of upper limb malformations, and in the discussion we present their classification, in the form of a manual.
Anatomy of the upper limb (appendicular skeleton)
The appendicular skeleton is formed by the bones and joints. There all the soft tissues are organized around them to form the upper limb (1). The skeleton of the upper limb consists of two segments: the pectoral girdle, located proximally, made up by the clavicle and the scapula, which are responsible for joining the upper limb to the pectoral region, mainly through muscles, rather than through ligaments (2). And the distal portion of the upper limb, made up of the humerus, radius and ulna bones and the carpal and hand bones (3, 4, 5) (Figure 1 D)
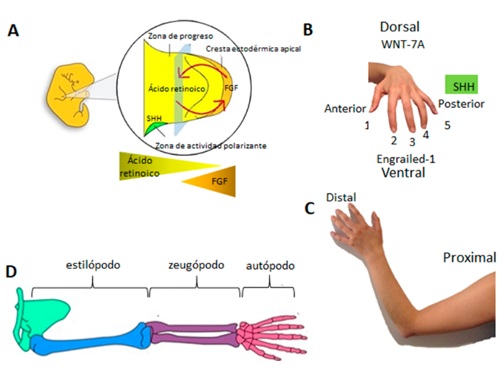
(A) Embryo at the end of the fourth week of development, which illustrates the formation of the four buds, two of upper limbs and two lower limbs, respectively. An enlargement of the bud is shown on the right, which highlights the areas of the apical ectoderm crest in the distal axis, where the fibroblast growth factor (FGF) is found in greater concentration (orange triangle and margin) and the progress zone (underlying mesoderm, yellow triangle illustrate their greater concentration towards proximal) differentiating the proximal axis. (B) The anterior-posterior and dorsal-ventral axes are shown with the main molecules for their determination: Sonic hedgehog (SHH) on the fifth digit that defines the posterior axis; its absence determines the anterior axis. On the dorsal axis, WNT-7A, which establishes its location, and Engrailed-1 (EN-1), the ventral structures. (C) Illustration of the proximal and distal axis and the five digits located in the distal axis. (D) Presentation of the four portions of the upper and lower limbs from their embryonic origin; they correspond from proximal to distal to the stylopod (humerus and femur), zeugopod (forearm or leg structures), followed by the mesopod (carpus or tarsus, respectively) and autopod (metacarpus, metatarsus and phalanges).
Likewise, the upper limb is divided topographically into regions called the shoulder, the arm, the forearm, the carpus and the hand, where each of the upper limbs is made up of 32 bones (2,4,5). From proximal to distal, the arm is made up of the humerus, and distal to the arm, the forearm houses the ulna and radius. In the most distal region of the upper limb is the hand, which includes the wrist with eight carpal bones, the palm (five metacarpal bones) and the fourteen phalanges of the fingers (2).
The appendicular skeleton provides support and insertion to the muscles and tendons responsible for limb movement (1). The movements carried out by the upper limbs are very extensive, thanks to the synovial joints that join the different bones: flexion, generated mainly by muscles located in the anterior zone of the limb, extension, generated by the muscles of the posterior zone, pronosupination, which is specific and exclusive of the region of the forearm, and the most important: grip and clamp, made by the thumb in the region of the hand (3).
Finally, irrigation and innervation are sectorized from proximal to distal from the subclavian artery, coming from the aortic arch and the brachial plexus nerves, giving rise to the radial nerve, with motor information for the posterior area of the upper limb; the muscular-cutaneous nerve, in charge of the muscular action for the anterior face of the arm; the median nerve, for the innervation of most of the muscles of the anterior region of the forearm and the thenar region of the hand, and the ulnar nerve, mainly for the innervation of the hypothenar and palmar region of the hand (3, 4, 5).
Embryonic development of the upper limb in humans
Due to the nature of this paper, we only describe the development of the skeletal component of the upper limb. The embryogenesis of the upper limb begins towards the end of the fourth gestation week with the formation of a bud or sprout. These buds are formed by a series of reciprocal inductions between mesoderm and ectoderm, highly controlled by the expression of transcription factors and paracrine factors in time and space (6,7). Limb buds correspond to the proliferation of the mesenchyme, derived from the lateral plate of the mesoderm, which will originate some cartilaginous molds, which later ossify and give rise to the skeletal tissue at the height of the C5 cervical vertebrae and up to the T2 thoracic vertebrae. This proliferation is regulated by a close interaction with the superjacent ectoderm, called the apical ectodermal crest, which gives rise to the structures in three spatial axes: proximal/distal, dorsal/ventral, anterior/posterior. Once the skeletal component is formed, from the somitic mesoderm, flanking each side of the neural tube, will give rise to the soft tissues of the limb (8).
The upper limb bud grows temporarily, from proximal to distal, and generates cartilaginous molds in four different portions (Figure 1) consisting of the stylopod, which will give rise to the structures of the humerus and the arm in the upper limb; followed by the zeugopod, which comprises the structures that will give rise to the radius, the ulna, the associated structures of the forearm; the zeugopod zone is followed by the mesopod, which will give rise to the carpal structures, and the autopod zone, which will finally give rise to the hand or foot structures, and will be the most distal musculoskeletal structure (8,9).
Once the cartilaginous tissue blastemas are formed, the endochondral ossification will take place (Figure 2), which is typical of the appendicular skeleton (8).
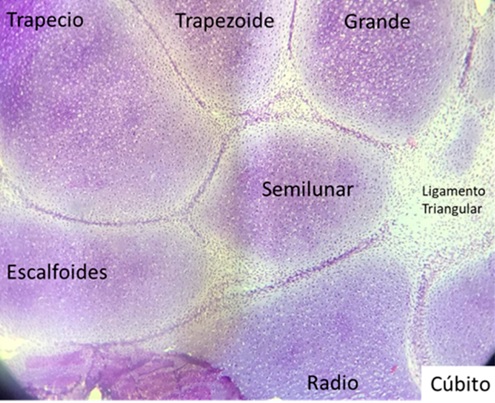
Figure 2. Bones of the forearm and palm with its five metacarpal bonesNote: Upper limb of a 15-week fetus, illustrated with cartilaginous molds that will differentiate into bone tissue to give rise to the formation of the palm bones through endochondral ossification, typical of the appendicular skeleton. The distal radio-ulnar and radio-carpal joints can be observed, as well as the joint between the first and second carpal row.
The upper limb develops itself in three spatial axes that differentiate in the following sequential order (Figure 1):
Proximal-distal axis: from opposite concentrations between retinoic acid in the proximal axis and the fibroblast growth factor (FGF), produced in the apical ectoderm crest. This interaction allows growth and projection of the limb in the proximal to distal direction (10, 11).
Anterior-posterior axis: from the signaling in the mesoderm located at the back of the bud. This region is known as the zone of polarizing activity, since it determines the polarity of the palette that will form the hand thanks to high concentrations of SHH. In this region the ulnar structures should be located. The suppression of signaling allows the development of radial structures. On the other hand, the expression of multiple HOX genes is also involved in the anteroposterior axis; in the case of the thumb in the upper limb, it is important to emphasize that its location in the hand is only achieved in the absence of SHH expression (10).
Ventral-dorsal axis: difference between the dorsal and ventral structures of the limb from the ventral signaling by Engrailed-1 expression, as well as the differentiation of the dorsal structures by WNT7A expression (10).
During embryonic life, the fingers are joined together by mesenchymal tissue membranes that form a palette in the most distal portion of the limb. However, the palette must be sculpted by mesenchymal tissue apoptosis in the interdigital space, thanks to the interaction between fibroblast growth factors, transcription factor Msx2 and bone morphogenic protein type 4 (BMP4) pathway (8).
Epidemiology
Congenital upper limb malformations are a common entity. It is estimated to occur in about 2.3 out of every 1000 live births (12). The prevalence of congenital upper limb malformations in the United States ranges between 0.16% and 0.18%. However, it is clear that it varies with a regional and ethnic correlation. Studies carried out in Finland, Canada and Australia report that the incidence of upper limb abnormalities ranges between 3.4 and 5.3 per 10,000 live births (13).
In Colombia, Zarante et al. (14) analyzed congenital malformations in 52,744 births in the cities of Manizales, Ubaté and Bogotá between 2001 and 2008. Their findings showed that upper limb malformations were the third most prevalent, among which polydactyly had an incidence of 21.2 per 10,000 live births. In general, this malformation was described more frequently in male patients (14). It should be noted that it is compatible with life, does not tend to get worse and improves significantly in terms of secondary disability with early medical intervention, which highlights the importance of recognizing it early.
However, the association between congenital upper limb malformations and potentially lethal syndromes should not be underestimated. Mortality among live-born patients with upper limb malformations has been documented to range between 14% and 16% in the first year of life; therefore, a comprehensive evaluation of these patients is required, as well as a complete examination of organs in the setting of a fetal necropsy (13). Other authors state that up to 18% of these patients have died by 6 years of age as a result of the syndromic association of the upper limb malformation (12). It is estimated that between 5% and 20% of patients with upper limb malformations have some syndrome that must be comprehensively evaluated by a multidisciplinary group of health professionals, in order to provide timely management (12).
Within the spectrum of congenital upper limb malformations, the most reported include failure of differentiation, followed by failure of duplication and formation abnormalities (12). In general, it has been identified that there is a higher prevalence of congenital upper limb malformations in men than in women, with a ratio of 3:2, respectively (12). Up to 50% of the patients have bilateral malformations, and in 17% of them multiple upper limb malformations are identified (12).
Methods
Performance and documentation of fetal necropsies
The photographic and histological documentation of congenital upper limb malformations used for this paper was taken from fetal necropsies performed by the authors in Bogotá, Colombia, from November 2012 to March 2019. All were carried out within the framework of Colombian legislation and had the informed consent of the parents or guardians. Photographic images and histological samples protect the identity of fetuses, relatives or guardians.
Search and selection of reports in the literature
Based on the clinical cases, the following keywords were searched in the PubMed, SciELO and LILACS databases: upper limb congenital malformation, upper limb failure of formation, upper limb failure of differentiation, syndactyly, phocomelia, club hand, upper limb duplication, polydactyly, upper limb overgrowth, upper limb undergrowth, constriction ring syndrome, Swanson upper limb congenital malformation classification. To describe the diagnosis and differential diagnosis, only review articles and case reports with an emphasis on diagnostic criteria were included, in Spanish and English, without date restrictions.
Results
Seven cases of fetal necropsies performed in Bogotá, Colombia, from 2012 to 2019 are described and presented below.
Congenital longitudinal failure of formation of the upper limb
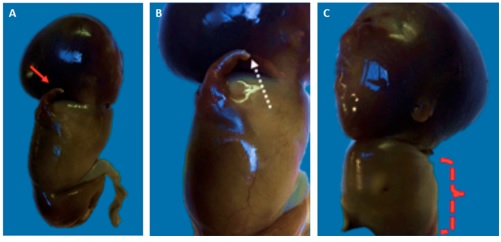
The case corresponds to a fetus of approximately 10 weeks of gestation with malformation of both upper limbs (Figure 3). It was classified as a type I bilateral upper limb malformation with failure of longitudinal formation. The right upper limb presents formation of the arm (stylopod) with deficiency of longitudinal formation. The zeugopod (forearm) is not present. On the contrary, presence of distal structures of the upper limb can be observed in the autopod, including appendages that rule out transverse deficiency of formation of the upper limb. For the left upper limb there is evidence of the presence of arm, forearm and parts attached to the hand with longitudinal growth deficiency of the limb.
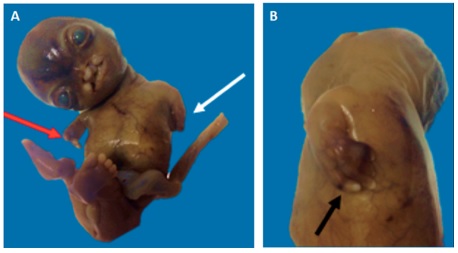
Figure 3. Fetus with type I bilateral upper limb malformation with failure of longitudinal formation
(A) The red arrow indicates the right upper limb with failure of longitudinal formation. Note the presence of distal structures of the upper limb, including appendages, which rules out transverse deficiency of formation of the upper limb. The white arrow points to the upper left limb with longitudinal growth deficiency. (B) Detail of the left upper limb showing the presence of hand appendages (black arrow) with longitudinal growth deficiency of the limb.
Phocomelia
The case corresponds to a 9-week fetus with malformation due to longitudinal growth deficiency of the right upper limb (Figure 4A). There is a unilateral phocomelia with only one hand structure, so it is a case of true right phocomelia (Figure 4B). Phocomelia is a congenital anomalous condition, in which the proximal component of the upper limb (humerus, radius and ulna) is absent or markedly hypoplastic with the presence of a hand component. Phocomelia refers to the similarity of the upper limb to the fin of a seal (15). Additionally, the complete absence of the left upper limb is recorded, so it is classified as a true amelia of the upper left limb (Figure 4C).
Necropsy of a nine-week fetus (A) Side view of fetus with malformation due to longitudinal growth deficiency of the right upper limb (red arrow). Clear example of a true unilateral phocomelia. (B) Detail of the right upper limb with presence of skin appendages given by an incipient nail bed (white dotted arrow). (C) Left side view showing true amelia.
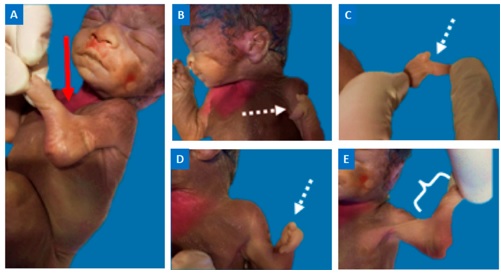
Radial club hand
The case corresponds to a 25 week gestation fetus with radial longitudinal deficiency in association with lobster claw hand. The fetus has upper left limb malformation with significant hypoplasia at the radial border, indicated by a red arrow (Figure 5A). The back (Figure 5B) and the palm of the upper left limb can be seen with only two digits (Figure 5C). On the radial end, a digit, which corresponds to the hypoplastic thumb (Figure 5D); additionally, another digit with ulnar deviation, which corresponds to a hand with lobster claw morphology. The hypoplasia of the radial edge of the upper left limb is shown in Figure 5E.
25-week gestation fetus with radial longitudinal deficiency in association with lobster claw hand. (A) Hypoplasia at the radial border indicated with a red arrow. (B) Back of the hand with lobster claw morphology. (C) Palm with two digits. (D) Hypoplastic thumb on the radial end; additionally, another digit with ulnar deviation. (E) Hypoplasia of the radial edge of the upper left limb.
Clinodactyly
Clinodactyly in a 38-week fetus. This malformation consists of a deviation of a finger in the coronal plane. It generally occurs due to an abnormal delta morphology of the middle phalanx of the fifth finger, which causes a deviation of more than 10 degrees of the distal interphalangeal joint (Figure 6).
38-week fetus with Down syndrome. (A) A middle phalanx of the fifth finger with wedge morphology is observed (red arrow). (B) Representation of a coronal view of a normal phalanx. (C) Representation of a coronal view of a wedge-shaped phalanx.
Polydactyly
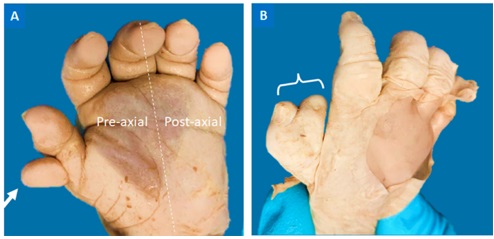
The case corresponds to an anomaly in a 38-week fetus, characterized by the existence of extra digits in the hands. In the palmar view of the upper left limb of the fetus, a supernumerary pre-axial digit is observed (Figure 7A). Additionally, in the upper right limb there is thumb duplication associated with syndactyly of the supernumerary digit (Figure 7B). Therefore, this fetus has bilateral pre-axial polydactyly associated with right upper limb syndactyly between the supernumerary finger and the thumb.
(A) Supernumerary pre-axial digit (white arrow) of the upper left limb in palmar view. (B) Thumb duplication associated with syndactyly of the supernumerary digit (white bracket) of the upper right limb of the same fetus.
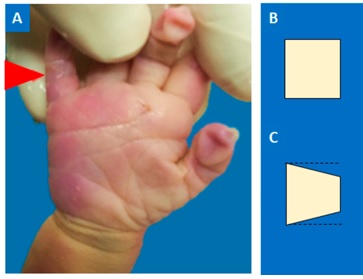
Brachydactyly
The case corresponds to a 40-week fetus with disproportionately short fingers. There is a difference between the length of the palm indicated with the white bracket and the region of the digits, indicated with the red bracket (Figure 8).
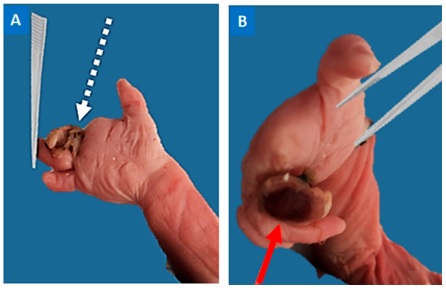
Acrosyndactyly or pseudosyndactyly
This case corresponds to a 35-week fetus that, due to amniotic bands, suffered constriction of the second digit of the right hand, for which it presented an ischemic process.
(A) Vestiges of the constriction bands (white dotted arrow). Distal to these is the ischemic digit. (B) Detail of the dorsal region of the second digit. Ischemic process (red arrow) in the affected digit, distal to the constriction bands.
Discussion
The understanding of the latest classifications and of upper limb congenital malformations are based on the processes in embryonic life that allow the development of the normal limb. Therefore, it is important for the clinician to understand the processes of embryonic development that form the upper limbs, to identify the affected anatomical structures, located in different regions and areas in the limb, in order to diagnose them in a timely manner.
The classification of congenital upper limb malformations was developed by Swanson in 1964. This classification was endorsed and approved by the American Association of Hand Surgery and the International Federation of Hand Surgery Societies. However, the international surgical community only accepted it until 1976, and it remains in force until today (12,16). Currently, the Swanson classification modified by the International Federation of Hand Surgery Societies (IFSHH) is used.
The Swanson modified classification (Table 1) is useful for understanding congenital upper limb malformations. However, it may be difficult to use it in the clinical setting, because some malformations are recognized in different categories.
Table 1 Swanson Classification
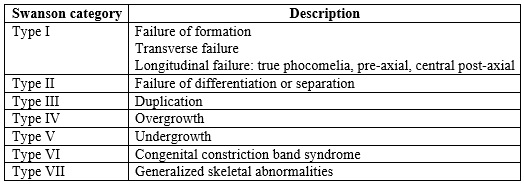
NoteClassification of congenital upper limb malformations developed by Swanson in 1964. It was later endorsed and approved by the American Association of Hand Surgery, as well as by the International Federation of Hand Surgery Societies. Finally, it was accepted by the international surgical community in 1976 (16).
For this reason, some authors have proposed other classifications, arguing that Swanson modified classification does not provide guidance on the etiology of the malformation. One of the proposed alternatives is the Oberg, Manske and Tonkin (OMT) classification, published in 2010. However, the international hand surgery associations have not approved this classification, so the Swanson modified classification remains in force and is accepted worldwide (17). The Swanson modified classification groups patterns of congenital upper limb abnormalities. However, it must be taken into account that each newborn or fetus with an upper limb malformation will have a total or partial involution, duplication or variable alteration of osteoarticular, muscle-tendinous and soft tissue in varying degrees, according to the penetrance of the malformation. Likewise, the anatomical structures associated with the malformation may vary in the same individual with bilateral involvement (16).
The Swanson modified classification considers all tissues of the upper limb. In addition, it should be noted that malformations affecting bone tissue are called major malformations (16). On the other hand, malformations that affect soft tissues in isolation are considered minor upper limb malformations. Based on this, congenital upper limb malformations are divided into seven groups distributed in failure of formation, which includes malformations by transverse and longitudinal failure, failure of differentiation or separation, duplication, overgrowth, undergrowth, amniotic band constriction syndrome and generalized skeletal abnormalities (12,16). Due to this, the authors of this paper propose the following classification manual for the differential diagnosis of upper limb malformations.
Manual for classification and differential diagnosis of congenital upper limb malformations
This classification categorizes the clinically predominant malformation in the patient into one of Swanson’s seven categories. Each limb of the patient should be addressed separately; although some congenital upper limb malformations tend to be bilateral, in some patients the diagnosis may differ in each limb (16,18).
Upper limb malformations due to failure of formation: type I
Upper limb malformations can be caused by a transverse interruption or a longitudinal interruption in limb formation.
Congenital transverse failure of formation of the upper limb
Transverse deficiency of formation of the upper limb, also known in the literature as peromelia (19), comprises a truncated upper limb without development of distal structures in that area. It is estimated that it constitutes up to 6% of congenital upper limb malformations, with an estimated incidence of 1 case per 20,000 live births (19, 20, 21). Generally, it does not have an associated inheritance pattern and is not associated with other malformations (19).
The most common clinical presentation is generated by transverse amputation in the forearm, and in some patients it is generated bilaterally (12). When the transverse congenital amputation is generated in the carpus, metacarpus or phalanges, a truncated upper limb is observed with complete absence of the hand. This is described in semiology as acheiria; in cases where one or more fingers are missing, it is described as adactyly (12).
It must be differentiated from the amniotic band constriction syndrome, in which there may be remnants of distal segments, unlike the transverse deficiency of formation of the upper limb, in which distal elements do not develop at the level at which the limb has been truncated, product of failure in the differentiation of the proximal-distal axis in embryonic life.
Congenital longitudinal failure of formation of the upper limb
Congenital deficiencies in longitudinal growth of the upper limb include all malformations in which the limb reaches total or partial involuted distal anatomical segments with the absence of some proximal segments (Figure 3). It occurs because the differentiation of the proximal-distal axis has been modified; it includes varieties of preaxial, central and post-axial presentation, according to the absence of segments in relation to their anatomical location in the upper limb. In some patients true phocomelia may occur (Figure 4), when they present longitudinal growth deficiency of the arm and forearm with preservation of the hand or its more distal segments (12,15, 22).
The most severe cases of patients with cessation of longitudinal growth of the upper limb, in whom there is complete absence of the limb, should be classified in semiology as patients with amelia (Figure 4C). For these, the possibility of rehabilitation is based on the use of external prostheses, given that the lack of tissue makes complete reconstruction of the limb impossible (16).
Preaxial longitudinal congenital failure of formation of the upper limb
Radial longitudinal or preaxial upper limb deficiencies include all congenital malformations of the hand or forearm ranging from mild radial hypoplasia to complete radial agenesis (12, 23). In general, they are characterized by shortening of the forearm with radial deviation at the radiocarpal joint; it is known in semiology as radial club hand (Figure 5). In some patients it is associated with thumb agenesis.
Radial longitudinal deficiencies of the upper limb are the most common longitudinal deficiencies. They have an estimated incidence of 0.5 cases per 10,000 live births (23.24). The penetrance of radial longitudinal deficiency is classified according to the degree of hypoplasia or radial agenesis, for which the classification of Bayne and Klug is used (25).
In the case of radial deficiencies in longitudinal formation, a prevalence of 1 per 5,000 live births has been reported. Its presentation with a syndromic disease should not be underestimated, since up to one third of the neonates diagnosed with radial longitudinal deficiency have pathologies of cardiovascular malformations, hematological dyscrasias, renal malformations and gastrointestinal dysfunctions. Therefore, they should always be referred for evaluation by specialized medicine, in order to carry out a comprehensive evaluation of the patient (12, 26, 27).
Central longitudinal congenital failure of formation of the upper limb.
It is known in medical semiology as cleft hand (Figure 5C). It occurs as involution or total absence of the soft tissues or bony structures of the central rays of the hand. In some occasions it can occur associated to syndactyly or synostosis of the central rays (12, 28). Central deficiency in the formation of the hand encompasses a wide spectrum of presentation, so the classification of these patients for surgical therapeutic planning has been considered a challenge throughout history. One of the most accepted classifications currently by hand surgeons is the Manske and Halikis classification (29, 30). This is based on the condition of the first interdigital space, assuming that its condition will define the patient’s prognosis in terms of functionality for clamping and a favorable esthetic result (29).
Post-axial longitudinal congenital failure of formation of the upper limb. It is estimated that post-axial or ulnar longitudinal congenital failure of formation of the upper limb occurs 4 to 10 times less per 100,000 live births than radial longitudinal congenital deficiency (12, 31, 32).
Most ulnar longitudinal deficiencies are not associated to other congenital malformations different from the musculoskeletal system, unlike the longitudinal radial deficiencies (12, 26, 27). However, an association with fibular deficiency in the lower limbs, congenital scoliosis or other upper limb malformations has been described. Up to 90% of the patients with ulnar longitudinal deficiencies present absence of one or more digits of the hand, and up to 30% of them present syndactyly in the affected upper limb (27,33). It has a variable spectrum of presentation ranging from ulnar hypoplasia to ankylosis of the humerus-ulnar joint (12).
Upper limb malformations due to failure of differentiation or separation of parts: type II
Failure of differentiation or separation of parts of the upper limb comprises the second group of congenital malformations described by Swanson. They include failures of soft tissues separation or even bone component separation (16). In this second group are all the malformations in which all the basic units of the upper member develop; however, not until its final form, so it does not reach the expected differentiation. Malformations can occur in any area of the upper limb. The most common included within this group are syndactyly, symphalangism or contracture due to failure of formation of muscles, ligaments or capsular structures.
Syndactyly
Syndactyly occurs when there is a failure of separation by apoptosis of the interdigital tissue, so an abnormal connection of tissues between them is maintained. It is one of the most frequent congenital malformations of the hand. The most frequent presentation is complete syndactyly, in which the connection between two fingers is preserved along the entire length of the digits. It usually occurs between the third and fourth interdigital space (12,16, 34).
Most studies have reported a prevalence of 1-10 per 100,000 live births. However, some authors have reported prevalences as high as 40 per 100,000 live births (34, 35, 36).
It is classified as simple syndactyly, when there is only soft tissue involvement, or as complex syndactyly, when there is fusion of associated skeletal structures. In some cases it occurs bilaterally symmetrical or asymmetrical (34). In addition, it may occur in association with other congenital malformations of the hand. With some frequency it is associated with brachidactyly; in these cases, the malformation is called symbrachidactyly (37).
Symphalangism
Symphalangism refers to a failure of segmentation of the interphalangeal joints of the fingers. It is usually evident in the proximal interphalangeal joint of the fifth finger, and does not affect the length of the fingers, although it may occur combined in patients with brachysymphalangism, that is, shortening of the usual length of the fingers, associated with failure of joint segmentation (12, 16, 38, 39).
Camptodactyly
Camptodactyly refers to upper limb malformations resulting from painless contracture of the proximal interphalangeal joint, usually in the fifth finger (40, 41). Most patients present asymptomatic, without signs of local joint inflammation, and it corresponds to an incidental finding on physical examination. It should be noted that on physical examination the metacarpophalangeal and distal interphalangeal joints present with compensatory malformations as a sequence; however, they do not understand the primary alteration in camptodactyly. It occurs bilaterally in more than half of the patients. It is attributed to an aberrant insertion of the lumbrical muscles into the superficial flexor muscle of the fingers or to a deficiency of the extensor muscles, that precipitates osteotendinous and capsular changes in the joint, leading to camptodactyly (12, 40, 42).
Clinodactyly
Clinodactyly is more common than camptodactyly and, at the same time, less problematic than camptodactyly. It refers to a deviation of a finger in the coronal plane. It is usually produced by abnormal delta morphology of the middle phalanx of the fifth finger (Figure 6A), generating a deviation of more than 10 degrees of the distal interphalangeal joint (12, 43, 44). It occurs more frequently bilaterally and corresponds to a malformation with little functional limitation. Between 35% and 79% of cases, clinodactyly presents with a diagnosis of Down syndrome (12, 44).
Synostosis
Finally, synostosis comprises the most severe variant of alterations in upper limb differentiation. It occurs at any anatomical level and includes all the malformations in which the bone components do not separate. It is a generic term for bone structures that are fused together when they should normally be separated. Among the most common are transverse metacarpal synostosis, in which the metacarpals of the fourth and fifth rays are fused. In some cases proximal radial-ulnar synostosis occurs. Cases of upper limb synostosis can be associated with fetal alcohol syndrome, trisomy 13 or trisomy 21, so a comprehensive and multidisciplinary assessment of the patient should always be done (12, 45, 46, 47).
Upper limb malformations by duplication: type III
These are the malformations that occur due to early alterations in embryonic development with changes in the apical ectoderm, zone of ectopic polarizing activity and SHH signaling. The spectrum of penetrance ranges from slight duplications, in the case of digits or skin appendages, to severe cases of duplication of the whole hand in patients with mirrored hands, or even duplication of the whole upper limb. Polydactyly, a malformation within this category, must be classified into pre-axial and post-axial duplications, according to its location with respect to the axis of the hand.
Polydactyly
This is the expression of a supernumerary digit. It is the most common upper limb congenital malformation. It is estimated that it occurs with a frequency of 1 case for every 700 to 1,000 live births (48). It usually presents as a soft tissue stump of variable size and shape; less frequently, it contains some remnant of bone structures. According to this, they are classified into type A supernumerary digit, which simulates an almost normal digit, and type B supernumerary digits, which are presented as a small stump of rudimentary or pedunculated soft tissues (12, 49). The most common form of polydactyly is thumb duplication (Figure 7), followed by post-axial duplication and central polydactyly (12, 50).
Ulnar dimelia
Ulnar dimelia or mirror hand is described as duplication of the ulna with or without duplication of the radius, accompanied by an abnormally increased number of digits in the absence of the development of a thumb. Different authors have attributed this malformation to an aberrant high expression of SHH over the radial border of the upper limb bud (51, 52, 53). The clinical presentation of these patients is characterized using the Al-Qattan classification (54, 55). In this classification, patients are categorized according to duplicate structures, but it is of little use in directing the surgical strategy or the esthetic and functional prognosis.
Upper limb malformations due to overgrowth: type IV
Upper limb malformations due to overgrowth can affect the entire limb. It is attributed to an overgrowth of the skeletal components of the limb with soft tissues of usual morphology. They include an increase in the size of the arm, forearm, hand or digits (12,16).
Macrodactyly
Macrodactyly comprises the excessive and disproportionate growth of all single or multi-digit structures (56). Pre-axial presentation has been reported more frequently in the medical literature. It usually occurs in isolation or in some cases associated with lipofibromatosis of local nerve fibers, most often over the distribution corresponding to the median nerve. It is also associated to patients with neurofibromatosis or vascular alterations such as hemangiomas and venous insufficiency disease (12, 56, 57).
Upper limb malformations due to growth restriction or growth failure: type V
They refer to all forms of hypoplasia of the upper limb or parts of it, that is, it corresponds to the whole limb, only arm, forearm, hand or hypoplasia of one or more digits (12,16). They must be distinguished from the congenital malformations of the first group in Swanson classification, and for this it is necessary to consider that in cases of hypoplasia there are no missing skeletal or soft tissue parts, unlike cases of longitudinal growth deficiency. On the contrary, the parts of the limb are complete, although involuted, resulting in limb hypoplasia. The most distal expression of cases in this category includes nail hypoplasia. Although it can occur in proximal structures and affect only the arm, forearm, hand, metacarpus or phalanges in isolation or in combination with any of the mentioned structures (12,16, 58, 59).
Brachymetacarpia and brachidactyly
It is called brachymetacarpia if it presents with isolated metacarpal hypoplasia. On the contrary, patients with hypoplasia of one or more phalanges are said to have brachydactyly (Figure 8) or brachyphalangia (59, 60).
Thumb hypoplasia
Patients with thumb hypoplasia may present with this malformation alone or in combination with other pre-axial deficiencies, as it happens more frequently. In this case, it should be classified in the group of the malformation that predominates for the patient (12, 16, 61, 62).
According to the absence of structures, hypoplasia differs from Müller’s classification, modified by Blauth (63), which includes five categories according to the absence of musculoskeletal structures, narrowness of the first interdigital space, absence of thenar muscles and instability of the respective metacarpophalangeal joint, abnormalities of extrinsic muscles with insertion into the thumb or floating thumb (63, 64).
Upper limb malformations due to congenital constriction band syndrome: type VI
Their frequency is estimated at 1 per 1,200 live births (65.66). These are congenital malformations resulting from a sequence of events leading to focal limb necrosis. This malformation occurs mainly during the post-embryonic stage. That is, it does not correspond to a failure in the embryonic development of the limb, but to an amputation by annular bands coming from chorionic tissue that are organized in the form of a tight band on the limb at any level, so that they produce ischemia, necrosis and intrauterine amputation of the most distal remnants, with scarring of the stump in that area (Figure 9). In the most severe cases, amputation of the entire limb occurs, but it can be at any level (12,16, 65, 67).
It is called acrosyndactyly or pseudosyndactyly in patients or fetuses in which a fusion of the digits is generated as part of the healing process to an injury due to amniotic band syndrome, in a patient or fetus in which there was no failure in the process of interdigital apoptosis and the digits were adequately formed (12, 65).
Upper limb malformations due to generalized skeletal abnormalities: type VII
This is the last group of congenital upper limb malformations described by Swanson. It includes patients who have failure of formation of the upper limb as a result of alterations in generalized skeletal development; for example, in the case of patients with dyschondroplasia, achondroplasia, diastrophic dwarfism and congenital multiple arthrogryposis (12,16). The review of each of these pathologies and their manifestations exceeds the objective of this article.
Conclusions
Congenital upper limb malformations are relatively common in newborns and fetuses. They pose a challenge for health professionals, and should be approached from the phenomena of embryonic development of the extremities to understand, identify and diagnose them in a timely manner, in order to refer patients to specialized medical management as required. This optimizes their functional and esthetic prognosis, when they receive the appropriate surgical interventions.
The differentiation of congenital upper limb malformations should make the health professional suspect their possible association with other systemic and musculoskeletal malformations which should be correctly described in the medical history or in the fetal necropsy report.
Acknowledgments
The authors would like to thank the parents or guardians of the fetuses who underwent necropsy.
REFERENCES
1. Arteaga Martínez SM, García Peláez MI. Desarrollo del sistema esquelético. En: Embriología humana y biología del desarrollo. Bogotá: Editorial Médica Panamericana; 2017. p. 268. [ Links ]
2. Nielsen M, Miller S. Esqueleto apendicular. En: Atlas de anatomía humana. Bogotá: Editorial Médica Panamericana; 2011. p. 83. [ Links ]
3. Latarjet R, Ruiz Liard A. Miembro superior. En: Anatomía humana. Tomo 1. 5.ª ed. Bogotá: Editorial Médica Panamericana; 2019. p. 455-70. [ Links ]
4. Pró E. Anatomía clínica. 2.ª ed. Bogotá: Editorial Médica Panamericana; 2014. p. 750-1. [ Links ]
5. Moore KL. Anatomía con orientación clínica. Wolters Kluwer; 2019. p. 771-9. [ Links ]
6. Carlson B. Desarrollo de las extremidades. En: Human embryology and developmental biology. New York: Elsevier; 2014. p. 193-215. [ Links ]
7. Lifemap Discovery. Development of the limbs [internet]. 2020 [citado 2020 may 4]. Disponible en: https://discovery.lifemapsc.com/library/review-of-medical-embryology/chapter-69-development-of-the-limbs [ Links ]
8. Al-Qattan MM, Yang Y, Kozin SH. Embryology of the upper limb. J Hand Surg Am. 2009;34(7):1340-50. [ Links ]
9. Tamura K, Yonei-Tamura S, Yano T, Yokoyama H, Ide H. The autopod: its formation during limb development. Dev Growth Differ. 2008;50 Suppl 1:S177-87. https://doi.org/10.1111/j.1440-169X.2008.01020.x [ Links ]
10. Al-Qattan MM, Kozin SH. Update on embryology of the upper limb. J Hand Surg Am. 2013;38(9):1835-44. [ Links ]
11. Cunningham TJ, Duester G. Mechanisms of retinoic acid signalling and its roles in organ and limb development. Nat Rev Mol Cell Biol. 2015;16(2):110-23. [ Links ]
12. Gishen K, Askari M. Congenital hand anomalies: etiology, classification, and treatment. J Craniofac Surg. 2014;25(1):284-94. [ Links ]
13. Dy CJ, Swarup I, Daluiski A. Embryology, diagnosis, and evaluation of congenital hand anomalies. Curr Rev Musculoskelet Med. 2014;7(1):60-7. [ Links ]
14. Zarante I, Franco L, López C, Fernández N. Frecuencia de malformaciones congénitas: evaluación y pronóstico de 52.744 nacimientos en tres ciudades colombianas. Biomedica [internet]. 2010;30(1):65-71. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-41572010000100009 [ Links ]
15. Bermejo-Sánchez E, Cuevas L, Amar E, Bianca S, Bianchi F, Botto LD, et al. Phocomelia: a worldwide descriptive epidemiologic study in a large series of cases from the International Clearinghouse for Birth Defects Surveillance and Research, and overview of the literature. Am J Med Genet C Semin Med Genet. 2011;157C(4):305-20. https://doi.org/10.1002/ajmg.c.30320 [ Links ]
16. Swanson A B. A classification for congenital limb malformations. J Hand Surg Am. 1976;1(1):8-22. [ Links ]
17. Tonkin M A, Tolerton SK, Quick TJ, Harvey I, Lawson RD, Smith NC, et al. Classification of congenital anomalies of the hand and upper limb: development and assessment of a new system. J Hand Surg Am. 2013;38(9):1845-53. https://doi.org/10.1016/j.jhsa.2013.03.019 [ Links ]
18. Laub Jr DR, Hentz VR, Ladd AL. Congenital hand deformities. En: Plastic surgery: indications, operations and outcomes. 2nd ed. New York: Mosby; 2000. p. 1735-48. [ Links ]
19. Farr S, et al, Peromelia-congenital transverse deficiency of the upper limb: a literature review and current prosthetic treatment. J Child Orthop. 2018;12(6):558-565. [ Links ]
20. Jain S, Lakhtakia PK. Profile of congenital transverse deficiencies among cases of congenital orthopaedic anomalies. J Orthop Surg (Hong Kong). 2002;10(1):45-52. [ Links ]
21. Mo T. Pediatric orthopedics. En: Congenital deformities. Philadelphia: WB Saunders; 1990. p. 104-12. [ Links ]
22. Osadsky C R. Phocomelia: case report and differential diagnosis. Radiol Case Rep. 2011;6(4):561. [ Links ]
23. de Jong JP, Moran SL, Vilkki SK. Changing paradigms in the treatment of radial club hand: microvascular joint transfer for correction of radial deviation and preservation of long-term growth. Clin Orthop Surg. 2012;4(1):36-44. [ Links ]
24. Ekblom AG, Laurell T, Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: a total population study from Stockholm, Sweden. J Hand Surg Am. 2010;35(11):1742-54. [ Links ]
25. Bayne LG, Klug MS. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am. 1987;12(2):169-79. [ Links ]
26. Colen D L, Lin IC, Levin LS, Chang B. Radial longitudinal deficiency: recent developments, controversies, and an evidence-based guide to treatment. J Hand Surg Am. 2017;42(7):546-63. https://doi.org/10.1016/j.jhsa.2017.04.012 [ Links ]
27. Koskimies E, Lindfors N, Gissler M, Peltonen J, Nietosvaara Y. Congenital upper limb deficiencies and associated malformations in Finland: a population-based study. J Hand Surg Am. 2011;36(6):1058-65. https://doi.org/10.1016/j.jhsa.2011.03.015 [ Links ]
28. Manske PR, Goldfarb CA. Congenital failure of formation of the upper limb. Hand Clin. 2009;25(2):157-70. [ Links ]
29. Sharma A, Sharma N. A comprehensive functional classification of cleft hand: the DAST concept. Indian J Plast Surg. 2017;50(3):244-50. [ Links ]
30. Manske PR, Halikis MN. Surgical classification of central deficiency according to the thumb web. J Hand Surg Am. 1995;20(4):687-97. [ Links ]
31. Watts AC, Hooper G. Congenital hand anomalies. Curr Orthop. 2006;20:266-73. [ Links ]
32. Miller JK, Wenner SM, Kruger LM. Ulnar deficiency. J Hand Surg Am. 1986;11(6):822-9. [ Links ]
33. Bauer AS, Bednar MS, James MA. Disruption of the radial/ulnar axis: congenital longitudinal deficiencies. J Hand Surg Am. 2013;38(11):2293-302; quiz 2302. [ Links ]
34. Malik S. Syndactyly: phenotypes, genetics and current classification. Eur J Hum Genet. 2012;20(8):817-24. [ Links ]
35. Hay S. Incidence of selected congenital malformations in Iowa. Am J Epidemiol. 1971;94(6):572-84. [ Links ]
36. Castilla EE, Paz JE, Orioli-Parreiras IM. Syndactyly: frequency of specific types. Am J Med Genet. 1980;5(4):357-64. [ Links ]
37. Goodell P B, Bauer AS, Sierra FJ, James MA. Symbrachydactyly. Hand (N Y). 2016;11(3):262-70. https://doi.org/10.1177/1558944715614857 [ Links ]
38. Baek GH, Lee HJ. Classification and surgical treatment of symphalangism in interphalangeal joints of the hand. Clin Orthop Surg. 2012;4(1):58-65. [ Links ]
39. Cushing H. Hereditary anchylosis of the proximal phalan-geal joints (symphalangism). Genetics. 1916;1(1):90-106. [ Links ]
40. Singh V, Haq A, Priyadarshini P, Kumar P. Camptodactyly: an unsolved area of plastic surgery. Arch Plast Surg. 2018;45(4):363-6. https://doi.org/10.5999/aps.2017.00759 [ Links ]
41. Choi B R, Lim YH, Joo KB, Paik SS, Kim NS, Lee JK, et al. Camptodactyly, arthropathy, coxa vara, pericarditis (CACP) syndrome: a case report. J Korean Med Sci. 2004;19(6):907-10. https://doi.org/10.3346/jkms.2004.19.6.907 [ Links ]
42. McFarlane R M, Classen DA, Porte AM, Botz JS. The anatomy and treatment of camptodactyly of the small finger. J Hand Surg Am. 1992;17(1):35-44. https://doi.org/10.1016/0363-5023(92)90110-b [ Links ]
43. Flatt A E. The troubles with pinkies. Proc (Bayl Univ Med Cent). 2005;18(4):341-4. [ Links ]
44. Leung AK, Kao CP. Familial clinodactyly of the fifth finger. J Natl Med Assoc. 2003;95(12):1198-200. [ Links ]
45. Tsai J. Congenital radioulnar synostosis. Radiol Case Rep. 2017;12(3):552-4. [ Links ]
46. Cleary JE, Omer Jr GE. Congenital proximal radio-ulnar synostosis: natural history and functional assessment. J Bone Joint Surg Am. 1985;67(4):539-45. [ Links ]
47. Hansen OH, Andersen NO. Congenital radio-ulnar synos<tosis: report of 37 cases. Acta Orthop Scand. 1970;41(3):225-30. [ Links ]
48. Ahmed H, Akbari H, Emami A, Akbari MR. Genetic overview of syndactyly and polydactyly. Plast Reconstr Surg Glob Open. 2017;5(11):e1549. https://doi.org/10.1097/GOX.0000000000001549 [ Links ]
49. Abzug JM, Kozin SH. Treatment of postaxial polydactyly type B J Hand Surg Am. 2013;38(6):1223-5. [ Links ]
50. Malik S. Polydactyly: phenotypes, genetics and classification. Clin Genet. 2014;85(3):203-12. [ Links ]
51. Tomaszewski R, Bulandra A. Ulnar dimelia-diagnosis and management of a rare congenital anomaly of the upper limb. J Orthop. 2015;12(Suppl 1):S121-4. [ Links ]
52. Chinegwundoh JO, Gupta M, Scott WA. Ulnar dimelia: is it a true duplication of the ulna? J Hand Surg Br. 1997;22(1):77-9. [ Links ]
53. Jameel J, Khan AQ, Ahmad S, Abbas M. Ulnar dimelia variant: a case report. J Orthop Traumatol. 2011;12(3):163-5. [ Links ]
54. Al-Qattan M, Al-Thunayan A, De Cordier M, Nandagopal N, Pitkanen J. Classification of the mirror hand-multiple hand spectrum. J Hand Surg Br. 1998;23(4):534-6. https://doi.org/10.1016/s0266-7681(98)80140-x [ Links ]
55. Gaba S, John N, Bhogesha S, Singh O, Vemula GK. Mirror hand: an uncommon neglected case managed with pollicisation. World J Plast Surg. 2017;6(2):263-5. [ Links ]
56. Dell P C. Macrodactyly. Hand Clin. 1985;1(3):511-24. [ Links ]
57. Barsky A J. Macrodactyly. J Bone Joint Surg Am. 1967;49(7):1255-66. [ Links ]
58. Bisneto E N. Congenital deformities of the upper limbs. Part I: failure of formation. Rev Bras Ortop. 2012;47(5):545-52. [ Links ]
59. Bisneto EN. Congenital deformities of the upper limbs. Part III: overgrowth; undergrowth; streeter and others. Rev Bras Ortop. 2013;48(2):121-5. [ Links ]
60. Miura T, Torii S, Nakamura R. Brachymetacarpia and brachyphalangia. J Hand Surg Am. 1986;11(6):829-36. [ Links ]
61. Sayadi L, Chopan M, Laub D. Thumb hypoplasia. Eplasty. 2015;15:ic62. [ Links ]
62. James MA, McCarroll Jr HR, Manske PR. Characteristics of patients with hypoplastic thumbs. J Hand Surg Am. 1996;21(1):104-13. [ Links ]
63. Blauth W. The hypoplastic thumb. Arch Orthop Unfallchir. 1967;62(3):225-46. [ Links ]
64. Tonkin M. Surgical reconstruction of congenital thumb hypoplasia. Indian J Plast Surg. 2011;44(2):253-65. [ Links ]
65. Walter J H Jr., Goss LR, Lazzara AT. Amniotic band syndrome. J Foot Ankle Surg. 1998;37(4):325-33. [ Links ]
66. Paladini D, Foglia S, Sglavo G, Martinelli P. Congenital constriction band of the upper arm: the role of three-dimensional ultrasound in diagnosis, counseling and multidisciplinary consultation. Ultrasound Obstet Gynecol. 2004;23(5):520-2. https://doi.org/10.1002/uog.1042 [ Links ]
67. Shetty P, Menezes LT, Tauro LF, Diddigi KA. Amniotic band syndrome. Indian J Surg. 2013;75(5):401-2. https://doi.org/10.1007/s12262-012-0468-x [ Links ]
Received: May 24, 2020; Accepted: July 03, 2020











 texto em
texto em