Introduction
The need to decrease the gaps between what is taught in the classroom as professionalism, and what students encounter in hospitals is well known. For this reason, Colombia and other countries have declared the importance of generating core competencies related to humanistic development and professionalism (H/P) for patients, peers and the health team (1, 2, 3).
There are different approaches to teaching H/P in medicine, with varying impacts and effectiveness. Learning experiences such as critical reflection, early clinical contact, and role modeling have better effects on the acquisition of H/P competencies than other techniques such as lectures (4, 5, 6).
Despite this, there are gaps between health curricula that state the development of H/P competencies and what students encounter in hospitals (4). In practice, this clash is due in part to the lack of provision of continuous experiences that situate learning and generate opportunities for positive modeling in these competencies (4).
Likewise, the teaching of humanization in the outpatient setting involves specific challenges: (i) time and productivity pressures; (ii) the desire to build a strong bond between the professional and the patient when the student is present, and (iii) psychosocial aspects of the outpatient (adherence, somatization, conceptions, administrative processes, impact of the disease, etc.) (3, 4).
Consequently, the following question arises: how can an ambulatory practice setting contribute to the provision of experiences that enable the development of H/P competencies?
The “Te Acompañamos” (We Accompany you) program as an experiential learning strategy in H/P, was born in a Colombian outpatient care institution (Javesalud) in 2017, to achieve an impact on the patient and provide an accompaniment to older adults who are cared for in Javesalud throughout the care process, to improve their experience; also in the student, implementing a teaching strategy that closes the gaps described in H/P training. In this way, the program proposes the following student learning objectives: (i) provide service learning experiences from the early stages of their clinical training to develop empathy as a core value; (ii) systematically provide a formal opportunity for the trainee to recognize their patient, their emotional states, fears and barriers in the care process; (iii) internalization and reflection of the service experience to their medical work outside the scope of the medical act in consultation.
This article presents the results of the program, emphasizing those related to student learning objectives. The analysis was conducted in light of the organizational strategy of humanized culture.
Materials and methods
The implementation of the program occurred in four steps, which are described below. In the first stage, induction and training in the program was performed at the beginning of outpatient primary care training. The objectives of the program, the approach to patients, the behaviors to avoid and the script were presented. In the second stage, activities were programmed and each student was assigned a day of accompaniment. In the third stage, the student received the button that identified him/her as a participant in the program, the patient registration and training form by the medical center in the administrative aspects that the student guiding the patient should know. At this stage, the students selected their patients and offered them accompaniment in the procedures before, during and after the consultation (obtaining the medicines, organizing their exams, helping them get dressed, reinforcing information, travel, paperwork, etc.). At the end, the student submitted the form to the medical center for internal control of the program. Finally, the student’s experience was evaluated through a qualitative tool of four open-ended questions.
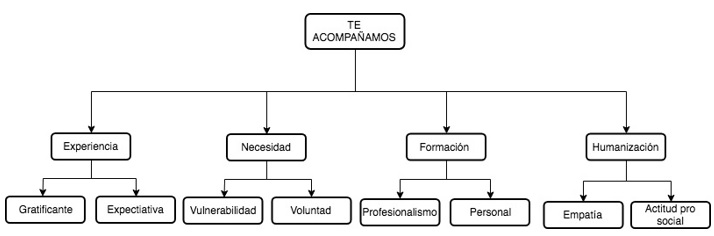
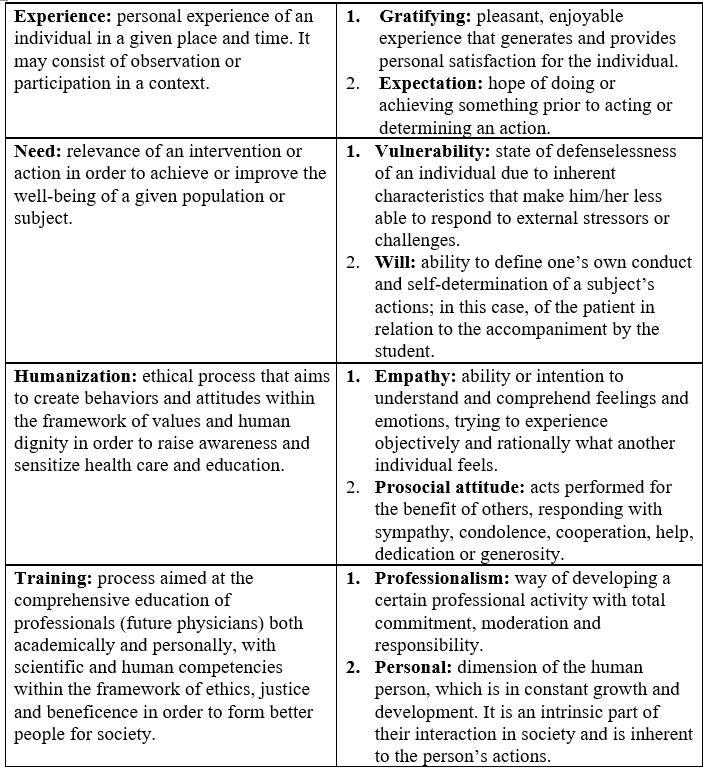
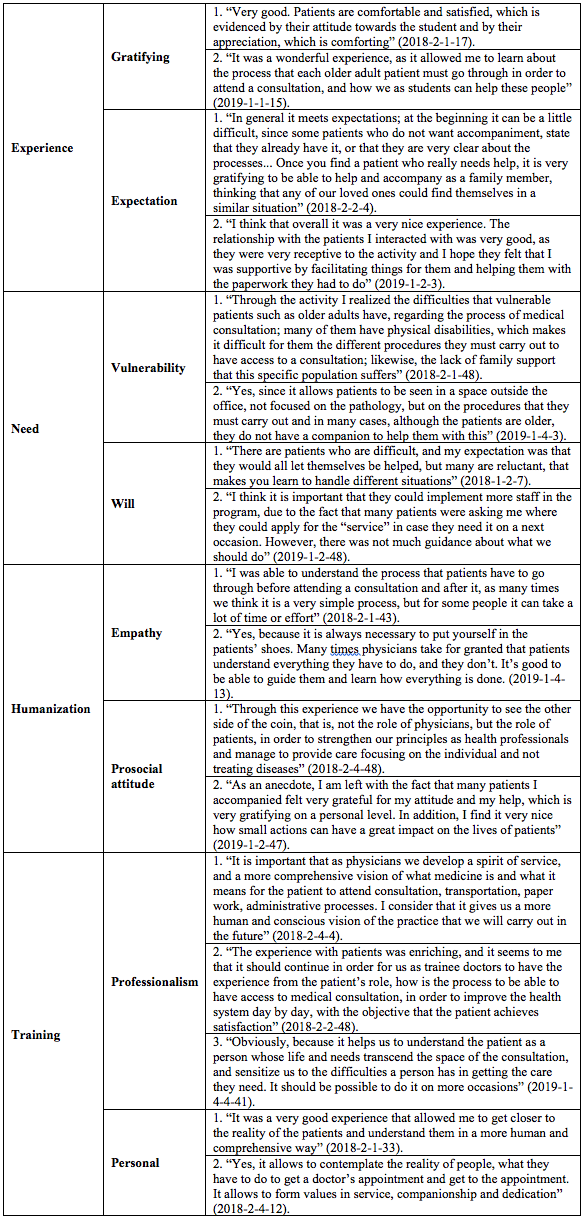
For the analysis of student perception results, survey responses were categorized according to the most frequent qualifying adjective (Figure 1 and Table 1). The year-semester-number of the question-participant number (e.g., 2017-2-1-3) was used as nomenclature for each response.
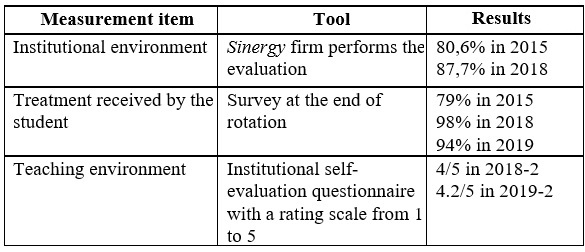
Patient satisfaction was measured by means of a biannual telephone survey, with a four-question Likert-type scale, where one was the most negative rating and five was the most positive. The measurements of humanized culture in Javesalud are described in Table 2.
Results
Until the end of 2019, 289 students participated and 824 older adults benefited. The satisfaction evaluation from 2017 to 2019 shows an average of 4.82/5. The results of humanized culture in Javesalud are presented in Table 2.
Table 3 shows the outstanding responses from 73 student surveys. In the “Experience” category, an attitude of bilateral appreciation is observed, with an adequate scope of what is expected for students, as they understand that academic training goes beyond scientific knowledge. In the “Need” category, there is a recognition of the vulnerability of older adults and a willingness to support and accompany them.
In the “Humanization” category, empathy and prosocial attitude are recognized as fundamental behaviors in professional training. The students approached the patient’s experiences and generated concrete actions to help him/her.
Regarding the “Training” category, the program seeks to build professionalism, seen from the integral education of human values and teachings that foster growth in different personal dimensions and social interaction.
Discussion
A teaching experience in professionalism, understood as “Construct based ideologically on value orientation,” was presented. This definition is adopted from Birden et al. (5), as it compiles a list of overlapping attributes that define the professional competence that a physician should have. These attributes that must be developed and are not innate are professionalism, humanism, spirituality, and morality. This definition is adopted because it incorporates empathy as a core value, the latter explained as a way of translating the prosocial orientation into prosocial behaviors (those that serve the benefit of another person) (6). This was evident in the “Humanization” category, where 27 people stated that they could put themselves in the other person’s situation with this program (e.g., “...it allows us to approach health care as patients, to put ourselves in their shoes” [2018-2-4-24]).
The perception of benefiting older adults was evidenced by 19 students, “Experience” category (e.g., “I could accompany him to complete administrative procedures that he did not understand” [2018-2-2-30]). These findings are consistent with the patients’ perception of help/well-being (see Table 2). Prosocial acts also include the perception of feeling good about helping another person (6), which was evidenced in the “Rewarding” subcategory (e.g., “but in my case there was more than a simple ‘thank you,’ because there was the satisfaction they expressed” [2018-2-2-29]). However, the recognition of not being able to help was perceived by 12 students. This result is not negative, as it fosters in students the habit of considering different ways of helping and improving the understanding of the individuality of the human being (7).
The H/P training for health professionals described by Gordon (8), describes three elements that must be taken into account for its implementation: (i) the recognition of the variables that influence the doctor-patient relationship (context factors, insurance, health system, social determinants); (ii) how these variables influence the doctor-patient relationship, and (iii) find ways to always advocate the patient’s perspective first (4). Of the students surveyed, 40 made explicit different variables that affect medical care (“Training” category). These are some examples: “Yes, because it allows to know a different viewpoint, a vision outside the office and to understand that sometimes patients can have many problems at the administrative level” (2017-2-4-11); “It opened up our knowledge of the problems that these people face on a day-to-day basis, in terms of making appointments and obtaining test results... It allowed us to know first-hand their complaints about the service provided by the entity and the staff” (2018-2-1-6).
Twenty-two students in the “Training” category show their attitude to advocate for the patient —Gordon’s point 3 (8)—: for example, “It allows you to put yourself on the other side, on the patient’s side and what happens after leaving the office and during the waiting time” (2017-2-4-6). Advocating the patient’s perspective creates positive spaces for understanding what it is like to be in the other person’s situation, also called interpersonal introspection. As an effect, the “me (professional) vs. them (patients)” view in students, which is usually in the hidden curriculum of medical education, is diminished (6).
One advantage of this strategy is its integration within the institutional humanization program. This is relevant because such strategies cannot remain peripheral efforts (3, 6). The literature suggests focusing on the institution and its values as the basis for teaching and learning H/P (4, 5). Javesalud had the best organizational climate and culture results in its history at the time of the implementation of the program (87.8%), as a result of actions that the humanization program undertook in 2015 (previous climate measurements: 80%). The measurement that the students made of the treatment they received was at 98% during the implementation of the program (measurements before 2015 were between 75% and 80%), and patient satisfaction has remained above 90% for the past two years. “Te Acompañamos” is, therefore, a strategy immersed in a humanized culture that helps bridge the gap between the “must be” of professionalism and hospital reality. The “Need” category shows how from the beginning of the program, there is a specific sensitivity to the vulnerability of the other (e.g., “I realized the difficulties that the most vulnerable patients such as older adults have” [2018-2-1-48]).
The strategy provides other novel elements in terms of knowledge generation since most of the documented experiences in H/P training are from the perspective of highly complex services, such as palliative care, intensive care and emergency care (4). Javesalud is an outpatient care institution that provides health services in the framework of outpatient primary care with challenges and difficulties of time pressures, productivity of professionals, special attributes of the population being cared for (older adults, mostly with chronic diseases). Therefore, the research and development of this type of strategy makes it possible to “decomplexify” the teaching of humanization of special services and to ground them in more practical and common realities for any general practitioner.
Another contribution of the strategy is to overcome the problem of when is the most appropriate time to teach humanization in health careers. Several authors have pointed out that doing it very early may not have a major impact, given that in the first semesters “hard” subjects have priority and there is not much clinical contact. In conytrast, defining teaching strategies in humanization in more advanced semesters may have the difficulty of dealing with a student who has already prefabricated a concept according to role modeling and it is difficult to unlearn certain behaviors. The program is developed in the sixth semester of medical school, which is an opportune and balanced moment in terms of training time (4).
The third contribution is the generation of a novel didactic strategy in humanization, by the patient outside the office. Most H/P experiences are described in the context of a clinical encounter with diverse results in the impacts on the development of these competencies (4, 5). This “out-of-office” experience allows the student to get to know the reality of the patient, the service and the health system.
Finally, this type of experience is designed by the faculty of the universities (5, 9), and a novel element is that it was built on the initiative of the students based on the perceptions of the “hidden curriculum” of Javesalud, and was aligned with the formal university curriculum.
Although the strategy is immersed in the culture of Javesalud, it needs to be integrated into a model such as Branch’s (9), which, in addition to professionalism experiences, includes spaces for critical reflection and support groups in the program. This integration has been tested in different institutions with results in improvements of communication skills and interest in psychosocial aspects of patients. It is contemplated to generate opportunities for continuity in other semesters and centers to guarantee training in the habit of professionalism (4).
A teaching strategy is presented in H/P that provides experiences for developing empathy as a central element and that is developed within the humanization policy of an outpatient care institution, with highly satisfactory results for students and patients. It is a way to bridge the gap between how professionalism should be taught and what happens in hospitals.
Conclusions
“Te Acompañamos,” as a teaching strategy in H/P in a Colombian outpatient care institution, is presented as a successful model and reference for the development and empowerment of fundamental qualities in the practice of a humanized medicine in medical students. The experiences in the medical practice scenarios transcend the theoretical knowledge acquired, as they allow the trainee doctors to approach the biopsychosocial context of the patient, which per se is part of the integral understanding and approach to the concept and definition of health of the World Health Organization (10).
The program has great achievements, among which stand out the learning process and humanization of the comprehensive training of the medical student, user satisfaction with the support and attention received in the center and the humanization of the care of the elderly in the outpatient services. In turn, the permanent evaluation of the institutional and teaching climate contributes to the continuous improvement of institutional policies, quality standards and teaching activities.
It is important to articulate medical professionalism-teaching strategies with the organizational culture and clinical practice scenarios to achieve adequate medical H/P training. The model could be reproduced in different healthcare scenarios and levels of complexity that have teaching-service agreements and healthcare personnel in training.











 text in
text in