Introduction
There is growing concern about the directly proportional relationship between the number of survivors and the rates of disability in preterm newborns, especially concerning important sequelae such as neurodevelopment, retinopathy of prematurity, and bronchopulmonary dysplasia (1), conditions clearly related to the immaturity of the organs at birth; as well as regarding the adverse effects of the therapies used to achieve their survival. These sequelae not only affect their quality of life but also have an impact on society as a whole, given the loss of skills (2) and the economic cost to health systems (3).
Bronchopulmonary dysplasia (BPD) is the most frequent cause of respiratory morbidity in premature infants who survive to the neonatal stage (4). Its incidence is inversely proportional to gestational age and newborn weight (5). This implies a long-term problem of pulmonary function, which results in the need for supplemental oxygen, increased susceptibility to respiratory infections, and significant associated mortality (6).
There are a variety of neurodevelopmental sequelae that require adequate screening and follow-up (7), particularly in this group, which presents greater neuropsychological complications (8). There is a directly proportional relationship between neurological alteration and earlier gestational age at birth, with high rates in the incidence of transient and mild neurological abnormalities (9), up to more severe and permanent forms of disability (10).
Retinopathy of prematurity (ROP) has a spectrum ranging from spontaneous regression to bilateral retinal detachment and total blindness (11). It is one of the main causes of infant blindness in third-world countries, and Colombia is responsible for 23.9% of cases (12). The Cooperative Cryotherapy Group for Retinopathy of Prematurity found that ROP occurred in 66% of children with a birth weight of 1250 g or less and 82% of children with a birth weight of less than 1000 g (13).
Thus, we have a group of pathologies that are a direct product of the prematurity of the newborn and its subsequent postnatal stage, which shares many risk factors that influence the development of these, and on many occasions have the possibility of being prevented. The objective of the research was to describe morbidity and mortality in newborns under 32 weeks of gestational age attended in a neonatal intensive care unit in Bogota (Colombia), between January 2018 and December 2020, and to determine the associated factors.
Materials and methods
Type of study and design
An observational, cross-sectional study with an analytical component was carried out. The inclusion criteria were all newborns under 32 weeks of gestational age, attended in a neonatal intensive care unit of a public hospital of high obstetric complexity and reference site in the city of Bogota, between January 2018, and December 2020, and who continued their follow-up in the Mother Kangaroo program of the same institution.
It should be clarified that patients with complications typical of prematurity, such as respiratory distress syndrome, enterocolitis, intraventricular hemorrhage, among others, are part of the inclusion criteria. The exclusion criteria were all newborns with major malformations, genetic diseases and serious or life-threatening diseases not related to the complications of prematurity.
Sample collection and processing
A non-probabilistic, convenience sampling was performed, in which all newborns who met the inclusion criteria were included. The mortality and morbidity of these patients was reviewed through inpatient and outpatient medical records, the single registry of affiliates and the outpatient records of the Mother Kangaroo program, pediatric neurology, physiatry, pediatric ophthalmology and pediatric pulmonology, where each of the comorbidities presented by the patients during their follow-up were described. This was determined by clinical, imaging or paraclinical findings.
Statistical analysis
Averages and medians were estimated for quantitative variables, as well as their respective measures of dispersion, according to the fit of the data to the normal distribution. Qualitative variables were presented as frequencies and percentages. Death registration and BPD were considered as dependent variables for the construction of the bivariate analysis. Averages were compared with Student's t-test; while medians were compared with the Mann-Whitney U test. Percentages were contrasted with the chi-square test (χ²), when expected values >5 were identified; otherwise, Fisher's exact test was used.
Statistically significant differences were taken into account as those with p values < 0.2 to be incorporated into the initial multivariate model. The logistic regression model was constructed based on the Backward stepwise strategy, in which the variables generating the highest p values were eliminated one by one. Finally, the most significant variables and those of greater relevance were left out because they were potential confounders. The analysis was performed in Stata software, version 12.
Results
During the study period, 157 newborns under 32 weeks were identified (33/629 births in 2020, 70/2198 births in 2019, and 54/1948 births in 2018). In the last year, the number of deliveries in the institution was affected by functional changes in the health network, given by the SARS-CoV-2 pandemic. Of the newborns, 108 met the inclusion criteria and were finally part of the analysis.
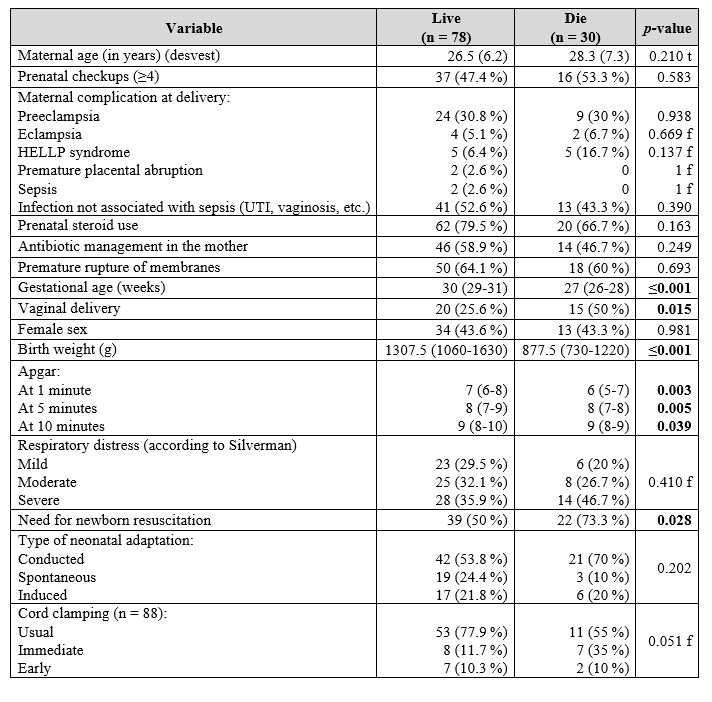
Concerning maternal characteristics, 9.26 % were adolescents; while 13.8 % were elderly mothers; 37 % were first pregnancy women; 13.9 % were of foreign origin, and 59.3 % were mothers in the subsidized health regime. Regarding antenatal care, 57/82 (69 %) received a complete pulmonary maturation scheme. Cesarean delivery occurred in 67.6 % of the mothers. The other maternal characteristics and information on the perinatal period are presented in Table 1.
Table 1. Maternal characteristics and perinatal history of newborns under 32 weeks of age, 2018-2020
f:Fisher's exact test
t:Student's t-test.
Among the newborns who developed severe respiratory distress syndrome (RDS), only 20 (47.6 %) received complete pulmonary maturation and 29 (69 %) required advanced resuscitation at birth. Regarding the characteristics of the newborn, the management in the delivery room and the clinical behavior in the early postnatal period are described in Table 2.
Table 2. Clinical and paraclinical findings and characteristics of the initial care of newborns less than 32 weeks of gestation, 2018-2020
f:Fisher's exact test
t:Student's t-test.
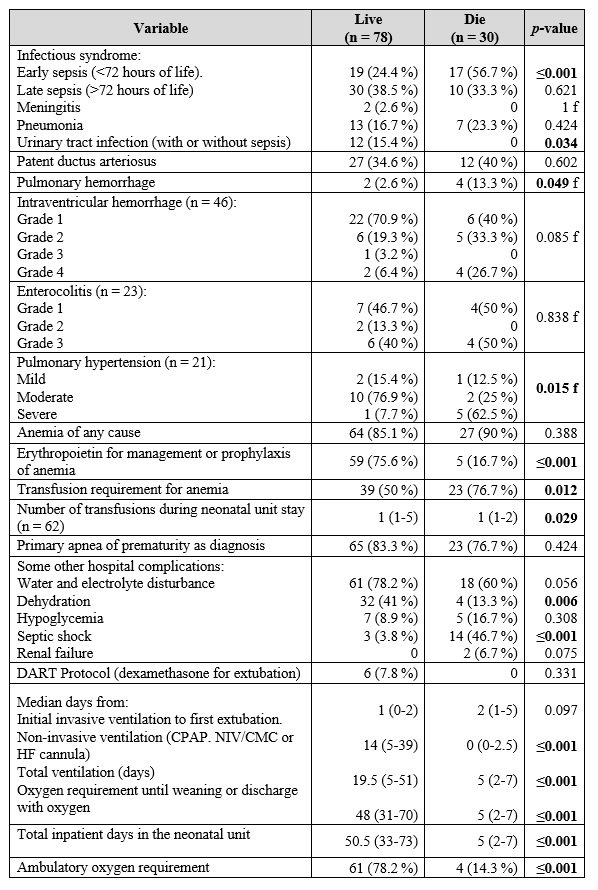
Table 3 shows the clinical outcomes. Among the sequelae explored among the surviving patients, no cases of infantile cerebral palsy, hypoxic-ischemic encephalopathy, or blindness were identified. The clinical outcomes identified were: one case of moderate retinopathy, five patients diagnosed with hypoacusis, eight patients with neurodevelopmental disorders, two with epilepsy, and one with hydrocephalus (who required surgical management); in addition to one case of periventricular leukomalacia.
Table 3. Inpatient and outpatient follow-up outcomes of preterm newborns, 2018-2020
f:Fisher's exact test
t:Student's t-test.
In patients who did not receive the full steroid regimen versus those who did receive the full regimen, neurodevelopmental impairment (33.3 % vs. 22.2 %; p = 0.618), enterocolitis (30.7 % vs. 17.54 %; p = 0.250), and early sepsis (19.23 % vs. 38.9 %; p = 0.129) were present. Of the survivors, 80.7 % (n = 63) received palivizumab prophylaxis before discharge. Nine patients developed bronchiolitis after hospital discharge, of which four (44.4 %) cases were found to have received a full palivizumab regimen.
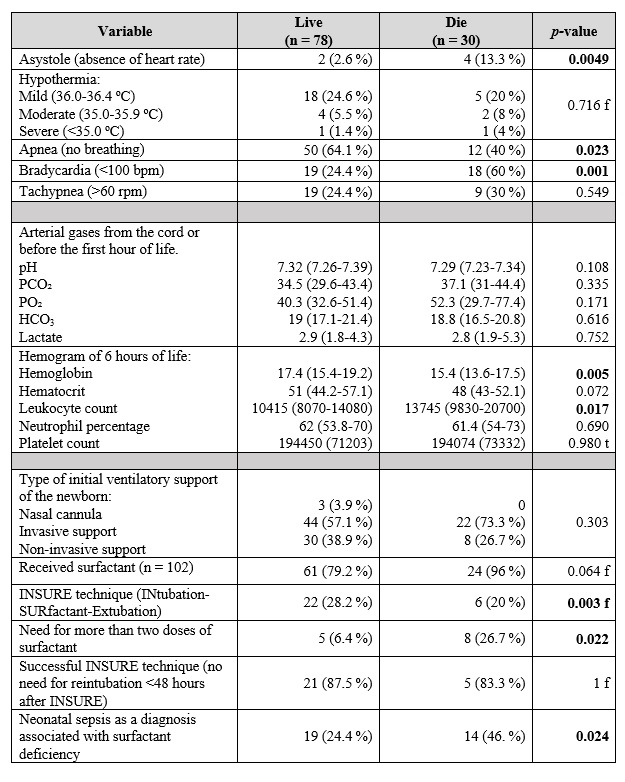
Thirty deaths were identified, which estimates mortality in this population of 27.7%. Within the cohort of deaths, it was striking that there was a higher frequency of incomplete pulmonary maturation with corticosteroids (53.3 % vs. 44.9 %; p = 0.430), sepsis as the main diagnosis associated with RDS in the newborn (46.7 % vs. 24.4 %; p = 0.024), and the need for ventilatory support at birth (100 % vs. 96.2 %; p = 0.559). The mean number of days of hospitalization in deceased participants found was 6.8 days (vs. 54.2 days among those who survived; p ≤ 0.001), with similar results for mean ventilator days (6.5 days vs. 28.7 days; p ≤ 0.001).
Based on the bivariate analysis presented, a multivariate logistic regression model was constructed to identify the factors associated with mortality in this population (Table 4).
Table 4. Multivariate analysis of factors associated with mortality in preterm infants, 2018-2020
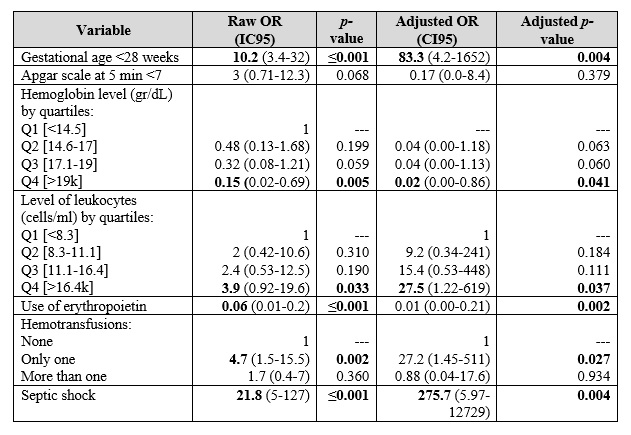
Pseudo R2 = 0.709 (p-value ≤ 0.001).
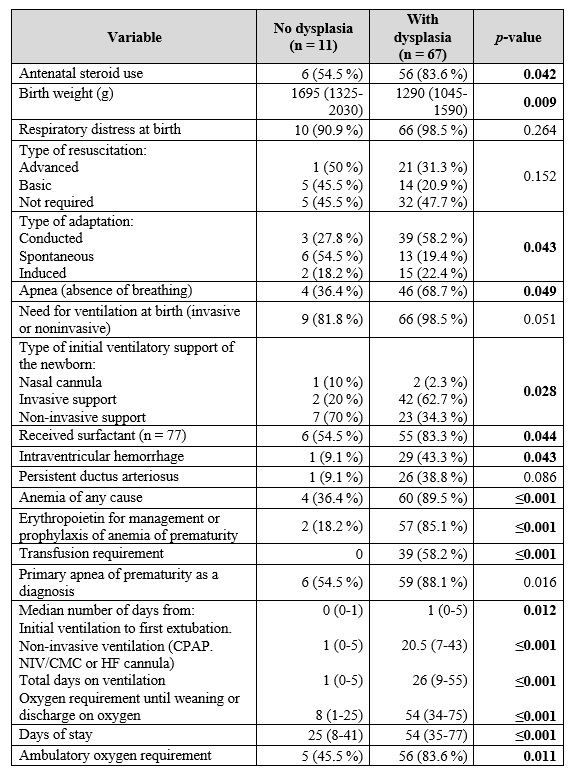
The outcome of BPD occurred in 67 (85.9 %) of the 78 survivors within this population (Table 5). Of these, 43 received full pulmonary maturation; 35.9 % (n = 28) developed severe respiratory distress syndrome at birth, and 37 were discharged with a need for home oxygen (median days of oxygen dependency = 30; RIQ = 10-90). Within the BPD cohort there is a higher proportion in the incidence of enterocolitis (22.4 % vs. 0 %; p = 0.110) and sepsis (68.6 % vs. 18.2 %; p = 0.002). Regarding surfactant use, 78.2 % (n = 61) received one dose and 6.4 % (n = 5) received at least two doses. The INSURE technique was successful in 28.2 % (n = 22); the success rate was higher in children with mild respiratory distress (34.8 %) and slightly lower in moderate and severe respiratory distress (28 % and 25 %, respectively; p = 0.862). In the multivariate analysis of factors associated with bronchopulmonary dysplasia, we observed how anemia constituted the most important risk factor for its development (ORa: 25.8; CI95 %: 4.37-149.9; p ≤ 0.001; pseudo-R²: 0.352, with p-value ≤ 0.001).
Discussion
The results obtained show a high rate of respiratory sequelae. Currently, BPD has a better prognosis and fewer long-term sequelae, but its incidence has not decreased over time. We found that children with lower birth weight, lower gestational age and longer duration of mechanical ventilation presented higher frequencies. There is a directly proportional relationship between the time of oxygen dependency and pulmonary compromise in terms of BPD (14), and inversely proportional to gestational age and newborn weight, ranging from 7% to 52% in children weighing less than 750 g (15).
Anemia was an independent risk factor for BPD. Suboptimal hemoglobin concentrations are associated with greater oxygenation impairment and longer ventilation times. The adverse effects of prolonged ventilation are strongly associated with adverse outcomes, and include, in addition, ROP and neurological disturbances. Different studies have shown how newborn RDS, sepsis, ventilator-associated pneumonia, mechanical ventilation, and red blood cell transfusion are the most important common risk factors for the development of BPD (16). Other factors found were the need for exogenous pulmonary surfactant at birth, patent ductus arteriosus, and necrotizing enterocolitis, frequent findings in other studies (17).
In patients in whom follow-up was completed, it was observed that the higher the chronological age after discharge, the lower the dependence on oxygen. In the first two years, hospitalizations due to respiratory causes are frequent (18), and although respiratory morbidity decreases with age, these children may present respiratory symptoms, need for oxygen, and alterations in pulmonary function beyond school age, and even in adolescence (19).
Despite advances in neonatal care, which resulted in a decrease in morbidity, limited progress has been made in reducing mortality, which was our second most important outcome, related to earlier gestational age and lower birth weight. In general, prematurity constitutes the main cause of perinatal mortality in Colombia, with records of up to 24.2 % of cases (20), somewhat lower than our record, but with similarities, in that infection constituted the variable with the highest lethality (21).
These findings show only early neurodevelopmental findings, and although severe neurological sequelae can usually be diagnosed during the first year of life (22), there is a larger group of sequelae that require adequate follow-up for screening (7). There are differences in brain growth and development among children and adolescents born preterm (23); however, although most survivors are free of major disabling conditions, many more subtle conditions are now evident in survivors, and this is closely related to the degree of immaturity at birth (24), including learning disabilities and visual and hearing impairments (25).
The development of retinopathy is closely related to early exposure to high amounts of oxygen; however, the frequency of ROP reported was almost nil, contrary to other publications, where an alteration has been reported, especially in the very low weight preterm baby and higher incidence at lower gestational weeks (26). These findings could be explained by adequate control of oxygenation limits, among other interventions. Wide fluctuations in oxygen saturation are most associated with an increased risk of severe ROP. According to its severity, it can cause severe visual impairment, and moderate forms regress with little or no impairment of visual function; but more severe forms can cause loss of visual acuity and even blindness (27).
The use of surfactant decreased the need for invasive mechanical ventilation. Overall, the results show a substantial reduction in mortality and respiratory morbidity (28). Noninvasive methods of ventilation were used more frequently in infants who did not develop BPD; consequently, these types of therapies could be considered with the clinical goal of reducing BPD, despite the variability in published results (29).
Maternal steroid administration was not found to be associated with a lower incidence of BPD. Studies indicate benefits of corticosteroids in reducing the risks of perinatal death, neonatal death, moderate/severe RDS, intraventricular hemorrhage, necrotizing enterocolitis, need for mechanical ventilation, and systemic infections in the first 48 hours of life but not in chronic lung disease or in reducing neurodevelopmental delay in infancy (30).
Conclusions
The incidence of BPD in preterm infants younger than 32 weeks is high, and this constitutes the most important morbidity in this group, with a significant associated overall mortality. In terms of mortality, the probability of death in these newborns is explained by lower gestational age (<28 weeks), lower hemoglobin concentrations, greater need for transfusions, and the presence of septic shock.











 text in
text in