Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
International Journal of Psychological Research
versão impressa ISSN 2011-2084
int.j.psychol.res. vol.7 no.1 Medellín jan./jun. 2014
Psychosocial Functioning in the Elderly: An Assessment of Self-concept and Depression
Funcionamiento Psicosocial en los Ancianos: Una Evaluación del Autoconcepto y la Depresión
Nicci Gracea,*, and Samia R. Toukhsatia,*
a Department of Cardiology, Austin Health, Heidelberg, Australia.
* Corresponding author: Samia, R. Toukhsati, Department of Cardiology, PO Box 5555 Heidelberg VIC. 3084 Australia. Tel: +61 3 9496 3209 FAX: +61 3 9496 5869. Email address: samia.toukhsati@austin.org.au
ARTICLE INFO
Article history: Received: 01-10-2013 Revised: 12-03-2014 Accepted: 20-03-2014
ABSTRACT
The aim of this study was to explore the relationship between self-concept and depression in elderly people living in Residential Aged Care (RAC) settings. Forty-five residents, comprising 17 males and 28 females (M = 82.64 years, SD = 8.38 years), were recruited from 10 low-care, RAC facilities in Melbourne, Australia. Participants completed the Geriatric Depression Scale - Short Form and the Tennessee Self Concept Scale: 2. The results revealed that all self-concept domains were significantly lower in RAC residents in comparison to norms drawn from community dwelling samples (p < 0.05). Moreover, a significant inverse relationship between depression and self-concept domains (p < 0.05) was observed in RAC residents, with 28.8% of the variance in depression scores accounted for by Physical Self Concept. These findings identify self-concept, particularly physical self-concept, as an important predictor of psychosocial well-being in elderly RAC residents. Further research is needed to examine the efficacy of psychosocial and rehabilitative interventions to optimise self-concept in RAC residents.
Key words: Depression; Self-concept; Quality of Life; Residential Aged Care; Psychosocial functioning.
RESUMEN
El objetivo de este estudia fue explorar la relación entre el autoconcepto y la depresión en las personas de edad avanzada que residen en residencias destinadas al cuidado de este tipo de personas. Cuarenta y cinco residentes de esta clase de residencias de bajo cuidado en Melbourne, Australia, 17 hombres y 28 mujeres, (M = 82.64 anos, SD = 8.38 anos) fueron incluídos. Los participantes completaron la forma corta de la escala de depresión geriátrica y la escala de autoconcepto de Tennessee: 2. Los resultados revelaron que todos los items relacionados al autoconcepto fueron significativamente bajos en las residencias mencionadas en comparación a las medias de muestras de habitantes de casas particulares (p < 0.05). Además, una relación inversa y significativa entre la depresión y el autoconcepto (p < 0.05) fue observado en los residentes del primer tipo de vivienda mencionada, con un 28.8% de varianza en los puntajes de depresión obtenidos para el autoconcepto físico. Estos hallazgos identifican el autoconcepto, particularmente el físico, como un importante síntoma de bienestar psicológico en los adultos mayores de residencias especiales destinadas a su cuidado. Es necesaria investigación posterior para examinar la eficacia de las intervenciones de rehabilitación y psicosociales para optimizar el autoconcepto en este tipo de población.
Palabras clave: Depresión, Autoconcepto, calidad de vida, residencies para el cuidado del adulto mayor, funcionamiento psicosocial.
1. INTRODUCTION
Emotional well-being is vulnerable to changes in an individual's social and physical environment and reports of poor emotional functioning in Residential Aged Care (RAC) residents are not uncommon (Antonelli, Rubini & Fassone, 2000; Davidson, McCabe, Knight & Mellor, 2012). In part, losses in quality of life domains, such as physical health, that often precede the transition to RAC likely contribute to mental health disturbance. In addition, the transition to RAC may be accompanied by a loss of social roles (Aitken, 1982; Shu, Huang, & Chen, 2003) and residents may experience social isolation and dislocation from their families, friends and the community to which they had previously belonged (Antonelli, et al., 2000; Bernoth, Dietsch & Davies, 2012). These factors are associated with, and may contribute towards, an increased vulnerability to the development of depression (Browning, Wells & Joyce, 2005).
Depression is a treatable, yet disabling, disorder that constitutes one of the most significant health issues among the elderly (Davidson et al., 2012). In addition, vulnerability to depression is often intensified within the RAC environment (Almeida & Almeida, 1999; Snowdon & Fleming, 2008). The incidence of depression is reported to range from approximately 9 to 50%, depending on the severity of depression specified (major or minor), the type of RAC (low or high level care) and the cognitive status of residents (George et al., 2007; McCabe, et al., 2006). Although there is some contention as to the prevalence of depression amongst RAC residents, in part due to the use and interpretation of different measures of depression, there is consensus that depression is a significant constraint to well-being in this cohort (Davidson et al., 2012).
Depression is highly correlated with quality of life (McCrae, et al., 2005) and bi-directionally correlated with self-concept (Almeida & Quintão 2012; de Gracia Blanco, Olmo, Arbones, & Bosch, 2004). Research has reported that, in addition to the high prevalence rates of depression and suicide ideation among RAC residents (Malfent, Wondrak, Kapusta, & Sonneck, 2010), negative self-conceptions are significantly higher in this cohort than in elderly people living independently (Antonelli, et al., 2000; de Gracia Blanco, et al., 2004). It should, however, be emphasised that depression is not known to be necessary or sufficient for the formation of a negative self-concept or vice versa. Rather, while deficiencies in one domain tend to predict deficiencies in other aspects of psychosocial functioning, causal explanations remain elusive. Nonetheless, maintenance of a positive self-concept is positively correlated with quality of life and well-being (de Gracia Blanco, et al., 2004; Shu, et al., 2003). As proposed by Markus and colleagues (Markus & Kunda, 1986; Markus & Herzog, 1991), self-concept is inherently implicated in all aspects of psychological experience and, consequently, influences inter- and intra-personal behavior and functioning. Thus, self-concept acts as a significant mediator of the personal aging experience (Shu, et al., 2003).
Research suggests that the self-concept becomes increasingly differentiated and multifaceted with age (Freund & Smith, 1999a, 1999b; Herzog, Franks, Markus, & Holmberg, 1996; Herzog & Markus, 1999; Marsh & Ayotte, 2003). This is likely due to increased life-experiences in a variety of social roles and situations (Atchley, 1991); the more multifaceted an individual's self-concept, the more resilient the person becomes in withstanding external social pressures (Atchley, 1991; Herzog & Markus, 1999).
Research has confirmed that a multifaceted self-concept contributes to increased emotional well-being and protects against depression (Freund & Smith, 1999a; Herzog, et al., 1996) by compensating for losses and impairments. However, as health-related losses and constraints intensify, the self-concept may become increasingly eroded and unstable (Freund & Smith, 1999a). As a person ages, the degree of importance placed on various aspects of the self are adjusted to reflect changes in capabilities and areas that are most vulnerable to age-related changes (such as increasing focus on maintaining health and independence) (Atchley, 1991; Freund & Smith, 1999a; McCrae & Costa, 1988). In circumstances when there is an accumulation of losses disproportionate to gains, this imbalance may undermine the stability of the self (Freund & Smith, 1999a). Therefore, it is unsurprising that RAC settings, which tend to represent losses in these valued domains, can often be perceived in a negative manner (Aitken, 1982; Antonelli, et al., 2000; Shu, et al., 2003).
Research has shown that RAC residents tend to have more negative self-conceptions than their community dwelling counterparts (Antonelli et al., 2000). de Gracia Blanco et al. (2004) found that Spanish RAC residents had higher rates of depression, lower self-concept and reduced psychological well-being in comparison to a community dwelling elderly sample.
The primary aim of this pilot study is to extend this literature base by examining self-concept evaluations in elderly people living in Australian RAC settings. A secondary aim is to explore the relationship between depression and self-concept in the elderly. In line with previous research, it is hypothesised that elderly participants living in RAC will possess significantly more negative self-conceptions compared to adult normative data. Further, it is hypothesised that self-concept will be negatively correlated with depression.
2. METHOD
2.1. Participants
Participants were recruited from a pool of 145 residents from 10 low-care (RAC) facilities in Melbourne, Australia, whom Directors of Nursing had identified as having the capacity to consent for themselves and to have lived at the facility for a minimum of three weeks. Directors of Nursing excluded individuals diagnosed with dementia or delirium and those legally blind or severely hearing impaired. Of these, 64 indicated their consent to participate in the study. With two exceptions, all participants scored > 24 on the Standardised Mini-Mental State Examination (S-MMSE) (Molloy, Alemayehu, & Roberts, 1991). Two participants scored between 20 and 23 on the S-MMSE and also scored 5 on the Geriatric Depression Scale; they were retained in order to accommodate any cognitive impairment associated with depression (Belsky, 1990). A total of 45 participants, including 17 males and 28 females (M = 82.64 years, SD = 8.38 years) were selected for inclusion.
2.2. Materials
Geriatric Depression Scale - Short form (GDS-S): The GDS-S (Sheik & Yesavage, 1986) is a 15-item, non-diagnostic index of depression for the elderly, as defined by the International Classification of Disease, 10th Edition and Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria (Almeida & Almeida, 1999). The GDS-S comprises items from the original GDS 30-item scale that have the highest correlations with depressive symptoms (Almeida & Almeida, 1999): these forms have a correlation of .84 (Lesher & Berryhill, 1994). Example items on the GDS-S include, "Are you basically satisfied with your life?" and "Do you think your life is empty?" to which respondents answer either "yes" or "no". Test administration takes an average of 5-7 minutes. The GDS-S has a possible score range of 0 to 15 and scores > 5 may indicate depression (Snowdon & Fleming, 2008).
Tennessee Self-Concept Scale: 2 (TSCS: 2) Adult Form: The TSCS: 2 is a standardised measure of self-concept suitable for individuals aged 13 to 90 years (Fitts & Warren, 1996). The TSCS: 2 comprises 82 self-descriptive statements rated on a 5-point Likert-type scale (where 1 = 'always false' and 5 = 'always true'). Due to the advanced age of participants, the question 'I treat my parents as well as I should' was changed to 'I treat(ed) my parents as well as I should'.
Six subscales are generated from 74 items: Physical (e.g., 'I have a healthy body'); Moral (e.g., 'I am satisfied with my moral behavior'); Personal (e.g., 'I am not the person I would like to be'); Family (e.g., 'I am satisfied with my family relationships'); Social (e.g., 'I do not feel at ease with other people'), and; Academic/Work (e.g., 'I am not as smart as the people around me'). Combined, these six subscales form a Total Self-Concept score.
The TSCS: 2 also comprises three Supplementary scores drawn from a specified combination of items from within the six subscales. These include Identity (e.g., 'I am a cheerful person'), Satisfaction (e.g., 'I don't feel as well as I should') and Behavior (e.g., "I have trouble doing the things that are right").
The TSCS: 2 Adult Form was standardised on individuals aged 19-90 years (n = 786). Normative scores are provided in the form of T scores (M = 50, SD = 10) for each scale. The TSCS: 2 Adult form has strong internal consistency with coefficient alphas ranging from 0.81 to 0.95 and strong test-retest reliability estimates ranging from 0.62 to 0.82 over a one to two week test-retest interval (Fitts & Warren, 1996).
2.3. Procedure
RAC facility recruitment: Following approval from the Monash University Standing Committee on Ethics in Research using Humans, residents identified by Directors of Nursing as meeting inclusion criteria were invited to participate. Consenting participants (N = 64) were administered the GDS-S and S-MMSE. Within each RAC facility, provided that S-MMSE scores > 20, participants were ranked according to their GDS-S scores (to prioritise high scorers) and invited to participate in the testing phase until a maximum of five participants per RAC were recruited.
General testing method: On the day following administration of the GDS-S and the S-MMSE, the TSCS: 2 was administered. Participants were requested to complete the TSCS: 2 in their own time. However, if assistance was required (commonly due to illiteracy, vision impairment and/or confusion), the measure was administered as an interview.
3. RESULTS
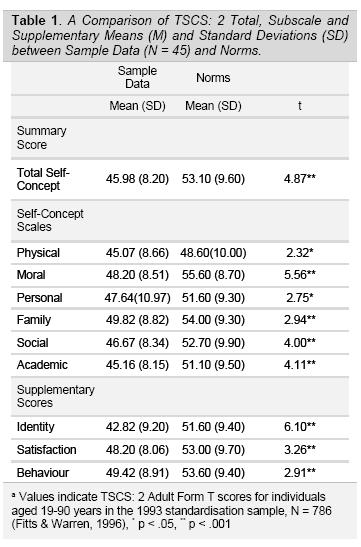
Descriptive statistics (means and standard deviations) for the TSCS: 2 Total, Subscale an Supplementary scores are presented in Table 1. There were no significant differences between males and females on any of the self-concept domains (p > 0.05).
The results presented in Table 1 show that all TSCS: 2 sample data means were significantly lower than norms (p < 0.05). The Holm-Sidák method was applied to correct for multiple comparisons.
3.1. Self-concept and depression
Scores on the GDS-S ranged between 0 to 11 with a mean of 4.56 (± 3.01) and 44.6% of the sample scored > 5. There were no significant differences between males and females on GDS-S scores (p > 0.05). The corresponding Pearson's r correlation coefficient matrix between the GDS-S and the TSCS: 2 is presented in Table 2.
Table 2 revealed a significant negative correlation between depression scores and all of the self-concept scales. A significant Backwards Linear Regression model (F(2,42) = 9.88, p < 0.001) revealed that Physical self-concept accounted for 28.8% of the variance in depression scores.
4. DISCUSSION
The primary aim of this pilot study was to examine self-concept evaluations in elderly participants residing in Australian RAC settings. The results revealed that all TSCS: 2 self-concept domains were significantly lower for elderly RAC residents in comparison to norms (Fitts & Warren, 1996). These results support those of Antonelli et al. (2000) and de Gracia Blanco et al. (2004) who determined that negative self-concept evaluations were prevalent in a European RAC context. Moreover, the findings are consistent with those of Davidson et al. (2012), who found that losses in personal autonomy (such as reduced resistance to normative pressure) were an important predictor of depression in elderly RAC residents.
The secondary aim of this study was to explore the relationship between depression and self-concept in elderly Australian RAC residents. Consistent with past research (de Gracia Blanco, et al., 2004), the results confirmed that all self-concept TSCS: 2 subscales were negatively correlated with depression. This suggests that all self-concept domains (physical, moral, personal, family, social and academic) are critically implicated in mood and well-being; this is consistent with recent research that has linked physical (Hsu & Lu, 2013) and health (Chang-Quan et al., 2010) self-concept to mental health and well-being in older adults. Whether vulnerability in these domains predisposed individuals to require RAC or, alternatively, developed in the context of the RAC environment is not clear from these cross sectional data; further longitudinal study is required to interrogate causal factors.
Results from this pilot study confirm that self-concept is a critical factor in need of addressing within the RAC context. Given that the current sample was limited to RAC residents, it would be worthwhile to compare these results to a community dwelling elderly sample to determine whether negative self-concept evaluations were intensified within the RAC environment. Once this was established, further research may be more able to examine ways in which the self-concept is restructured in later life and how this influences self-concept evaluation.
Given the capacity for self-concept change and its relationship to well-being and depression (both of which appear to be vulnerable within an RAC context), it may be appropriate to identify interventions that optimise and enhance self-concept in RAC settings. Many interventions seeking to enhance well-being (by enhancing positive affect and decreasing depression) in RAC contexts tend to be social in nature; the extent to which such interventions may have self-concept benefits remains a subject for empirical investigation.
5. LIMITATIONS
One of the limitations of this pilot study was related to the participant recruitment process. A non-random sample was employed to maximise the number of depressed participants recruited, which may limit the generalizability of the findings. Future research that recruits all cognitively intact elderly residing in RACs, regardless of depression severity, and includes a community dwelling sample, would be worthwhile.
6. CONCLUSION
Depression is a significant mental-health problem in the elderly. In RAC environments, where age-related losses are often intensified, depression is particularly prevalent (Davidson et al., 2012; Snowdon & Fleming, 2008). Our results suggest that self-concept is significantly eroded in elderly RAC residents and that this is linked with poor mental health, such as depression. Further empirical research is required to advance understanding of the self-concept and provide novel insight into the way individuals negotiate the aging experience. In view of empirical evidence supporting the capacity for self-concept change (Markus & Kunda, 1986), particularly in response to significant environmental changes, further research is needed to examine the means by which self-concept might be optimised in order to promote well-being. One such method might be to introduce social interventions that provide opportunities for purpose and mastery (Davidson et al., 2012), which have proven successful in enhancing mood and quality of life in the past.
7. ACKNOWLEDGEMENTS
We gratefully acknowledge the research support of Ms Leila Greenfield, Dr Jenny Patterson, Mr Daniel Condon, Ms Julia Lee and Ms Aimee Maxwell. We also gratefully acknowledge the support of the Residential Aged Care facility residents and staff for their participation.
8. FUNDING
This work was supported by the ANZ Trustees JO & JR Wicking Trust (Grant Number: CT 9048).
9. REFERENCES
Aitken, M. J. (1982). Self-concept and functional independence in the hospitalized elderly. The American Journal of Occupational Therapy, 36(4), 243-250. [ Links ]
Almeida, O. P., & Almeida, S. A. (1999). Short versions of the Geriatric Depression Scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. International Journal of Geriatric Psychology, 14, 858-865. [ Links ]
Almeida, L. & Quintão, S. (2012). Depression and suicidal ideation in elderly institutionalized and non-institutionalized in Portugal. Acta Médica Portuguesa, 25(6), 350 -358. [ Links ]
Antonelli, E., Rubini, V., & Fassone, C. (2000). The self-concept in institutionalized and non-institutionalized elderly people. Journal of Environmental Psychology, 20(2), 151-164. [ Links ]
Atchley, R. C. (1991). The influence of aging or frailty on perceptions and expressions of the self: Theoretical and methodological issues. In J. E. Birren, J. E. Lubben, J. C. Rowe, & D. E. Deutchman (Eds.), The concept and measurement of quality of life in the frail elderly (pp. 207-225). San Diego, CA: Academic Press. [ Links ]
Baltes, M. M., Wahl, H.W., & Reichert, M. (1992). Successful aging in long-term care institutions. Annual Review of Gerontology and Geriatrics, 11, 311-337. [ Links ]
Belsky, J. K. (1990). The Psychology of Aging: Theory, Research, and Interventions. (2nd ed.). Belmont, California: Brooks/Cole Publishing Company. [ Links ]
Bernoth, M.A., Dietsch, E., & Davies, C. (2012). Forced into exile: the traumatising impact of rural aged care service inaccessibility. Rural Remote Health, 12:1924. [ Links ]
Browning, C., Wells, Y., & Joyce, A. (2005). The experience of ageing: Influences on mental health and well-being. In V. Minichiello & I. Coulson (Eds.), Contemporary Issues in Gerontology: Promoting Positive Ageing (pp. 53-77). Crows Nest, NSW: Allen and Unwin. [ Links ]
Chang-Quan, H., Xue-Mei, Z., Bi-Rong, D., Zhen-Chan, L., Ji-Rong, Y., & Qing-Xiu, L. (2010). Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing, 39(1), 23-30. [ Links ]
Davison, T.E., McCabe, M.P., Knight, T., & Mellor, D. (2012). Biopsychosocial factors related to depression in aged care residents. Journal of Affective Disorders, 142(1-3), 290-6. [ Links ]
de Gracia Blanco, M., Olmo, J. G., Arbones, M. M., & Bosch, P. M. (2004). Analysis of self-concept in older adults in different contexts: validation of the Subjective Aging Perception Scale (SAPS). European Journal of Psychological Assessment, 20(4), 262-274. [ Links ]
Fitts, W. H. & Warren, W. L. (1996). Tennessee Self-Concept Scale: TSCS:2. (2nd ed.). U.S.A: Western Psychological Services. [ Links ]
Freund, A. M., & Smith, J. (1999a). Content and function of the self-definition in old and very old age. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 54B(1), 55-67. [ Links ]
Freund, A. M., & Smith, J. (1999b). Methodological comment: Temporal stability of older persons' spontaneous self-definitions. Experimental Aging Research, 25, 95-107. [ Links ]
George, K., Davison, T. E., McCabe, M., Mellor, D., & Moore, K. (2007). Treatment of depression in low-level residential care facilities for the elderly. International Psychogeriatrics, 19(6), 1153-1160. [ Links ]
Herzog, A. R., Franks, M. M., Markus, H. R., & Holmberg, D. (1996). Age differences in temporal orientation of the self: Current, past and possible selves. In Proceedings from the 14th Biennial Meeting of the International Society for the Study of Behavioral Development, Quebec City. [ Links ]
Herzog, A. R., & Markus, H. R. (1999). The self-concept in life span and aging research. In V. L. Bengston and K. W. Schaie (Eds.), Handbook of theories of aging (pp. 227-252). New York: Springer. [ Links ]
Hsu, Y-W., & Lu, F. J-H. (2013). The development and validation of the physical self-concept scale for older adults. Educational Gerontology, 39(7), 501-513. [ Links ]
Lesher, E. L., & Berryhill, J. S. (1994). Validation of the Geriatric Depression Scale-Short Form among inpatients. Journal of Clinical Psychology, 50, 256-260. [ Links ]
Malfent, D., Wondrak, T., Kapusta, N.D., & Sonneck, G. (2010). Suicidal ideation and its correlates among elderly in residential care home. International Journal of Geriatric Psychiatry, 25(8), 843 -849. [ Links ]
Markus, H., & Kunda, Z. (1986). Stability and malleability of the self-concept. Journal of Personality and Social Psychology, 51(4), 858-866. [ Links ]
Markus, H. Z., & Herzog, A. R. (1991). The role of the self-concept in aging. Annual Review of Gerontology and Geriatrics, 11, 110-143. [ Links ]
Marsh, H. W., & Ayotte, V. (2003). Do multiple dimensions of self-concept become more differentiated with age? The differential distinctiveness hypothesis. Journal of Educational Psychology, 95(4), 687-706. [ Links ]
McCabe, B. W., Davidson, T. E., Mellor, D., George, K., Moore, K., & Ski, C. (2006). Depression among older people with cognitive impairment: Prevalence and detection. International Journal of Geriatric Psychiatry, 21, 633-644. [ Links ]
McCrae, N., Murray, J., Banerjee, S., Huxley, P., Bhugra, D., Tylee, A., & Macdonald, A. (2005). 'They're all depressed, aren't they?' A qualitative study of social care workers and depression in older adults. Aging & Mental Health, 9(6), 508-516. [ Links ]
McCrae, R. R., & Costa, P. T. (1988). Age, personality and the spontaneous self-concept. Journal of Gerontology: Social Sciences, 43B, S177-S185. [ Links ]
Molloy, D. W., Alemayehu, E., & Roberts, R. (1991). Reliability of a Standardised Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. American Journal of Psychiatry, 148, 102-105. [ Links ]
Sheik, J. A., & Yesavage, J. A. (1986). Geriatric Depression Scale (GDS). Recent development of a shorter version. Clinical Gerontology, 5, 165-173. [ Links ]
Shu, B.-C., Huang, C., & Chen, B.C. (2003). Factors related to self-concept of elderly residing in a retirement center. Journal of Nursing Research, 11(1), 1-7. [ Links ]
Snowdon, J., & Fleming, R. (2008). Recognising depression in residential facilities: An Australian challenge. International Journal of Geriatric Psychiatry, 23, 295-300. [ Links ]