1. Introduction
Pediatric bipolar disorder (PBD) has a worldwide prevalence of 1.8% (Van Meter, Moreira, & Youngstrom, 2011), it appears at an early age and has repercussions at academic, family and interpersonal levels (Birmaher et al., 2006). The relationship between PBD and bipolar disorder (BD) has been established not only by retrospective and prospective studies, but also by genetic studies (studies in families, twins and adoption), which demonstrate high heritability (McGuffin et al., 2003). PBD is a highcost disorder with high risk for suicide; therefore, it is relevant to explore the underlying pathophysiological mechanisms and their correlation with clinical variables (Axelson et al., 2015; Goldstein et al., 2013).
The anterior limbic network is involved in the regulation of emotions, affection, and cognition (Emsell & McDonald, 2009; Strakwowski et al., 2012). A possible dysfunction in this network has been suggested as a potential pathophysiology of BD and PBD (Pfeifer, Welge, Strakowski, Adler, & DelBello, 2008). Some neuroimaging studies in adults with BD show increased volume of the lateral ventricles (Strakwowski et al., 2012), hyperintensities in white matter (Frey et al., 2013; Lenox, Gould, & Manji, 2018), and neuroanatomic changes mainly in the anterior limbic network. However, not all of these findings have been replicated (Houenou et al., 2011; Kempton, Geddes, Ettinger, Williams, & Grasby, 2008). Some structural changes occur from the first episodes of mania in young adults, for instance, the smaller volume of the amygdala found in BD studies (Hajek, Kopecek, et al., 2009; Rosso et al., 2007) has been replicated in the PBD population (K. Chang et al., 2005; DelBello, Zimmerman, Mills, Getz, & Strakowski, 2004; Dickstein et al., 2005; Frazier et al., 2005; Wilke, Kowatch, DelBello, Mills, & Holland, 2004). However, it is still necessary to evaluate whether there are other anatomical changes even before the first episode.
Bipolar offspring (BO), compared to community controls offspring (CCO), is a population at a higher risk to present bipolar spectrum disorder (OR=14) or any psychiatric disorder (OR=2-3) (Axelson et al., 2015; Birmaher et al., 2009; Duffy, Jones, Gooday, & Bentall, 2015). On one side, some neuroimaging studies in BO show a compromise of the fronto-limbic neural network: increase of right amygdala (Bauer et al., 2014), decrease in left orbitofrontal cortex region and right cerebellum, dorsolateral prefrontal cortex (DLPFC), increased gray matter at the left parahippocampal, left hippocampal gyrus (Ladouceur et al., 2008), and reduced striatal volume (Lancaster, 2018). In addition, volumetric increased had been reported in the white matter at the middle and inferior frontal gyrus, at middle and inferior temporal (Nery et al., 2017), amygdala (Karchemskiy et al., 2011; Kelley et al., 2013; Ladouceur et al., 2008; Singh, DelBello, Adler, Stanford, & Strakwowski, 2008), orbito medial prefrontal cortex (Ladouceur et al., 2008), cingulate, temporal lobe (Bauer et al., 2014), hippocampal region (Bauer et al., 2014; Karchemskiy et al., 2011), corpus callosum (Walterfang et al., 2009), striatum (Singh et al., 2008), or subgenual cingulate (Hajek, Gunde, et al., 2008). In this regard, several authors agree that these mentioned studies showed inconsistent findings, had small samples, used different definitions for “symptomatic or asymptomatic”, and not all of them included a comparison group (Nery, Monkul, & Lafer, 2013).
The aim of the present study was to find out brain volumetric differences between BO group compared with CCO group. Descendants of parents within the “paisa”1 population were studied, since it is an ethnic group with a high prevalence of BD type I, and it has previous studies on inheritable endophenotypes for BD (Fears et al., 2015, 2014)
2. Materials and methods
2.1 Participants
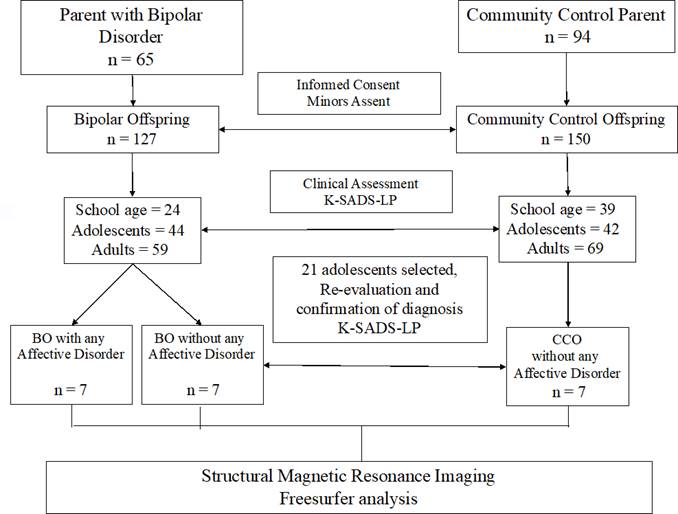
An observational, descriptive, cross-sectional, exploratory study was conducted with multiple comparison groups. The “top-bottom” methodology was followed, which first defines BD parent diagnosis, and then studies its offspring. Inclusion criteria for BD parents were: having BD type I by diagnostic interview for genetic studies (DIGS), having at least one psychiatric hospitalization before age 50, and absence of any organic disorder that could be confused with BD. The parent control group was taken from the same geographical area, with these inclusion criteria: no personal or first-degree relative history of BD, schizophrenia or any psychotic disorder. A sample of twenty-one adolescents was obtained from a previous comparison study of one hundred and twenty-seven BO versus one hundred and fifty CCO (Palacio-Ortíz et al., 2015; Palacio-Ortiz et al., 2017b, 2017a). All those subjects between 10 and 18 years old were invited to participate. Figure 1 shows the collecting sample flowchart.
The sample was constituted by three groups: BO with AD, BO without AD, and CCO. Initially, BO with AD was defined as those BO with a life time affective disorder, either major depressive disorder (MDD), mania or hypomania. Adolescents diagnosis were obtained by the Diagnostic Interview for Affective Disorders and Schizophrenia in Children and Adolescents, Present and Longitudinal version ([K-SADS-PL] Kaufman et al., 1997; Ulloa-Flores et al., 2006). The first step was to gather seven BO with AD, and then matching groups gyrus, precuneus, and a caudate volume (Hajek, Gunde, et al., 2008, 2009b). On the other side, some BO studies have not found volumetric differences in white matter were selected considering age, gender and Tanner stage. The subjects belonging to the groups BO without AD and CCO could present any type of psychopathology except MDD, mania or hypomania. Exclusion criteria for the subjects of the three groups were intellectual disability, autistic spectrum disorders, carrying metal pacemakers or prosthetic limbs, brackets, hydrocephalus history, central nervous system surgery, moderate or severe cranial brain trauma, history of structural or degenerative neurological lesions, and epilepsy.
2.2 Instruments
2.1.1 K-SADS-PL
This semi-structured interview evaluates the presence of a psychiatric disorder according to the DSM-5, during the present and in the past (Kaufman et al., 197AD). It also includes the Children’s Global Assessment Scale ([CGAS] Shaffer et al., 1983), which assesses the performance level on a scale from zero to 100 points (lower scores indicate a greater compromise of functionality). The K-SADSPL was translated into Spanish and has an inter-rater reliability rating from good to excellent (de la Peña et al., 2018; Ulloa-Flores et al., 2006).
2.2.2 DIGS
This diagnostic interview was developed for genetic studies of schizophrenia and affective disorders, and takes into account diagnostic criteria based on DSM-5 (American Psychiatric Association, 2013). It was translated and validated for Colombia and has high reliability test-reporter as well as inter-evaluator (Palacio et al., 2004).
2.2.3 Anthropometric Measurements and Tanner Stage
The values of weight, height and cephalic perimeter were taken by medical personnel. Tanner stage was determined by self-report, taking into account mammary development in women using images of the different stages; in males, the testicular size using the Prader orchidometer (Carel & Leger, 2008; Marshall & Tanner, 1969, 1970). Pubic hair was a complementary measure, and in case of obtaining different stage between both measurements, Tanner stage was defined according to the mammary development or the testicular size.
2.3 Procedures
The research protocol was approved by the Ethics Committee of the Medical Research of the Center, Faculty of Medicine from the University of Antioquia, and by the Ethics Committee of the University Hospital of San Vicente Fundación. Initially, the parents (from both groups: BD and controls) were evaluated, and their offspring were subsequently selected according to the inclusion criteria. After explaining the project, all the parents signed an informed consent and the participants signed a minor assent. The group coordinator selected the adolescent subjects for this study. A psychiatrist with previous training conducted the DIGS and K-SADSPL interviews. The evaluators were blind to the parent diagnoses. All data were taken from direct interview with adolescents and with at least one of their parents. In order to corroborate the offspring’s psychiatric status, a procedure of “best estimate” was carried out by two child psychiatrist experts. Magnetic resonance imaging (MRI) was performed the day after the interview.
2.3.1 MRI Methods
MRI acquisition parameters.
MRIs were performed at the Instituto de Alta Tecnología Médica (IATM), and the technical staff verified the quality throughout the neuroimage acquisition process. Subjects were asked to remain still and a constant accompaniment was made during MRI. A 3 Teslas Philips Ingenia resonator was used to acquire a T1-weighted volumetric sequence. Sequence parameters were: voxel size: 0.7 × 0.7 × 0.7mm3, Geometry: sagittal, FOV=256mm (matrix of 384 × 384), and a 0.7mm thick.
2.3.2. MRI Volumetry
A quality control was performed to ensure that MRIs did not have artifacts. The volumes of subcortical structures and cortical regions were calculated for every subject, using automatic segmentation algorithms from the Freesurfer analysis suite (Hospital, 2016). The Freesurfer work flow (Desikan et al., 2006) consisted of several steps. First, a register was made accordingly with the Talairach anatomical space, followed by an initial volumetric labeling or segmentation. Subsequently, a motion correction of the images in T1 and elimination of the non-cerebral tissue was carried out through a segmentation that excluded structures that were not of interest. Then, a subcortical volumetric segmentation was performed followed by an intensity variations correction of the image due to magnetic field inhomogeneities (“bias field correction”). After that, the white matter was segmented accordingly to the Desikan-Killiany surfaces atlas. Finally, brain surface and cortical segmentation was performed by a labeling based on brain´s gyri and sulci. Finally, volumetric measurements were normalized according to the intracranial volume of each subject.
Imaging processing was performed by one investigator (J.P.Z.) blinded to the diagnosis and group assignment. The following subcortical structures were measured for both hemispheres: thalamus, caudate, putamen, globus pallidum, hippocampus, amygdala, and nucleus accumbens. The cingulate for each hemisphere was divided into caudal anterior, rostral anterior, posterior, and isthmus. The frontal region for each hemisphere was divided into caudal middle, lateral orbitofrontal, medial orbitofrontal, pars opercularis, pars orbitalis, pars triangularis, rostral middle, superior, and frontal pole. Other measurements were bilateral cortex volume, subcortical gray matter volume, and total gray matter volume.
2.4 Statistical Analysis
A comparison was made between the different groups of subjects and the effect size was calculated with their respective 95% confidence interval. The magnitude of the differences between the groups was quantified (BO with AD versus BO without AD, BO with AD versus CCO, BO without AD versus CCO, BO versus CCO, BO with AD versus BO without AD + CCO) using the effect size measure: d Cohen’s (absolute) (Iraurgi, 2009). This measure shows the difference in standard deviations between study groups, for each brain structures volumes, without having the magnitude affected by the sample size. A p-value of less than 0.05 and an absolute value of effect size greater than 0.5 were considered significant. The systematization, processing and analysis of the data were performed using the programs Stata version 13 and Aabel 20/20 data vision 3.
For the descriptive analysis of socio-demographic and clinical features, we used absolute and relative distributions, and summary indicators such as arithmetic mean, standard deviation, median, and interquartile range. The criterion of normality and homoscedasticity of the brain structures was established through the Shapiro-Wilk and Levene tests. To control the effect of age differences between study groups, it was adjusted by covariance analysis and the homogeneity assumption of regression was evaluated. In order to explore possible relation between socio-demographic and clinical features for each study group, Chi square test of likelihood ratio, analysis of variance and Kruskal-Wallis test were used.
3. Results
3.1 Demographics
A sample of twenty-one subjects was obtained, seven subjects per group (see details in Table 1). After comparing social demographic characteristics among the three study groups, no statistically significant differences were found. All subjects in the BO with AD group had a MDD diagnosis (present or past). Two subjects in this group had BD type I (28.57%) and two other specified BD (OS-BD) (28.57%). The BO with AD group had a higher number of comorbidities as shown in Table 2. Attention deficit hyperactivity disorder (ADHD) is one of the most prevalent disorders in the three groups, even present in two subjects from the CCO group (28.6%). There is a tendency for the BO with AD group to have experienced with cigarettes, alcohol and substances. The BO with AD group had a lower functionality score than the other two groups as shown by their current CGAS (median score: 65 versus 80 and 91) and past CGAS (median score: 50 versus 70 and 81). None of the participants had pharmacological treatment 6 months prior to the MRI, and none of them presented experimental consumption of substance of abuse 6 months prior to MRI.
3.1 Volumetric Results
The main finding was obtained in the right rostral middle frontal region, where a greater volume in the BO with AD group was found compared to the other two groups (p = 0.041). By effect size analysis, a greater volume was found in the BO with AD group compared to the BO without AD group in the isthmus region of the right cingulate (d = 0.53), and the left pars opercularis region (d = 0.63), and also when compared to the CCO group in the right hippocampus (d = 0.53) (See Table 3).
The BO without AD group compared to the CCO group, had a lesser volume in the left anterior caudate (d = 0.6). When comparing the two BO groups (with and without AD) versus the CCO group, two findings were obtained (by effect size analysis): the BO groups showed a greater volume in the right frontal pole (d = 0.52), and a lesser volume of the right globus pallidum (d = 0.55). There were no volumetric differences in other brain regions, such as putamen, nucleus accumbens, or amygdala, when making other comparisons among groups.
4. Discussion
This is one of the first studies comparing brain volumes of BO versus CCO groups using the Freesurfer technique (Desikan et al., 2006). The current methodology allowed further comparisons of the BO subgroups, and it was found that the BO with AD group had a greater volume compared to the other two groups in the right rostral middle frontal, the right isthmus cingulate, the right hippocampus, and the left pars opercularis region. In addition, the two BO groups presented a larger volume in the right frontal pole region compared to the CCO group.
Neuroanatomical changes in the frontal areas could be related to BD. In this regard, findings at the frontal region have been referred by other authors. One study found a greater volume in the region of the right inferior frontal gyrus in the BO group (with and without AD) than in the CCO group (Hajek et al., 2013). Three other studies indicate differences in the frontal region. However, it was different in BO without AD compared to CCO: one found a higher cortical volume in the medial orbitofrontal region (Ladouceur et al., 2008); another a smaller volume in the right inferior orbitofrontal region and the right middle frontal (Falluca et al., 2011); and the last one found a small effect size difference showing a slightly larger volume in prefrontal cortex in the BO without AD group versus the CCO group (Singh et al., 2008).
The above mentioned is congruent with some findings in adults with BD. A recent meta-analysis comparing BD versus controls showed a involvement of frontal areas that exhibits reduce volumes of pars opercularis, fusiform gyrus and rostral middle frontal cortex (Hibar et al., 2018). Another adult study pointed out a decreased volume for the right medial frontal for subject with BD an also unaffected first-degree relatives of BD (Matsuo et al., 2012).
At some point, our findings at the prefrontal region in the BO group could be attributable to an affective disorder such as MDD, but it should be taken in to account that previous data in the frontal region from studies in adolescents with MDD is contradictory (Falluca et al., 2011). While one study found a larger volume in the dorsal middle frontal region (Reynolds et al., 2014), other studies indicated a smaller volume of the DLPFC (C. Chang et al., 2008; Khundakar, Morris, Oakley, McMeekin, & Thomas, 2009; Peterson et al., 2009). Therefore, BO with AD group current results in frontal region could be consider as attributable to the early manifestations of BD in this high-risk population. Previous BO population studies had not found volume differences at the cingulate (Bauer et al., 2014), nor the subgenual cingulate region (Hajek, Kozeny, Kopecek, Alda, & Hoschl, 2008; Hajek, Gunde, et al., 2009a). But in the present study, a lesser volume in the left anterior caudate cingulate was found in the BO without AD group versus the CCO group. In fact, this present finding is in the same direction as other PBD studies that have found a lesser cortex volume in the left anterior cingulate (Chiu et al., 2008; Kaur et al., 2005; Wilke et al., 2004), as well as studies of bipolar depression in young people (MacMaster, Langevin, Jaworska, Kemp, & Sembo, 2014). Nevertheless, the present result cannot be considered as an initial manifestation of BD, since it was not found in the BO with AD group.
Several structural and functional imaging studies in adults with BD indicate the key role of amygdala and hippocampus. In the PBD population a smaller volume of amygdala (Blumber et al., 2003; Blumberg et al., 2005; K. Chang et al., 2005; DelBello et al., 2004; Dickstein et al., 2005; Frazier et al., 2005; Wilke et al., 2004) and hippocampus (Bearden et al., 2008; Blumber et al., 2003; Blumberg et al., 2005; Frazier et al., 2005) has been consistently found. The same is not true for BO MRI studies. On one hand, there are only two studies in BO without psychiatric disorder that found a larger volume in the right amygdala (Bauer et al., 2014) and the left hippocampus (Ladouceur et al., 2008). On the other hand, there are other studies that have not found such differences comparing CCO versus BO in the amygdala (Karchemskiy et al., 2011; Ladouceur et al., 2008; Singh et al., 2008) nor in the hippocampus (Bauer et al., 2014; Karchemskiy et al., 2011). This present analysis showed a greater volume in the right hippocampus in BO with AD group versus BO without AD group. In this regard, a few studies on depression in adolescents show inconsistent results in the hippocampus and amygdala (MacMillan et al., 2013; Rosso et al., 2005; Van Eijndhoven et al., 2013), which is a data that does not allow to define if this last finding is better attributed to the antecedent of MDD or to the risk of BD in this population.
Table 1 Demographics variables
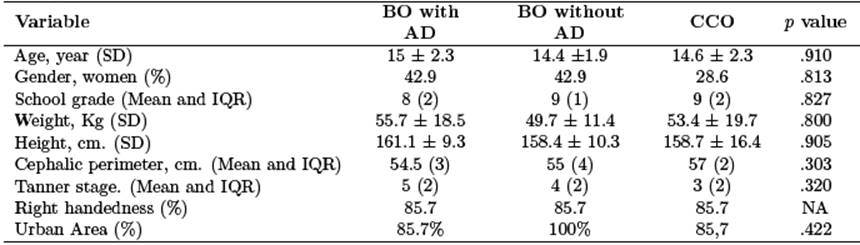
Note: n = 7; BO with AD: Bipolar Offspring with current or past history of affective disorder; BO without AD: Bipolar Offspring without a lifetime history of any affective disorder; CCO: Community Control Offspring; SD: standard deviation; IQR: interquartile range
Table 2 Clinical variables
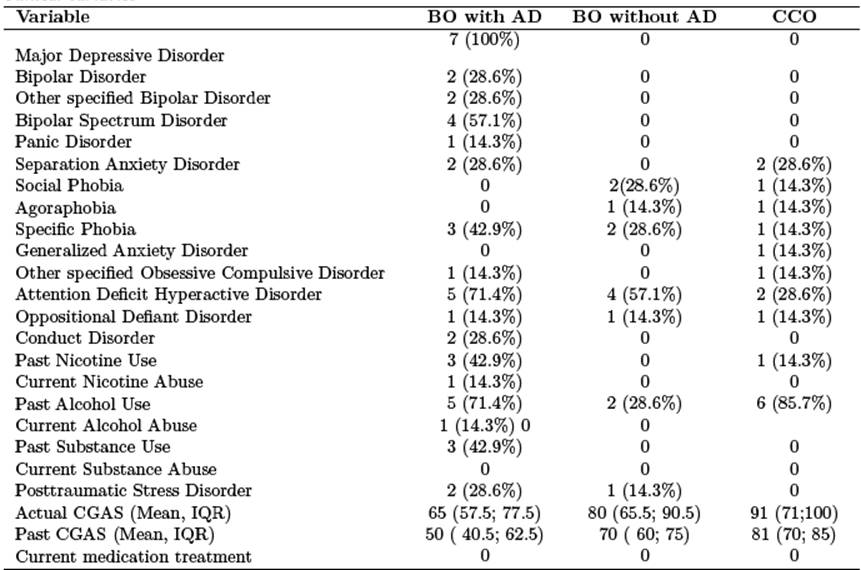
Note: n = 7; BO with AD: Bipolar Offspring with current or past history of affective disorder; BO without AD: Bipolar Offspring without a lifetime history of any affective disorder; CCO: Community Control Offspring; IQR: interquartile range; CGAS: Children’s Global Assessment Scale
In imaging studies is important to control other confounding factors, such as medications, drug use and prevalent comorbidities. In the present study the volumetric differences found out between groups were not influenced by the presence of psychotropic drugs or medications (none of the subjects took psychotropic medication or used drugs in the previous 6 months). However, we cannot rule out that some volumetric differences could be due to comorbidities such as ADHD, which involve nearby brain areas (Baroni & Castellanos, 2015; Krain & Castellanos, 2006; Liu et al., 2011).
Table 3 Comparison of normalized brain volumetry of frontal, cingulate and subcortical structures
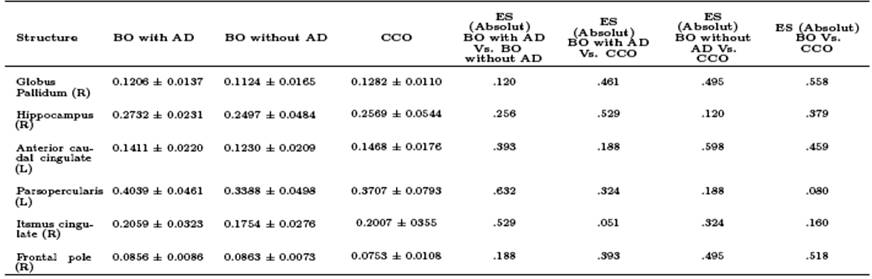
Note: n = 7; BO with AD: Bipolar Offspring with current or past history of affective disorder; BO without AD: Bipolar Offspring without a lifetime history of any affective disorder; CCO: Community Control Offspring; (L): Left. (R): Right; ES: Effect Size.
*ANCOVA adjusted by age.
Two neuroanatomical regions that could have their role as biological markers were found when comparing the CCO group with the two groups of BO: the right frontal pole (with greater volume in the BO) and the right globus pallidum (with lesser BO volume). A previous study of adult with BD and relatives from the “paisa region” showed a decrease in total brain volume, hippocampus, ventral diencephalon and corpus callosum, among other regions (Fears et al., 2015, 2014). Although in that study some findings pointed out similar regions to our study such as the cingulate and the middle frontal region, we cannot be considered this results as endophenotypes for two reasons: first, present methodology did not include MRI of parents, and second, our sample was constituted by adolescents that may have brains at different neurodevelopment stages (Casey, Jones, & Hare, 2008; Goddings et al., 2014).
The images quality provided by the Freesurfer MRI analysis is a strength of the present study; however, being a last generation technology, it decreases the possibility of making a direct comparison with volumetric studies prior to this technique (Fischi & Dale, 2000). Another strength is to analyze by effect size to increase the external validity of the study. Finally, a classification of the subjects was carried out in three study groups, which allowed to identify if the volumetric differences were associated to the BD or to the condition of bipolar descendent.
The authors acknowledge that one study limitation is sample size. In spite of this, an adequate control of the possible confounding factors was made. This is an exploratory study that delimited only subjects between 11 and 17 years old, which should be considered when extrapolating the data to other populations. “Paisa” population was studied, which increases the penetrance capacity of possible endophenotypes, but at the same time it makes our findings less comparable with other populations. Lastly, other studies with greater statistical power, that allow to extend and deepen these results, are required.
5. Conclusion
The present study was performed with the intention of finding volumetric differences in the frontolimbic neural network structures when comparing two groups of BO versus a CCO group. Significant differences were found in the right rostral middle frontal region, with a greater volume in the BO with AD group compared to the BO without AD group. Some further volumetric differences were found in the pars opercularis, isthmus, hippocampus, and anterior caudate cingulate regions. There are two anatomical regions that could be suggested as biological markers in this BO population: right frontal pole and right globus pallidum. More studies are needed in this population of high risk in order to improve accuracy and replicability of these findings.