1. Introduction
It is estimated that more than 1.9 billion people in the world suffer from some type of chronic painful condition (Mills et al., 2019), understood as that which recurs or persists for more than three months, causing a significant emotional or functional affectation (Treede et al., 2015). The nature of chronic pain is complex and its under-standing implies integrating dimensions of an organic and psychological nature, the efforts of multiple disciplines, such as psychology and neuroscience, which have added their knowledge to that of neurophysiology and branches of clinical application, to generate theoretical models with the objective of knowing the multidimensional nature of pain. Among these theories, the Multidimensional Model of Pain or Neuromatrix Theory (Melzack, 1996), the Fear Avoidance Model (Vlaeyen & Linton, 2000), the Neurocognitive Model of Attention to pain (Legrain et al., 2009), and, recently, the Dynamic Pain Connectome Model (Kucyi & Davis, 2015) have been emerging.
Although these models have approached the aspects of the emotional or cognitive experience associated with pain, they cannot satisfactorily explain the patients response to this experience, its chronicity, and the impact of pharmacological and non-pharmacological therapies on functionality for different chronic painful conditions. In this regard, the neurocognitive model of Selfregulatory Executive Functions has attracted interest (Wells & Matthews, 1996), which aims to associate the results of the sensory experience and illness with the cognitive processes and beliefs related to the experience of pain and the evaluation that the subject makes of them. This model integrates subjective elements the individual’s beliefs and their evaluations to the variables of daily impact of the patients, such as the intensity of pain and functional compromise.
The model considers that emotional processing is carried out through a system of three levels, which constantly interact with each other. The Processing Units are located At the lower level, which comprise the body’s sensory systems (both interoceptive and exteroceptive) and cognitive systems. At this level, which is characterized by being automatic and not very reflective, the information is channeled and the stimuli to which the attentional effort is intended are selected.
Ontheotherhand, attheintermediatelevel, self-regulationfunctionsarecarriedoutthroughpre-establishedplans that guide the monitoring of sensory systems. This level receives information from the cognitive processing units to analyze it, and is characterized by being reflective and with limited attention span (Reyes, 2015).
Finally, self-beliefs are located at the higher level, which can be declarative, corresponding to ideas, evaluations or judgments about oneself (Sierra, 2010); or procedural, which guide the way the individual gives a personal meaning to the stimuli and provides the general plan of the coping responses through the metacognitive processes. Both can be understood as “implicit plans that guide processing and operate largely outside of consciousness” (Wells, 2000, p. 19).
Recently, some authors have considered that this theoretical proposal may be useful for understanding the perceptual, cognitive-emotional, and behavioral responses in conditions of both acute and chronic pain (Kollmann et al., 2016; Spada et al., 2016; Yoshida et al., 2012). One of the main properties of this model is the integration into a single theoretical structure of the sensory elements of the painful experience and their links with the cognitive and self-regulation processes through beliefs. This is a characteristic that is absent in the other theoretical models, which have restricted themselves to mentioning these relationships without committing to a procedural structure.
Additionally, it has been proposed that its integrative capacity is what allows articulating the multiple evidences that relate the psychological aspects, physical deterioration, and intensity of pain with the cognitions associated with it in patients with fibromyalgia (Martínez et al., 2015; Peñacoba-Puente et al., 2015; Tirado et al., 2014). This condition has been defined as a syndrome of unknown origin that is characterized by the development of generalized pain, multiple tender points (points sensitive to pressure in muscle examination), in addition to other symptoms such as fatigue, muscle stiffness, and cognitive dysfunction (Wolfe et al., 2010). Its uncertain etiology raises multiple questions related to the diagnosis and treatment of this condition, but above all with the progressive deterioration in functionality and quality of life of approximately 2% of the world population that suffers from it (with a proportion of 4:1 between women and men), as well as in the strategies for reducing the impact on health systems (Cabo-Meseguer et al., 2017).
For these reasons, fibromyalgia could be considered as one of the pain syndromes that best meets the conditions for the study of chronic pain within the framework of the S-REF model. In fact, research on fibromyalgia suggests that psychological and cognitive variables can have a great influence on its progression and on its interference with daily activities (Luciano et al., 2014; Mobini et al., 2017; Vanhaudenhuyse et al., 2015).
Among these psychological and cognitive elements, the catastrophic evaluations oriented towards pain stand out (Loggia et al., 2015), which seem to be closely related to the emotional impact and reduction of the functionality of patients (Lami et al., 2018). Likewise, the perception of pain self-efficacy seems to mediate the impact of pain in daily life, the perception of pain and the anxiety manifested by patients with this syndrome (De Rooij et al., 2013; Lee et al., 2017). Additionally, the impact that beliefs about pain have on the coping processes, functionality, and emotional state of patients with the syndrome has gradually taken on greater interest (Kollmann et al., 2016; Kuppens et al., 2015), although this topic is still under development.
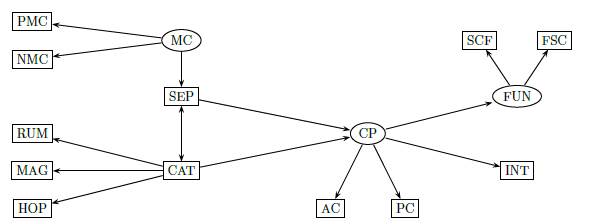
Given these questions about the nature of this syndrome, and based on the approaches and research antecedents on the role of cognitions related to pain, the present investigation is proposed with the purpose of determining the explanatory capacity of metacognitions about the control of symptoms, self-efficacy, and catastrophism towards pain, over the functionality, coping, and pain intensity, following the Model of Self-Regulation Executive Functions. Figure 1 shows the initial theoretical model that was proposed.
2. Method
2.1 Type of study
Analytical empirical study with a cross-sectional explanatory design with observable variables according to Ato et al. (2013), in which psychometric techniques were used to collect the information.
2.2 Sample
Non-random sampling, for convenience. The sample of participants consisted of 108 women, between 24 and 60 years old, residing in Medellín and its Metropolitan Area (Northwest Colombia), with a diagnosis of fibromyalgia given by a specialist doctor. Women with severe physical disability for any reason other than fibromyalgia, or with cognitive impairment that limited the responses to the instruments were excluded. The verification of these disabling conditions was carried out through the analysis of the clinical history provided voluntarily by the participants.
The collection of the sample was carried out through different procedures: 1. Invitation to participate made by some medical specialists in the field of pain in the city of Medellín and the metropolitan area; 2. Direct invitation to patients who required emergency consultation in a home health care institution in Medellín and the metropolitan area for pain control between June 2017 and June 2018; 3. Invitation to participate through a social assistance foundation in Medellín; 4. Invitation to participate through the mediation of other participants; and 5. Invitation on social networks and through a Facebook group, made up mainly of fibromyalgia patients from Medellín and its Metropolitan Area. The patients were summoned for a meeting that lasted around one hour. During the meeting, after the completion of the informed consent for the participation in the study, a review of the patient’s medical history was performed to confirm the diagnosis made by a doctor or specialist doctors.
2.3 Instruments
Metacognitions Scale about Symptom Control (MSC) (Fernie et al., 2015), designed to evaluate positive and negative metacognitions related to the control of the disease or its consequences. It consists of 17 items, which are answered according to a Likert scale of five response options and the degree is evaluated according to the subject. Regarding the internal consistency, a Cronbach’s alpha of .89 was obtained for Positive Metacognitions about Symptom Control (PMCS) and .88 for Negative Metacognitions about Symptom Control (NMCS) (Fernie et al., 2015).
Pain Self-efficacy Questionnaire (PSEQ), originally created by Nichollas in 1989 to assess the self-efficacy beliefs of patients with chronic pain conditions, consists of 10 items that inquire about the perception of selfefficacy that the subjects present to face different situations of personal, work, and social nature, as well as of their illness, related to their experience of pain. Each item is evaluated through a seven-point Likert scale ranging from 0 to 6, with 6 being the highest level of self-efficacy. The factoring analyses of the questionnaire establish a one-dimensional construct, with high levels of internal consistency, and a Cronbach’s alpha of .9 (Nicholas, 2007).
Pain Catastrophizing Scale (PCS) (Sullivan et al., 1995). Made up of 13 items that assess the degree to which the person has experienced a series of thoughts or feelings in past painful experiences, on a 5-point scale, where 0 means “not at all” and 4 “all the time”. It has shown a good level of internal consistency, with a Cronbach’s alpha of .86 (Suso-ribera et al., 2017).
Questionnaire about Facing Chronic Pain (QFCP; Soriano & Monsalve, 2005), which assesses the strategies for coping with chronic pain and is made up of 24 items that represent two dimensions of coping with pain: Passive Coping and Active Coping. The Passive Coping is made up of two factors: religious coping and the search for emotional support; while the Active Coping is made up of four factors: distraction, mental self-control, self-assertion, and search for instrumental social support. Each of the items assesses the degree of agreement on a 5-point Likert scale. The rates of internal consistency of each of the factors, measured through the Cronbach’s alpha, are .94, .88, .82, .81, .79, and .77, respectively (Soriano & Monsalve, 2005). This scale has been validated for patients with fibromyalgia with similar results of internal consistency (Soucase et al., 2004; Vázquez-Rivera et al., 2009).
WHODAS 2.0 scale (WHO, 2015) is a generic tool for evaluating health and disability in the general and clinical population. For this study, the use of a 12-item scale, which has already been used in patients with fibromyalgia was selected. The items make up two dimensions that assess social-cognitive functionality (ScCF), integrating the domains of relationships, daily activities for work, cognitionm and participation; and self-care functionality (SCF), integrating the domains of mobility and self-care. Good levels of internal consistency have been reported for both subscales, with a Cronbach’s alpha of .83 for social-cognitive functionality and .81 for self-care functionality (Smedema et al., 2016).
Note. Slope/Shape factors are not included in the intercept model. A parameter value with a plus sign indicates the parameter value is fixed. *indicates that the factor loadings may be fixed to 4 (linear trajectory model) or freely estimated (unspecified model).
Figure 1 : Initial theorical model. MC=Metacognitions about symptom control, NMC=Negative metacognitions about symptom control, PMC=Positive metacognitions about symptom control, SEP=Self-efficacy to pain, CAT=Catastrohizing to pain, CP=Coping with pain, AC=Active coping, PC=Passive coping, RUM=Rumitation, HOP=Hopelessness, MAG=Magnification, FUN=Functionality, SCF=Sociocognitive functionality, FSC=Functionality for self-care, INT=Intensity. Own elaboration.
Numeric Pain Rating Scale: In order to assess the intensity of pain at the time of application of the instruments, the patients had to record the pain they felt at the time, scoring from 0 (absence of pain) to 10 (maximum pain level).
Individual survey. An individual survey on sociodemographic data was applied.
Since these instruments have not been validated in Colombia, a process of linguistic and conceptual equivalences was carried out by means of a judgment of experts for its subsequent application in the sample. To do this, the following steps were taken: 1. Direct translation of the scales; 2. Translation synthesis; 3. Back-translation; and 4. Expert evaluation.
2.4 Procedures for data collection
Two trained evaluators applied the scales in person to the sample of participants, after obtaining the informed consent.
The study took into account the ethical considerations established in Resolution 8430 (1993, October 4) of the Ministry of Health of the Republic of Colombia and those raised in Law 1090 (2006) of the Ministry of Social Protection, which regulates the Deontological and Bioethical Code of studies in Psychology.
2.5 Analysis of the information
Given that this research has as its main objective the modeling of a theoretical structure, the data analysis involved two moments. In the first of them, a descriptive analysis of the variables and a correlational analysis between them were performed using the SPSS 20® program. For this, the levels of reliability and adequacy to the factorial analysis of the variables were determined.
In a second moment, a modeling process was carried out by means of a trail analysis. The fitting evaluation of the model was carried out with the Mplus® 7.31 program and, for this, iterative procedures were used, with the Maximum Likelihood method, and the adjustment measures: Chi-square test, Root Mean Square Error of Approximation (RMSEA), Standardized Root Mean Squared Residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A significance level of 5% was used for all tests, and, a value of 0.50 was taken into account to identify the strength of the correlations among the variables.
3. Results
3.1 Sample description
The sample consisted of 108 women with a mean age of 47.2 years, being the most frequent age range in the sample corresponding to the interval 49-60, with 53.7%. Approximately 60% had a stable relationship and 68.52% of the sample had developed higher level studies, including technical or technological training and university education at undergraduate and graduate levels. Only 1.85% of the participants reported not having completed formal studies, although they had an adequate level of reading comprehension to allow the application of psychometric instruments. The socio-demographic details of the sample are summarized in Table 1.
Table 1 Sociodemographic variables, mood and affective balance. Correlation matrix
| Variable | Category | N=108 | |
| fi | % | ||
| Age ranges | 24-36 years | 18 | 16.67 |
| 37-48 years | 32 | 29.63 | |
| 49-60 years | 58 | 53.70 | |
| Marital status | Married/ Free Union | 66 | 61.11 |
| Single | 22 | 20.37 | |
| Separate/ Divorced | 17 | 15.74 | |
| Widowed | 3 | 2.78 | |
| Educational level | No studies | 2 | 1.85 |
| Elementary school | 13 | 12.04 | |
| Secondary school | 19 | 17.59 | |
| Technical/Technology | 41 | 37.96 | |
| Undergraduate | 18 | 16.67 | |
| Postgraduate | 15 | 13.89 | |
Note. N: Total sample; f i : absolute frequency; %: percentage of frequency.
3.2 Descriptive and correlational analysis
To start the data analysis, an evaluation of its behavior was performed by using three methods of normality evaluation. The first, by means of the Kolmogorov-Smirnov test, in which it was found that this assumption was not fulfilled; however, given that the results of the scales could be affected by the size of the sample, an analysis was also performed through the visual inspection of the QQ graphs, and we valued the Asymmetry and Kurtosis coefficients for each of the scales. As suggested for the development of analysis of structural equation models (Kline, 2011; Kumar & Upadhaya, 2017), these were found among parameters of normal distribution. Additionally, the criterion of the Central Limit Theorem (Kwak & Kim, 2017) was considered to assume that due to the size of the sample the data could be analyzed under the assumption of normal behavior.
The results of the descriptive analysis of the instruments are summarized in Table 2. The negative and positive metacognitions dimensions about the control of symptoms obtained an acceptable level of reliability, with scores in Cronbach’s alpha of .79 and .77, respectively.
The relationships between the analysis dimensions are presented in Table 3, which shows the correlation matrix among the variables of the study. The positive metacognitions variable showed weak correlations with the negative metacognitions variable, that is, Active coping with pain and Passive coping with pain. In contrast, the negative metacognitions variable presented a greater number and strength of correlation with Catastrophizing towards pain and its dimensions, with SocioCognitive Functionality, Functionality for Self-care, and Passive Coping to pain; and a negative correlation with Self-efficacy to pain.
In addition, the variable of Self-efficacy to pain presented moderate negative correlations with negative Metacognitions, Rumination, Magnification, Hopelessness, Catastrophizing to pain, Socio-Cognitive Functionality, and Functionality for Self-care, just as Low positive correlation with Active coping with pain, and negative correlation with Pain intensity. On the other hand, the Catastrophizing to pain showed moderate correlations with the variables of Socio-Cognitive Functionality and Functionality for Self-care, as well as weak correlations with Passive Coping to pain and Pain intensity.
3.3 Structural Model Development
To carry out the multivariate analysis, it was subjected to the determination under the structure of the trail analysis, which was done step by step, according to the results of the goodness of fit indices found between the relationships among variables. It is important to clarify that the resulting model is the product of changes that were made in the original model, following the values of the indices, but these modifications were made following the theoretical guidelines, which are described below:
Starting from the original model proposed in Figure 1, the following modifications were made: The latent variable of Metacognitions about the control of Symptoms was excluded from the analysis and the variable of positive Metacognitions, negative Metacognitions, and Selfefficacy to pain were used as endogenous variables. The dimensions of Rumination, Magnification, and Hopelessness, which constitute the pain catastrophism variable, were removed to use the global result of the instrument. The reliability results of the Pain Catastrophizing Scale allowed us to conclude that it was possible to use the global result of the instrument, and thereby improve the goodness of fit indices. The variables of coping with pain were removed from the model, because their presence reduced the validity of the goodness of fit indices, although they did not modify the coefficients of determination.
In Figure 2, the re-specified model is shown, in which latent variables of negative metacognitions and positive metacognitions, and pain self-efficacy can be seen. On the other hand, Catastrophizing to pain acts as a mediating variable on the intensity of pain, Socio-Cognitive Functionality, and Functionality for Self-care. Table 4 shows the results of the goodness of fit indices and the regression coefficients of the re-specified model that were best adapted statistically.
Table 2 Summary of descriptive data of each dimension of the study
| Scale | Dimenssion | Ítem | Range | x | S | α | IC 95% | P25 | P50 | P75 |
| CMSC | PMC | 9 | 9 to 36 | 23.66 | 6.684 | .774 | .708-.835 | 18 | 24 | 29 |
| NMC | 8 | 8 to 32 | 22.16 | 5.988 | .798 | .735-.851 | 18 | 22 | 27 | |
| SEP | SEP | 10 | 0 to 60 | 34.29 | 14.213 | .924 | .901-.944 | 23 | 36 | 45 |
| CAT | CAT | 13 | 0 to 52 | 25.56 | 13.112 | .942 | .892-.942 | 16 | 26 | 36 |
| CAD | AC | 16 | 16 to 80 | 48.30 | 9.983 | .794 | .733-.833 | 41 | 48 | 57 |
| PC | 8 | 8 to 40 | 24.95 | 8.172 | .824 | .769-.870 | 18 | 25 | 32 | |
| WHODAS 2.0 | SCF | 7 | 7 to 35 | 15.86 | 4.892 | .82 | .773-.876 | 12.25 | 16 | 19.75 |
| FSC | 5 | 5 to 25 | 18.21 | 5.267 | .83 | .763-.867 | 15 | 18.5 | 22 | |
| INT | INT | 0 to 10 | 6.69 | 2.684 | 5 | 7 | 9 |
Note. CMSC = Metacognitions Questionnaire about Symptom Control, NMC=Negative Metacognitions Dimension, PMC=Positive Metacognitions Dimension, SEP=Self-efficacy to pain Questionnaire, PCQ=Pain Catastrophism Questionnaire, RUM=Rumination Dimension, MAG = Magnification Dimension, HOP=Hopelessness Dimension, CAT=Catastrophizing to pain , CPQ=Pain Coping Questionnaire, AC=Active Coping Dimension, PC=Passive Coping Dimension, SCF=Social-Cognitive Function Dimension, FSC=Functionality for Self-Care Dimension. x=Mean, S=Standard deviation, α=Cronbach’s alpha, CI=Confidence interval, P25=25th percentile, P=50th percentile, P=75th percentile.
Table 3 Matrix of correlations among variables
| PMC | NMC | SEP | CAT | FSC | SCF | INT | ||
| PMC | r | 1.00 | 0.204* | -.008 | -.067 | -.030 | -.040 | -.115 |
| p | .00 | .034 | .934 | .494 | .760 | .677 | .236 | |
| NMC | r | -.329** | .535** | .441** | .385** | .040 | ||
| p | .001 | .000 | .000 | .000 | .682 | |||
| SEP | r | -.564** | -.563** | -.590** | -.371** | |||
| p | .000 | .000 | .000 | .000 | ||||
| CAT | r | .572** | .562** | .244** | ||||
| p | .000 | .000 | .011 | |||||
| FSC | r | .720** | .323** | |||||
| p | .000 | .001 | ||||||
| SCF | r | .403** | ||||||
| p | .000 |
Note. PMC=Positive metacognitions, NMC=Negative metacognitions, SEP=Self-efficacy to pain, CAT=Catastrophizing to pain, AC=Active coping, PC=Passive coping, SCF=Social-cognitive function, FSC=Functionality for Self-care, I=Intensity, r=Pearson’s correlation coefficient, p=Level of significance. * The correlation is significant at the 0.05 level (bilateral). Outlined in bold. ** The correlation is significant at the 0.01 level (bilateral). Outlined in bold.
Starting from the final model, we can conclude that the latent variables Positive Metacognitions, Negative Metacognitions, and Self-efficacy to pain influence each other, so under this influence the direct effect of the variable Positive Metacognitions on Socio-Cognitive Functionality had a magnitude of -.055, a -.050 on Functionality for Self-care, and -.089 on Pain intensity , which as effect magnitudes are not considerable. Therefore, it is assumed that the impact of the exogenous variable of Positive Metacognitions is not representative over its exogenous variables (Self-Care Functionality, Socio-Cognitive Functionality, Pain intensity). In turn, negative Metacognitions as an exogenous variable of Catastrophizing to pain had a direct effect β = .393, while the direct effect of Catastrophizing pain as an endogenous variable of Self-efficacy to pain was β = .437. The effects of these two variables explain 45.5% of the variance of Catastrophizing to pain in this model.
In relation to the endogenous variable of Socio-Cognitive Functionality, it was observed that positive Metacognitions had a direct effect β = .55, which is not representative; Negative metacognitions had a direct effect β =.196, which is still considerably lower; and Self-efficacy to pain had a direct effect β = .351, which can be considered important. Here it should be noted that the strength of the magnitude of this relationship is negative, which means that for each point that increases self-efficacy, the score in the subjects’ social cognitive functionality will decrease by three points; while Catastrophizing to pain had a direct effect β = .269. These variables explain 43.5% of the variance of Socio-Cognitive Functionality.
Table 4 Goodness of fit indices and regression coefficient of the final model
| Model | description | χ2 (gl) (p) | RSMEA (IC 90%) | CFI | TLI | SRMR | R2 |
| NMC-PMC- | 4.8 (1) (p = .029) | 0.187 (.048-.036) | .985 | .711 | .027 | SEP=11.2% | |
| SEP (L) | CAT=45.5% | ||||||
| >CAT> | SCF=43.6% | ||||||
| SCF-FSC-INT | FSC=43.4% | ||||||
| INT= 15.9% |
Note. NMC=Negative Metacognitions Dimension, PMC=Positive Metacognitions Dimension, SEP=Pain Selfefficacy to pain Questionnaire, CAT=Pain Catastrophizing to pain Questionnaire, SCF=Social-cognitive Function Dimension, FSC=Functionality for Self-Care Dimension. CI=Confidence interval, L=Variable considered as latent, χ 2=Chi squared, gl=Degrees of freedom, p=Level of significance, RMSEA=Root Mean square error of approximation, CFI=Comparative fit index, TLI=Tucker-Lewis Index, SRMR=Standardized mean square residual, R 2=Multiple squared correlation.
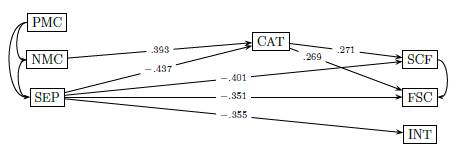
Figure 2 Re-specified model. In the resulting model, the exogenous variables are seen to influence each other. Notice that SEP has a direct effect on endogenous variables and CAT behaves as a moderating variable for endogenous variables. MC=Metacognitions about symptom control, NMC=Negative metacognitions about symptom control, PMC=Positive metacognitions about symptom control, SEP=Self-efficacy to pain, CAT=Catastrohizing to pain, CP=Coping with pain, AC=Active coping, PC=Passive coping, RUM=Rumitation, HOP=Hopelessness, MAG=Magnification, FUN=Functionality, SCF=Sociocognitive functionality, FSC=Functionality for self-care, INT=Intensity. Own elaboration.
For the endogenous variable of Functionality for SelfCare, we found that positive metacognitions had a direct effect β = .50, which is not representative; the negative metacognitions variable had a direct effect β = .120, which is still considerably lower; Self-efficacy to pain had a direct effect β = .401, an even greater effect than in the case of Socio-Cognitive Functionality; while Catastrophizing to pain had a direct effect β = .271. These variables explain 43.3% of the variance of Functionality for Self-care. It is important to mention that the resulting model states the existence of a considerable effect on the functionality variables whose origin cannot be determined.
To finish with the endogenous variables, it should be noted that in Pain intensity, the positive Metacognitions had a direct effect β = −.089, which is not representative; Negative metacognitions had a direct effect β = .111; Self-efficacy to pain had a direct effect β = .355; and Catastrophizing to pain had a direct effect β = .098. These variables explain 15.9% of the variance of pain intensity. In summary, the final model had a barely acceptable fit (χ 2 = 4.8, p = .029, RMSEA=.187, CFI=.985, TLI=.711 CFI=.985, SRMR=.027), which implies that the model does not manage to validate itself.
4. Discussion
The results of this study do not allow us to affirm that the S-REF Model can satisfactorily explain the variables of coping, functionality, and pain intensity in the study sample. The analysis does not support with statistical evidence the causal relationships proposed in the theoretical model, although some research has proposed that this maybe use ful for understanding the role of meta cognitions in the psychological processes associated with the experience of pain and its physical and emotional impact on fibromyalgia (Kollmann et al., 2016; Spada et al., 2016).
However, this general result does not diminish the importance of the conclusions that can be drawn from the final model. In this sense, the results suggest that the variables of Positive Metacognitions, Negative Metacognitions, and Self-efficacy to pain act as exogenous variables and influence each other, despite the fact that the positive Metacognitions did not have a direct impact on the moderating variable (Catastrophizing to pain) and the exogenous variables (Self-Care Functionality, Socio-Cognitive Functionality, and Pain intensity). These results differ with the study developed by Kollmann et al. (2016), in which it was found that positive Metacognitions influenced the variables of physical and work impact that they evaluated.
Given these results, two reflections can be raised: (1) the few correlations established by positive Metacognitions cast doubt on their relevance in pain self-regulation processes, although different theorists consider the role of beliefs and especially metacognitive beliefs fundamental factors in self-regulation phenomena (Bandura, 1998; Beer & Moneta, 2012; Vohs & Baumeister, 2011); or (2) based on their experiences, the patients have not developed useful or beneficial attributions to the content of their thoughts and control processes.
Although the results have not found a direct effect of positive Metacognitions on functionality, coping or pain intensity, it cannot be said that these types of cognitions do not have final effects on the pain experience process, since, as can be seen in the model, this variable does generate an impact on the variables: Negative metacognitions and Self-efficacy to pain, that is, it can be stated that in this study its effect may be indirect on them. In contrast to this directionality of the effect, in their recent publication, Schütze et al. (2020) has suggested that pain intensity may have an influence on positive Metacognitions, although this directionality of effect was not considered in this study.
On the other hand, the results suggest that the two variables, both Negative Metacognitions and Self-efficacy to pain, influence each other and behave as latent on Catastrophizing to pain. Thus, the greater the belief in the absence of control over the symptoms of fibromyalgia is, especially pain, the lower the belief in self-efficacy about this same symptom is expected. Theoretical links between personal self-efficacy and the sense of control have already been raised in other areas (Ajzen, 2002; Bandura, 1992) but not in the field of pain, which is novel because this relationship between variables has not been included in other research.
Regarding the effect of the negative metacognitions variable on Catastrophizing to pain, it can be said that when thought control strategies are linked to attempts to reduce these negative cognitions, a paradoxical effect occurs, leading to an increase in the catastrophic content of the cognitions (Wang et al., 2018; Wenzlaff & Wegner, 2000; Yoshida et al., 2012), and in negative evaluations in different dimensions of the subject (Nolen-Hoeksema et al., 2008).
The relationship between the variables of Self-efficacy to pain and Catastrophizing to pain has been documented in other studies in this population (Sánchez et al., 2011; Tirado et al., 2014). Few authors have been inclined to present explanations about the nature of this relationship: some consider them independent evaluations, highlighting their function as beliefs (Quartana et al., 2009; Sánchez et al., 2011); while others postulate theories about their interdependence relationship within the framework of theoretical models. Such is the case of Woby et al. (2007), who related them in the framework of the Fear-Avoidance Model, suggesting that the catastrophic assessment of pain precedes the perception of self-efficacy for functioning in the subject and, in this way, the resulting behavior to pain is triggered in the face of pain, either as that of confrontation or avoidance.
In our model, we have interpreted that self-efficacy assessments exercise declarative content functions at the higher level that will guide the perception of the individual’s ability to manage pain, including the tendency to catastrophize, but no conclusions can be drawn about the influence of Catastrophizing to pain in Self-efficacy to pain. That is, that Self-efficacy to pain can affect the Catastrophizing to pain, with whom it competes at the intermediate level, inducing a cascade of actions destined for the execution and control of action plans, whether they are a behavioral or a cognitive action.
At the second level of the model, we see the relationships that are established with the higher level. According to what was proposed by the original authors of the S-REF, the higher level participates directly in the selection of plans to be executed at the second level. Similarly, this intermediate level can participate in the creation of new beliefs (Wells, 2000). This process must be considered dynamic and with a transforming capacity of cognitions related to pain. This is one of the elements that has been ignored in the analyses of the Neuromatrix Model when it is used in the understanding of the cerebral phenomena involved in the processing of painful stimuli (Melzack, 2001).
Now, we see that the variables of Self-efficacy to pain and negative Metacognitions can explain a high percentage of the variance of Catastrophizing to pain, mainly due to the effect of Self-efficacy to pain. In this sense, the idea of Catastrophizing to pain is also taken up as a moderating variable between exogenous and endogenous variables, given that in the initial model proposed, the variables of Active Coping with Pain and Passive Coping with Active Pain were also constituted in Moderator variables directly influenced by Catastrophizing to pain.
On the other hand, the determination coefficients for the variables of Active coping with pain and Passive coping with pain explained a low percentage of their variance in the proposed general model, and affected the goodness of fit indices, resulting in the decision of excluding these two dimensions in the final model. Coping with pain is one of the variables that presents problems when trying to analyze it associated with other psychological variables, and it has been suggested that there is a great lack of knowledge of the strategies and styles of coping in the face of the painful experience and the evaluation domains for the Latin-American population (Campbell et al., 2009).
In any case, the fact of having excluded these variables cannot simply be translated as that coping with pain was completely excluded from the model, since Catastrophizing to pain is actually a coping strategy. In fact, in its origins, this construct was a dimension of coping styles that later, due to the robustness of its results, evolved to become an independent construct (Neblett, 2017).
Returning to the idea of Catastrophizing to pain as a moderating variable between exogenous and endogenous variables, the statistical model supported the presumption of the theoretical model for the effect of this, in the deterioration of the levels of functionality in both dimensions, with a predominance over Functionality for Selfcare, and also for the performance in the Socio-Cognitive Functionality dimension. Other research has found an association between higher levels of Catastrophizing to pain with the deterioration of the physical functionality (Besen et al., 2017; Craner et al., 2016; Vohs & Baumeister, 2011).
Another point to consider is that the statistical analysis confirmed the initial assumption that Self-efficacy to pain exercises functions at the intermediate level of the model, in such a way that it is able to directly influence endogenous variables, besides the indirect effect that exerts through the Catastrophizing to pain. Thus, the model proposes that Self-efficacy to pain has a negative effect on the impact variables with a predominance on Functionality for Self-care, that is, the higher the degree of self-efficacy, the lower the commitment in terms of functionality. Several studies have provided similar conclusions (Alok et al., 2014; Peñacoba-Puente et al., 2015; Sánchez et al., 2011; Van Liew et al., 2018), and the remarkable thing about this finding is that Self-efficacy to pain generated a greater effect on them than the Catastrophizing to pain. Other studies have found similar results, even in the same impact proportions (Sánchez et al., 2011; Tirado et al., 2014).
Additionally, the results should be mentioned in relation to the intensity of the pain. The model explains only a small percentage of the variance of this variable; and the only variable that had an impact on it was Self-efficacy to pain. This may be related to the conclusions that other authors have made of this, as the variable with the greatest impact in the daily life of those who suffer from fibromyalgia, in the perceptions that they have of the painful experience (De Rooij et al., 2013; Lee et al., 2017), as well as the level of emotional commitment they manifest. Other investigations have found this relationship, although they have not considered techniques of explanatory analysis (Mirõ et al., 2011; Sánchez et al., 2011; Van Liew et al., 2018; Wells-Federman et al., 2003).
On the other hand, it should be noted that these variables of Self-Care Functionality, Socio-Cognitive Functionality, and Pain Intensity indirectly represent the third and last level, also called processing units, because it is constituted by the interoceptive sensory processing subcircuits, processing exteroceptive sensory, and cognitive processing, which are subject to the effects of the intermediate level or self-regulation.
That is to say that these cognitions and the action plans that they induce intervene directly on the processing units, especially through the induction of monitoring or hyper vigilance, and with it an intensification of the activity of the intermediate level, with the consequent increase in rumination processes, a frequent characteristic in patients with fibromyalgia syndrome (Coppieters et al., 2015). Now, although the theoretical model also predicts that the activity of the cognitive processing subunit influences the level of self-regulation through intrusive thoughts, the design of this project does not allow to reach this conclusion.
Finally, according to the results obtained, the beliefs and metacognitions of people who suffer from chronic pain, as in the case of fibromyalgia, are not enough to explain the pain, the way a person deals with pain, how it affects their performance in society, and its intensity, that is, the thoughts are not the origin of this condition and would not increase it. This would have important implications both for the conceptualization of the fibromyalgia condition itself and for the pharmacological and psychological therapeutic approach. In this last aspect, it should be understood that, in psychological therapy, false expectations should not be created about how the change in thoughts related to pain will modify pain levels, and in this way prevent fibromyalgia patients from feeling, as with pharmacological treatments and others, frustrated by the low response to the modulation of the pain experience.
5. Conclusions
With the statistical technique of pathway analysis used in the study, it cannot be stated that the S-REF Model can satisfactorily explain the variables of coping, functionality, and pain intensity in the study sample. It is possible that it be necessary to consider that other variables have an effect of greater impact on the model, and that they have not been included in the proposed model.
However, this general result does not diminish the importance of the conclusions that can be drawn between the dimensions that make up the model resulting from the analysis.
In the model derived from the study, positive metacognitions, negative metacognitions, and pain self-efficacy were considered as exogenous variables. They constitute the content of self-beliefs capable of directing the action plans that are put into operation in the processes of cognitive self-regulation in the face of the painful experience, and they are capable of influencing one another.
It is possible that metacognitive variables take part in determining the functionality in patients with fibromyalgia, but they do not modulate pain intensity. Self-efficacy to pain is the variable that exerts the greatest influence on the impact variables and, possibly, participates in the targeting of cognitive self-regulation plans that decrease the intensity of pain and improve functionality.
Additionally, catastrophic cognitions about the painful experience are influenced by negative evaluations about control strategies and by the perception of self-efficacy in the face of this experience. It also acts as a moderator of the impact variables.
Finally, it can be concluded that psychological variables and cognitions cannot explain the level of intensity of pain reported by patients with fibromyalgia.
6. Limitations and recommendations
An important limitation of the study was the sample size, due to its influence on the analysis of structural equations. However, it should be mentioned that access to this type of clinical samples is usually very limited. Other investigations that include larger sample sizes should be considered.
Additionally, a limitation was that this study did not have male participants, which can be expected due to the higher prevalence of this condition in women. For future studies, the inclusion of the male population is recommended.
On the other hand, it is convenient that theoretical and applied research in psychology focus on the adequacy of instruments or on the design of new psychometric scales for the study of chronic pain in our population, since some instruments used in this study only had Expert judgment of linguistic and conceptual equivalence and not with scales at a population level.
It would also be advisable to study the relationship of the variables studied here with other clinical and therapeutic variables that can demonstrate their influence on metacognitive processes. In the future, it is recommended to explore the influence of other variables that explain the alteration of the functionality and intensity of pain, taking into account other dimensions that have shown relevance in reference sources.














