1. Introduction
Cancer is a serious health problem for people of all countries, regardless of wealth or social status (WHO, 2020), and it is the second leading cause of death in the United States (Siegel et al., 2020). The impact of this chronic illness on the biopsychosocial aspects of individuals’ health and well-being cannot be simply interpreted as a medical issue (Chen & Chang, 2012); instead, it represents a severe crisis for both patients and relatives (Aydın Sayılan & Demir Do˘gan, 2020) with important implications in patients’ lives, daily routines, work activities, relationships, and family roles (Zabalegui et al., 2005).
While the dominant psycho-oncological research has traditionally been focused on negative impact of the disease or treatments (e.g., distress, loss of functioning, anxiety, depression), the more recent resource-oriented perspective has been focused on the individual’s positive creative resources (e.g., optimism, self-efficacy, sense of coherence, and social support; Finck et al., 2018). About these, the social support (SS) has a considerable impact on physical and mental health (Cohen & McKay, 2020; Eom et al., 2013) and has been identified as the most significant factor in helping patients adjust to cancer (Harper et al., 2016; Jie et al., 2019; You & Lu, 2014).
Previous research highlighted that patients who receive appropriate SS experience higher levels of wellbeing (Crothers et al., 2006; Pinar et al., 2012; Tan & Karabulutlu, 2005). However, SS is not a unitary concept but rather a meta-construct of different components (Prins et al., 2004). Generally, it is divided into “two broad ideas: social support concerns (1) the support that is actually received (i.e., structural support and functional support) or (2) the individual’s subjective appraisal of the social support (perceived social supportPSS)” (Den Oudsten et al., 2010, p. 500). Cohen et al. (2000) also showed that the social support is composed of received and perceived social support; they proposed a theoretical model -the social, psychological, behavioral, and biological pathways- to explain how social support can be a predictor of disease morbidity and mortality. The PSS may be even more critical to predict a better outcome in patients with a diagnosis of cancer (Applebaum et al., 2014), showing a role in reducing physical, psychosocial, and emotional problems (Aydın Sayılan, & Demir Dog˘an, 2020), and a “buffer effect” in protecting individuals against the negative impact of stressful events (Pocnet et al., 2016). For example, a recent study (Tsuchiya et al., 2020) found that cancer patients who disclose their diagnosis to close friends perceived more informational support. The family also seems to be a leading source of SS for cancer patients, and especially the support that comes from partner (Aydın Sayılan & Demir Do˘gan, 2020; Jie et al., 2019; Lee et al., 2019; Pinar et al., 2012). Furtherly, a longitudinal study (Thompson et al., 2017) among women with breast cancer showed that those who perceived a decline of social support during the first year after diagnosis reported worse depressive symptoms and worse general health; thus, highlighting the importance to increase the knowledge about how several sources of PSS may have an impact on various indicators of patients’ well-being.
The patients’ PSS is often studied in association with illness perception. The individuals with chronic diseases -including cancer- develop the illness perception from their physical symptoms, previous medical experiences, and information coming from family, healthcare professionals, and media (Aydın Sayılan & Demir Dog˘an, 2020; Lee et al., 2019). And the positive illness perception is associated with physical, social, and psychological wellbeing (Fanakidou et al., 2018; Finck et al., 2018).
Optimism is also crucial in this detecting context with its positive association with PSS; both have been identified as critical resources for cancer patients (Applebaum et al., 2014; Shelby et al., 2008). According to He et al. (2016), lower degree of PSS predicted lower levels of optimism. The optimistic thought also “enhances the perception of social network availability, which diminishes the appraisal of threat, increases feeling of success, and improves social desirability” (Matthews & Cook, 2009, p. 3) in a virtuous circle of mutual influence between PSS and optimistic attitude. Indeed, others suggested that optimism, being a socially accepted behavior, could improve the offered SS (Hodges & Winstanley, 2012).
Additionally, the PSS also influences the patients’ emotions, cognition, and behaviors, consequently making individuals capable to maintain and promote their health status and well-being (Olsson et al., 2017). As a result, the individuals can achieve a more satisfying life, through better health and the perception of a supportive social network (Bozo et al., 2009; Hamdan-Mansour et al., 2015; Pocnet at al., 2016). It is, thus, important to understand the specific roles of the various sources of PSS on patients’ life-satisfaction to foster the strengthening of social networks that can enhance everyday life support.
Ultimately, regardless of the source (Ng et al., 2015; Pinar et al., 2012), the PSS directly influences the quality of life (Aydın Sayılan & Demir Do˘gan, 2020), featuring the measure of the patients’ perception of selfwell-being (Ng et al., 2015). Some studies have paid particular attention to the symptom of fatigue (Den Oudsten et al., 2010; Servaes et al., 2002). It is not an organic illness or the result of a long effort, but it results in a substantial reduction in previous levels of daily personal and social activities (Prins et al., 2004). The patients with fatigue, which is often associated with typical chemotherapy symptoms (e.g., nausea and vomiting; Servaes et al., 2002; Eom et al., 2013) perceive less SS than those with other syndromes (Prins et al., 2004). This could reduce the size of the network and/or induce cancer patients giving less support to others, generating an imbalance that would induce them to withdraw (Den Oudsten et al., 2010). The closeness of the various loved ones can be a valid and specific help in the different moments of difficulty, which makes worthing to deepen the role of the different sources of PSS on symptoms.
Previous research seemed inconsistent to identify the different types and sources of PSS. Although it is a highly explored topic, the various available classifications make the results poorly comparable. The general purpose of this study was to increase the knowledge about the role of different sources of PSS (i.e., family, friends, and significant other) and examine their association with psychological well-being in a group of cancer patients. We hypothesized high levels of well-being associated with high levels of PSS. As indicators of wellbeing, we used the constructs that have been shown to have a significant influence on illness experience. In light of previous research findings, when the patients’ levels of PSS were high (regardless of the sources; i.e., family, friends, and significant other), we expected to find a better illness perception (H1), and an increase of optimism (H2) and life satisfaction (H3) levels. Finally, we also expected to find a better general quality of life, with an improvement in the patient’s functionality, with a particular increase in physical functioning and related symptoms (H4).
2. Method
2.1 Participants and procedure
Participants were recruited in a public hospital in Italy between September and December 2019. A specific authorization from the medical director was obtained and the study procedure was approved by the Internal Review Board of the psychological research of the University of Enna “Kore”. The data collection was performed by a single researcher who -during waiting time for personal medical treatments or examination- explained to the patients the study objective. 138 patients were reached, of whom 13 refused to participate (since participation in the study was voluntary, we did not investigate the reasons for declining) and 4 abandoned the procedure (3 participants considered the questions too emotionally difficult and 1 gave no explanation). They arrived at the hospital unit with different medical needs, such as carrying out periodic check-ups, talking with a doctor, undergoing themselves to chemotherapy treatment in day-hospital. After explaining the purpose of the study, all participants signed informed consent. The inclusion criteria envisaged the enrolment of patients who went to hospital for oncological needs, but excluded one patient with psychological disorders (i.e., mental delay). As a result, we used a convenience sample, selected by a non-random procedure.
Participants were mainly women (70.2%), aged from 26 to 88 years (M = 61.90, SD = 12.16) with different cancer sites (breast 35.8%, prostate 2.5%, lungs 5.8%, liver .8%, kidneys 1.7%, head .8%, colon 13.3%, other 39.3%), time elapsed since diagnosis (less than six months 39.2%, from 6 to 12 months 13.3%, from 1 to 2 years 20.8%, from 3 to 5 years 13.4%, more than 5 years 13.3%), and presence of metastasis (21.7%). This information was conditioned by what patients knew or have understood about their disease since we did not have access to the medical records. They mostly have a partner (68.6%), and 84.8% of the participants have children (M = 2.46, SD = 1.03). The most diffused treatment was chemotherapy (38.8%), only 1.7% of the participants indicated radiotherapy, and 39.7% reported no current treatments. Because of the hospital setting, all participants perceived themselves as patients and not as survivals. We have not consulted the medical records to extrapolate an objective parameter useful to this classification.
All patients completed the battery of psychometric tests administered in compliance with the privacy guarantee regulations according to the Legislative Decree n. 196/2003 and the GDPR (EU Regulation n.2016/679). Data were collected for research purposes only and treated in an aggregated and anonymous form.
2. 2 Measures
2.2.1 Multidimensional Scale of Perceived Social Support (MSPSS)
The MSPSS (Zimet et al., 1988) measures the perceived social support and it is composed of three subscales, which are able to distinguish the source of social support: family, friends, and significant other. It is comprised of 12 items, based on a 7-point Likert scale from 1 (very much disagree) to 7 (very much agree). As a result, the maximum achievable score is 84. Scores from 69 to 84 reflect high-PSS, from 49 to 68 reflect moderatePSS and from 12 to 48 reflect low-PSS. The Cronbach’s alpha was calculated for the three subscales (Significant Other=.91; Family=.87; Friends=.85). The Italian validation of the instrument (De Maria et al., 2018) in the healthcare sector reported good reliability and validity in reference to chronic diseases and satisfying internal consistency with cancer patients (Cronbach’s alpha=.89; Bozo et al., 2009).
2.2.2 Illness Perception QuestionnaireRevised (IPQ-R)
The IPQ-R (Moss-Morris et al., 2002) is a generic measure of illness perception and it is composed of three dimensions of illness perception: identity, opinions, and causes. The first subscale -“identity”- examines how an individual attributes 14 commonly experienced symptoms to the illness, using yes/no responses (e.g., pain, nausea, tiredness). The second subscale -“opinions”- is measured using 38 items rated on a 5-point Likert scale concerning probable causes involved in the development of the disease (e.g., “My illness won’t last long”; “I can do a lot to control my symptoms”), subdivided into seven sub-dimensions: acute/chronic duration, cyclical duration, consequences, personal control, treatment control, disease coherence, and emotional representations. The last dimension -“causes”- is assessed using 18 items concerning possible illness causes, which are rated on a 5-point Likert scale (e.g., stress, environmental pollution, alcohol). All subscales demonstrate good internal reliability and Cronbach’s alpha for each subscale ranged from .79 to .89. The IPQ-R has been used among cancer patients, and it has demonstrated acceptable psychometric properties (Lee et al., 2019), also in the Italian version (Giardini et al., 2007) which resulted homogeneous with the original version.
2.2.3 Life Orientation Test-Revised (LOT-R)
The LOT-R (Scheier et al., 1994) measures the dispositional optimism and it is a 10-item scale, which included 4 unscored items (Cronbach’s alpha=.78). We used the Italian version (Giannini et al., 2008) with a 5point Likert scale from 0 (strongly disagree) to 4 (strongly agree) for 10 items. Total scores range from 6 to 30, with higher scores indicating higher optimism. Cronbach’s alpha value is .81 and it confirms the unidimensional structure of the original version.
2.2.4Satisfaction with Life Scale (SWLS)
The SWLS (Diener et al., 1985) measures the life-satisfaction and it was used to detect general information about patients’ life well-being in the present study. We used the Italian version (Di Fabio & Busoni, 2009), which is articulate in five items on a 7-point Likert scale, from 1 (strongly disagree) to 7 (strongly agree), with higher scores indicating higher satisfaction with life. The SWLS demonstrated high internal consistency reliability (α =.87) and confirms the unidimensional structure of the original version.
2.2.5 European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30)
The EORTC QLQ-C30 (Aaronson et al., 1993) is an integrated system for assessing the quality of life (QoL) of cancer patients participating in clinical trials and other types of research in which patient-reported outcomes are collected. It consists of 30 items, which belong to five functioning scales (physical, role, emotional, cognitive, and social functioning), three symptom scales (fatigue, nausea, and vomiting), six single symptoms (dyspnoea, insomnia, loss of appetite, constipation, diarrhoea, and financial difficulties), and a 2-item general health/QoL scale (i.e., “How would you generally assess your health over the last seven days?”, “How would you generally assess your quality of life over the past seven days?”; Cronbach’s alpha>.75). A summary score of the EORTC QLQC30 can be calculated. All scores are transformed to the range 0-100. High scores on the functioning scales and on the global health/QoL scale indicate good QoL, while high scores on the symptom scales indicate reduced QoL. The Italian version was used here (Apolone et al., 1998).
2.3 Statistical analysis
First, descriptive analyses were carried out to summarize the patients’ beliefs about their physical symptoms and causal attribution to cancer. A series of standard multiple regression analyses were also performed to study patients’ psychological well-being derived from PSS (from family, friends, and significant other) at the time of the survey. Based on previous research, we considered illness perception, optimism, life satisfaction, and quality of life as indicators of psychological well-being. There were no missing data. We used IBM SPSS Statistics for Windows, version 25.0.
3. Results
3.1 Power Analysis
A post hoc power analysis to compute achieved power, given α, sample size, and effect size, was conducted using G∗Power 3.1.9.7; the study had a power of 94% (.001 alpha level) to detect an effect size of f 2 = .21 for personal control, 90% (.05 alpha level) to detect an effect size of f 2 = .09 for coherence of disease, 87% (.001 alpha level) to detect an effect size of f 2 = .17 for optimism, 98% (.001 alpha level) to detect an effect size of f 2 = .26 for life satisfaction, 82% (.05 alpha level) to detect an effect size of f 2 = .07 for physical functioning, 63% (.05 alpha level) to detect an effect size of f 2 = .04 for fatigue, 68% (.05 alpha level) to detect an effect size of f 2 = .05 for fatigue, and 76% (.05 alpha level) to detect an effect size of f 2 = .06 for diarrhoea.
3.2 Illness perception
Firstly, on a descriptive level, we assessed the first and the third part of the IPQ-R to show the patients selfperception of the cancer. We investigated how the physical symptoms were distributed in the examined group of cancer patients (IPQ-R Part 1). The perception of the presence of fourteen different ailments was reported with high frequencies of fatigue (67.8%) and loss of energy (55.4%). All the results are shown in Table 1.
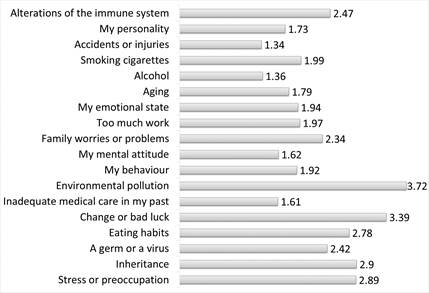
We also explored patients’ beliefs about the causes of their illness (IPQ-R Part 3). Data analyses revealed that environmental pollution (M = 3.72; SD = 1.31) and change or bad luck (M = 3.39; SD = 1.25) were the most frequently chosen responses, followed by inheritance (M = 2.90; SD = 1.53), stress and preoccupation (M = 2.89; SD = 1.28), and eating habits (M = 2.78; SD = 1.29), whereas accidents or injuries (M = 1.34; SD = .66) and use of alcohol (M = 1.36; SD = .72) were the less frequently chosen alternatives (Figure 1). When the examined patients were required to order the possible illness causes on a 3-position hierarchical scale, most of them put inheritance first (19.6%), eating habits in second place (17.5%), and environmental pollution in third place (19.5%).
Table 1 Cancer Patients’ Physical Symptoms (IPQ-R Part 1)
| Symptom presence | Patients’ attribution of the symptoms to the disease | |||
|---|---|---|---|---|
| N | % | N | % | |
| Pain | 44 | 36.4 | 42 | 34.7 |
| Sore throat | 19 | 15.7 | 11 | 9.1 |
| Nausea | 48 | 39.7 | 47 | 38.8 |
| Wheezing | 57 | 47.1 | 48 | 39.7 |
| Weight loss | 52 | 43.3 | 44 | 36.7 |
| Fatigue | 82 | 67.8 | 76 | 62.8 |
| Joint stiffness | 47 | 38.8 | 42 | 34.7 |
| Redness of the eyes | 25 | 20.7 | 16 | 13.2 |
| Wheezing | 49 | 40.8 | 41 | 34.2 |
| Headache | 35 | 29.2 | 22 | 18.3 |
| Upset stomach | 56 | 46.7 | 49 | 40.8 |
| Sleep disorders | 60 | 49.6 | 45 | 37.2 |
| Dizziness | 43 | 35.5 | 29 | 24.0 |
| Loss of energy | 67 | 55.4 | 63 | 52.1 |
3.3 Illness perception and PSS
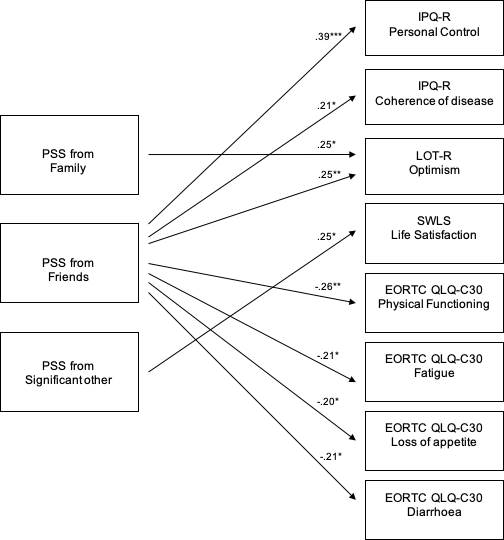
The association between the seven factors of patients’ disease opinion (IPQ-R Part 2) and PSS was detected. Specifically, inserting PSS from family, friends, and significant others as independent variables and acute/chronic duration, cyclical duration, consequences, personal control, treatment control, disease coherence, and emotional representations as dependent variables. Consequently, the performed regression analyses when PSS from friends was inserted as an independent variable revealed the following statistically significant results: personal control (β = .39, t = 4.58, p = .000), and disease coherence (β = .21, t = 2.27, p = .025). No other associations were found between PSS and the other evaluated disease opinions. Outcomes about relationship between illness perception and PSS are displayed in Table 2.
3.4 Optimism and PSS
Further, we investigated the association between optimism and PSS. Based on our findings, PSS seemed associated with higher levels of positive psychological disposition. Specifically, when inserting PSS from family and PSS from friends as independent variables and optimism as a dependent variable, data analyses highlighted the following statistically significant results: PSS from family (β = .25, t = 2.01, p = .047), and PSS from friends (β = .25, t = 2.85, p = .005). However, no statistically significant association was found between PSS from significant others and optimism. Complete results referring relationships between optimism level and PSS are shown in Table 2.
Table 2 Standard Multiple Regression Analysis between PSS and Psychological Well-Being
| β | t | Sig. | R2 | |
| IPQ-R: Personal Control Family | -.10 | -.82 | .413 | .184 |
| Friends | .39 | 4.58 | .000 | |
| Significant Other | .17 | 1.41 | .162 | |
| IPQ-R: Coherence of disease Family | .10 | .77 | .441 | .094 |
| Friends | .21 | 2.27 | .025 | |
| Significant Other | .10 | .78 | .439 | |
| LOT-R: Optimism Family | .25 | 2.01 | .047 | .152 |
| Friends | .25 | 2.85 | .005 | |
| Significant Other | .01 | .05 | .962 | |
| SWLS: Life satisfaction Family | .19 | 1.61 | .111 | .208 |
| Friends | .13 | 1.53 | .128 | |
| Significant Other | .25 | 2.03 | .044 | |
| EORTC QLQ-C30: Physical functioning Family | .08 | .58 | .562 | .064 |
| Friends | -.26 | -2.78 | .006 | |
| Significant Other | -.03 | -.26 | .798 | |
| EORTC QLQ-C30: Fatigue Family | -.02 | -.15 | .879 | .042 |
| Friends | -.21 | -2.24 | .027 | |
| Significant Other | .05 | .40 | .689 | |
| EORTC QLQ-C30: Loss of appetite Family | -.09 | -.68 | .500 | .047 |
| Friends | -.20 | -2.14 | .035 | |
| Significant Other | .18 | 1.36 | .178 | |
| EORTC QLQ-C30: Diarrhoea Family | .04 | .32 | .749 | .052 |
| Friends | -.21 | -2.26 | .026 | |
| Significant Other | -.09 | -.64 | .523 |
3.5 Life satisfaction and PSS
We also explored the association between perceived social support and life satisfaction in cancer patients. Based on data drawn from the examined group of cancer patients, we found a positive significant association between PSS from significant other and life satisfaction scores. When inserting PSS from significant other as an independent variable and life satisfaction as a dependent variable, the performed regression analyses showed a statistically significant result: β = .25, t = 2.03, p = .044. Instead, life satisfaction did not appear related to any of the other PSS sources (i.e., family and friends). Outcomes about relationships between life satisfaction and PSS are presented in Table 2.
3.6 Quality of life and PSS
Finally, the association between quality of life and PSS was detected. When inserting PSS as an independent variable and all patients’ functioning dimensions and symptoms as dependent variables, we found a negative significant association between levels of PSS from friends and patients’ physical functioning (β = .26, t = 2.78, p = .006). Specifically, negative significant association was found between PSS from friends and fatigue (β =.21, t = 2.24, p = .027), loss of appetite (β = .20t = 2.14, p = .035), and diarrhoea (β = .21, t = 2.26, p = .026). No other associations were found between PSS and the other evaluated types of functioning and symptoms. Relationships between quality of life and PSS are reported in Table 2. Figure 2 shows the overall main effects model.
4. Discussion
The present research was aimed to study the relationship between PSS derived from different sources and levels of individual well-being, in terms of illness perception, optimism, life satisfaction, and quality of life, reported by cancer patients in a cross-sectional measurement of psychological experiences.
Based on observed data, beliefs about cancer causation mainly concerned the environmental pollution and change or bad luck, whereas causes such as alcohol, smoking, personality, behaviour, emotional state, mental attitude, too much work, inadequate care in the past were not probably associated with the development of the disease. Accordingly, the attribution of illness cause seemed predominantly external. As a viable interpretation, cancer patients might employ a survival mechanism to defend themselves against self-blame as a means of coping with intolerable stress. As a clinical implication and according to previous research (Applebaum et al., 2014), paying strong attention to the causal attributions of the disease used by the patient could prevent perseverative and unproductive worry bouts and related mental health problems (Julkunen et al., 2009).
According to previous research (Applebaum et al., 2014; Jie et al., 2019; Lee et al., 2019; Pinar et al., 2012), and as stated by our early general hypothesis, we confirmed the expected associative links between PSS and the degree of well-being among cancer patients. However, according to a previous study (Pinar et al., 2012), we found that the various PSS sources had a different predictive role on the self-assessed well-being indicators.
As a practical implication, it is worth knowing about the supporting role of loved ones to improve psychological treatments oriented to an holistic approach of support. Further, according to recent studies (Fanakidou et al., 2018; Finck et al., 2018; Lee et al., 2019), and also in line with our initial hypothesis (H1), patients who perceived a higher social support from friends were more likely to perceive greater personal control over the disease, as well as increasing perception of disease coherence. Thus, our outcomes supported the previous evidences (Fanakidou et al., 2018), which highlighted the influence of friends in supporting cancer patients, especially referring to illness perception. As an implication, clinical interventions could be helpfully oriented to support human relationships and social contacting, discouraging social withdrawal. Instead, no associations were observed between PSS from other sources and illness perception indicators. As a possible explanation, both family and significant others could be perceived by cancer patients as an emotional retreat, while friends would be considered as belonging to a leisure context distracting from symptomatology and therapy.
In accordance with both prior literature (Bozo et al., 2009; Hodges & Winstanley, 2012; Applebaum et al., 2014; Finck et al., 2018; Shelby et al., 2008) and our derived hypothesis (H2), we found a positive relationship between PSS and optimism degree. Explicitly, patients who felt more support from family and friends showed a positive attitude towards the disease. As shown by some research (Hodges & Winstanley, 2012; Matthews & Cook, 2009), indeed, the perception of a usual reference network can improve the attitude towards life. Subsequently, this patients’ positive propensity could bring new social relationships since optimism is a socially approved behavior, eventually resulting in a positive circle of reciprocity. From clinical and prevention perspectives, these findings highlight the importance of fostering social connectedness and belongingness with others. Nevertheless, we did not find any association between PSS from significant other and optimism. In the light of the contradictory results, further investigations are required to deepen how the social network breadth, and available network players, would affect patients’ well-being.
Interestingly, we found a positive relationship between PSS from significant other and life satisfaction, whereas no other significant associations were observed with the two remaining PSS sources (i.e., family and friends). These results partially confirmed our early hypothesis (H3) and are in line with some research outcomes, revealing how people satisfied with their life did not show an imbalance between personal goals and current life conditions (Olsson et al., 2017). The proximity of a significant person could play a key role in one’s life satisfaction, especially during illness. However, previous studies (Bozo et al., 2009) did not show difference in the associations between life satisfaction and the different sources of PSS. Instead, our results highlighted the prevalent role of significant other among the social network players. Based on this empirical evidence, we argue the relevance of our findings for general clinical implications. Specifically, our results sustain the need of a wide adoption of a couple-focused approach into cancer care. Since the partner support could be a crucial resource for patients facing with a life-threatening disease, indeed, couple-based psychosocial interventions might be effective in reducing distress and enhance wellbeing during health care experiences and struggles.
Finally, according to previous studies (Pinar et al., 2012; Ng et al., 2015; Aydın Sayılan & Demir Do˘gan, 2020), and also in line with our initial hypothesis (H4), we found an inverse relationship between PSS from friends and quality of life referring to physical functioning. Precisely, our findings showed significant negative associations between PSS from friends and fatigue syndrome (Den Oudsten et al., 2010), loss of appetite, and diarrhoea, which were more frequently reported symptoms associated with cancer, especially during medical treatments (Prins et al., 2004; Eom et al., 2013; HamdanMansour et al., 2015). Patients often attributed this kind of symptomatology to cancer and not to any other medical comorbidities, as a sign of the pervasiveness of the disease in their lives. As a practical interpretation, friends -with their support and encouragement- could make a difference in patients’ perception of physical symptoms: their presence could be essential for creating recreational opportunities during the illness period. Despite some research showed how PSS from all kind of sources (Aydın Sayılan & Demir Dog˘an, 2020; Den Oudsten et al., 2010; Ng et al., 2015; Pinar et al., 2012) would improve patients’ physical functioning and quality of life, interestingly, we did not find significant relationships with family and significant other PSS. As a viable interpretation, friends might serve as a protective factor against symptoms development and relapse, since they can encourage patients to a more active and joyful life, directing them away from focusing on symptoms and pathology.
In conclusion, our findings suggested that the various sources of PSS might increase well-being in cancer patients. Nevertheless, it is worth noting that our findings are referred to the Italian context; outcomes could be changed in different countries or in various part of Italy (e.g., patients from individualistic culture could focus more on personal resources than those from collectivist culture). However, it is important to improve the attention on social networking in clinical setting: the consideration of the patients’ relationships could prevent the social isolation, activating social support networks, such as supportive groups. The health care practitioners could facilitate the relationship between patients and their families or between patients themselves, so as to have the health system paying attention not only to medical needs but also to psychological needs. In accordance with a biopsychosocial approach, the clinical care practices should not be addressed to the suffering individual, neglecting the relationships with those proving care and the social environment in which the individual is absorbed.
4.1 Study limitations
Some limitations of the current study should be noted. Although the prospective nature of the study offers more confidence that PSS is a valid predictor of psychological well-being in cancer patients, the cross-sectional nature of the data does not allow to determine causal links between the observed variables and raises the possibility that third factors may influence both PSS and selfreported well-being measures. Secondly, data were collected in a single hospital in Italy using a convenience sample. This screening of participants limits generalization of the results. Indeed, previous research (Jie et al., 2019; Pinar et al., 2012) showed that the cultural background can influence the patients’ beliefs and behaviours, how they perceive the disease, the resources they feel they have to cope with the disease, thus modulating the general attitude towards the disease. Indeed, the observed sample arrived at the hospital with various medical needs or treatments, which could have affected their approach and beliefs regarding the disease. The disabling treatments that some patients followed may have worsened psychological dimensions such as quality of life, the perception of illness, and optimism. We also were unable to identify the stages of disease since we did not consult the medical records, but we used the self-report assessment based on personal identification as “patients” and not patient/survival. This makes the results less comparable with previous research, especially from other country. Furthermore, due to the unequal distribution by gender and type of cancer, we were unable to investigate statistical comparisons.
5. Conclusions and Clinical Implications
Despite the above-mentioned limitations, this study may provide a contribution to the knowledge around the relationships between PSS and psychological well-being among cancer patients. Interestingly, our findings revealed a specific relevance of the various sources of perceived social support when associations with self-reported well-being measures were evaluated. Overall, based on our outcomes, cancer patients with higher levels of well-being perceived the proximity of loved ones. Distinctively, the perception of the support from significant others was related with patient’s life satisfaction, the perception of family support was associated with a positive attitude toward life, and the perceived support from friends was connected with higher levels of personal control, coherence of disease, optimism and physical quality of life.
As a clinical implication, our findings support the importance of examining the social context of cancer patients to increase their awareness of several possible resources, which might improve patients’ well-being and the opportunity for quality of life. The knowledge around the potential positive impact of loved ones could be addressed within psychological programs for couples, families, and groups. Thus, the care of the patients’ could be directed to combine medical and psychological treatment to enhance life satisfaction: a consciousness of the potential benefit of social support might help reduce the isolation resulting from illness.
Health care professionals should pay attention to the patient as a subject who is involved in a social and relational context for the purpose of improving his/her well-being during the illness experience. Among the network players, friends might act a significant protective role against symptoms perception and somatisation. It is also important that industry professionals (i.e., medical and health personnel) are sensitive to potential discrepancies between the experience, availability, and adequacy of social support. Accurate psychometric and clinical evaluations of the PSS are essential to prevent social isolation that can worsen the patients’ physical and psychological health. Future research should pay attention to other further sources of social support (e.g., medical staff, patients with the same illness experiences, supportive groups, other relatives) to increase the knowledge around the potential members of patients’ social network.