1. Introduction
The relationship betweenmental health and psychopathology has been deemed essential in the deepening of psychological mechanisms and processes related to psychopathological expressions and the evolutionary trajectories of such manifestations (Tortella et al., 2016). At this point, schizotypy stands out as one of the constructs on which there is still no definitive consensus (Suzuki et al., 2015).
In a framework of commonassociationbetweenschizotypal personality, schizotypal personality disorder (SPD), and schizophrenia spectrum disorders (SSD; Cheli et al., 2019), the possession of associated traits is considered at risk of developing SSD (Fonseca & Inchausti, 2018). This highlights the relevance of understanding all its dimensions, when it has been found overlapping of its features with others of a psychiatric and subclinical type (Zhang et al., 2019).
In the research carried out on the schizotypy construct, two marked lines can be seen: those of personality and clinical (Álvarez, 2005). From the analysis of personality, it is characterized in the types that fit within cluster A (APA, 2013), which present traits that are distinguished by strange behaviors, eccentricity, social withdrawal, and suspicion (Belloch and Fernández, 2010). In parallel, in the clinical approach, schizotypy comprises the correlational and probability terms towards the understanding of schizophrenia (Cabrera et al., 2017). The DSM5 classificatory model (APA, 2013) presents schizotypy as a personality type with its relative pathological expression. DeYoung et al. (2012) highlight the complexity of the construct, composed of multiple subfactors that probably come from different sources, and that sometimes present contradictory models. Thus, a global definition denotes schizotypy as a unifying construct, representing the underlying vulnerability of SSD psychopathology, and is expressed through a wide range of personality phenomenology and clinical parameters (Kwapil & Barrantes, 2014). However, there are still notable gaps, referring both to its correct definition and to the diagnostic and pathological implications (Fumero et al., 2017), which are able to recognize three characteristic domains used by various approaches, these are the negative/interpersonal, positive/cognitive, and disorganization.
Based on the above, the purpose of this study aims to synthesize the recent and high-quality empirical evidence, through the analysis and synthesis of the research works developed for the assessment of schizotypy, in order to respond to the difficulties in the replication and consolidation of empirical research results within psychology (Shrout & Rodgers, 2018).
2. Method
The following systematic review is consolidated on the quality of reporting based on the guidelinesof the PRISMA Systematic Review Reporting and Meta-Analysis Referred Submission (Liberati et al., 2009) and with an AMSTAR checklist (Shea et al., 2007) for the review articles used.
PRISMA method proposes an organization system in 4 stages: identification, screening, eligibility, and inclusion, which are reported through a flow chart, to guarantee transparency in the search and selection. In addition, it provides a list of criteria to structure the report (Liberati et al., 2009), complementing the AMSTAR checklist given the diversity of methodologies found. The lists also allowed us to examine the articles reviewed, as well as their methodology and quality.
Consequently, to maximize the breadth of the research, studies of both psychometric validation and other types of design were considered for review. Therefore, there were no specifiers of control/comparison conditions and studies were selected independently of this process. From the same intention, investigations were included without considering the temporal moments.
Criteria for the inclusion of studies imply: a) articles in English in an indexed journal reviewed by external peers published until September 2020; b) articles that identify with the keywords “schizotypy”, “assessment”, “clinical”, “psychometric”; c) articles with a sample defined by clinical, subclinical, and non-pathological participants; d) those that take into consideration at least one validated tool; e) articles that use healthy controls; f) those that reported an outcome measure designed to verify the schizotypy construct.
The exclusion criteria mainly comprised a) research papers that do not report their methodology, b) studies that exclusively comprised the child or adolescent population, c) undergraduate or undergraduate thesis, and d) single case studies or interviews with professionals.
The process of identification and selection of studies began with a search in the Web of Science databases, Scopus, PubMed, Taylor and Francis, Wiley, Science Direct, Google Schoolar, and PsycNet. As a result, an initial total of 9030 records was obtained through the keywords and using search commands. Similarly, after applying the first ten-year time filter (2010-2020), they were reduced to 5797. To those, a first screening was carried out, which resulted in 369 selected texts.
Later, a detailed individual review delimited 156 texts to the base articles. Through the selection criteria, as well as the review protocols and counting repeated records, 91 articles were discarded, concluding with a total of 65
Table 1 Search records
| Data Bases | First Registration | Last 10 years | Initial Selection | Criteria Inc/Ex |
| Web of Science | 499 | 225 | 73 | 44 |
| Scopus | 347 | 252 | 73 | 19 |
| PubMed | 73 | 52 | 30 | 23 |
| Taylor & Francis | 173 | 95 | 32 | 13 |
| Wiley | 266 | 141 | 25 | 11 |
| Science Direct | 721 | 411 | 45 | 21 |
| Google Schoolar | 6940 | 4610 | 85 | 23 |
| PsycNet | 11 | 11 | 6 | 2 |
| Total | 9030 | 5797 | 369 | 156 |
| Discarded∗ | 91 | |||
| Final Selection | 65 |
Note. Own elaboration. ∗After the last selection phase.
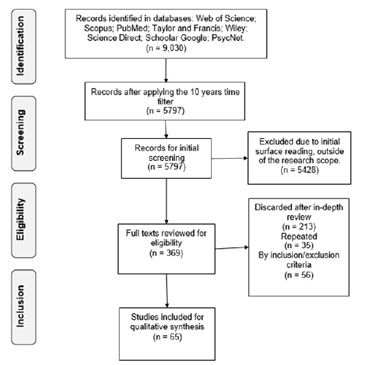
Note. Graphic model from Moher et al. (2009) in Preferred Reporting Items for Systematic Reviews and MetaAnalyses
Figure 1 PRISMA flow chart for file identification and selection
articles selected for the final review and information synthesis. The selection by databases is detailed in Table 1.
Finally, a list of selected studies was compiled, from which, after an in-depth individual review, the relevant information was extracted using a data extraction protocol (reading sheet). The information synthesis was carried out according to thematic axes on which the results section is organized. The PRISMA flow chart is illustrated in Figure 1.
3. Results
Given the plurality of research methodologies found, it is necessary to establish generalities about the group of articles reviewed. The methods chosen to evaluate the construct show a variety of designs: proposal of new tools, validation of pre-existing models, and correlational proposals to cement a multidimensional model. This disintegration of methodologies could be representative of the lack of consensus when defining this issue (Kwapil & Barrantes, 2014).
Another remarkable characteristic is the predominance of the use of large university populations or young adults. In contrast, those with small samples used clinical, psychometrically delimited or extreme group populations, using control groups (Mason, 2015). The university characterization implies limitations when generalizing the results and on their ecological validity (Ragsdale & Bedwel, 2013).
Those designs with university groups respond to what could be called large-scale epidemiological research (Mason, 2015); from the same groups more delimited secondary investigations appear, ranging from subclinical samples to designs with extreme groups (Kocsis et al., 2017). In this sense, the publications reflect segments in the research projects, evidencing research teams in specific regions (Debbané & Mohr, 2015; Giakoumaki, 2016). A generalized naming of the articles reviewed is summarized in Table 2.
Basic theories vary between the clinical and personality approaches (Mason, 2015); they also highlight attempts to unify both current (Debbané & Mohr, 2015) and multidimensional procedures (Gross et al., 2018; Kemp et al., 2019; Kwapil et al., 2018). In addition to the motivation to reach a definition (Mason, 2015), there are works that study the relationships of the construct with other phenomena (Haslam et al., 2019; Siddi et al., 2017), mainly towards the role it manifests in the risk to SSD (Bora et al., 2014).
The latter highlights that the approach from schizotypy opens the doors to low-cost, high-benefit research (Kline & Schiffman, 2014), since the use of subclinical and non-pathological populations has cemented advances for research on clinical, factorial fronts, risk, cognitive, brain structure, and even genetic factors of schizophrenia (Lawrie et al., 2011).
Using terminology found in Kwapil and Barrantes (2014), the results will be classified as psychometric tools, which define schizotypy in three main dimensions; personality tools, which integrate normal and pathological personality models; and clinical tools, focused on the expression of symptoms or clinical correlates. This classification is not representative of the basic theories, since certain protocols follow from the same theoretical frameworks.
3.1 Psychometric Definition Tools
The psychometric proposal in the reviewed research sample is made up of evaluations with a factorial structure, characterized by three dimensions: positive, negative, and disorganized (Oezgen & Grant, (2018). These tools represent the backbone in terms of construct assessment (Mason, 2015). Mainly highlighting the Schizotypal Personality Questionnaire (SPQ; Raine, 1991), the Wisconsin Schizotypy Scales (WSS; Winterstein et al., 2011) and the Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE; Mason et al., 1995).
Specifically, predominance of the SPQ stands out, as it is used in more than half of the researches reviewed, and it has a wide acceptance in clinical, subclinical, and general populations (Torbet et al., 2015) that extends to its short versions SPQ-B, SPQ-BR (Callaway et al., 2014; Mitchell and Cohen, 2017), demonstrating capacity of adaptation to the advances of current models, such as the DC-SPQ structure developed for DSM 5 (Xi, et al., 2019).
From a factor analysis between these instruments, it is possible to establish a common framework and make accurate comparisons of the positive and negative dimensions (Gross et al., 2014), with reported ecological validity (Kwapil et al., 2012). In contrast, ambiguity is found when dealing with disorganization, as there is no consensus on its constituent features. This implies that there is no complete unit in the construct and the results may vary by tool (Oezgen & Grant, 2018).
A need for these dimensions to be differentiated when evaluated is emphasized (Barrantes et al., 2013), being disorganization the weak point when using these tools, mainly internationally and in various languages (Kocsis et al., 2016). The differential functioning of the items may lose validity when comparing multiethnic samples, as some even cancel each other out (Cicero et al., 2017).
In contrast, the SPQ-B, in a transnational internal structure validation process, integrated results from 14 countries, corroborating the three-factor structure on a large scale; it showed levels of invariance in the configurable measurement, although its quality varied between samples (Fonseca-Pedrero et al., 2018).
Although the development of these psychometric tools found a kind of zenith decades ago, their status has been relegated by more precise and reliable biological and neurological tests (Cicero et al., 2019), especially when evaluating the risk of psychosis (Moritz et al., 2019). Therefore, additional measures and protocols have been designed and validated in an attempt to establish a more complete framework (Kemp et al., 2020), since their results can be contrasted with other measures referred to here as clinical and personality measures (Ragsdale & Bedwel., 2013).
Table 2 General characteristics of the articles reviewed
| Authors and year | Schizotypy Tools | Population | Sample | Control | Method | ||
| C | A | M | |||||
| Ashton et al., 2012 | PID-5; HEXACO-PI-R; NEO-PI-3 | University students | 378 | × | × | × | |
| Badcock, 2016 | WSS | University students | 551 | × | × | × | |
| Barrantes et al., 2013 | WSS | Young adults | 206 | × | × | × | |
| Blanchard et al., 2011 | IPDE; SDS; GAF | Community | 86 | 86 | × | × | × |
| Brosey & Woodward, 2015 | SPQ; PANS; WSS | Schizophrenics | 68 | 59 | × | × | × |
| Burgin et al., 2014 | WSS; SAS | University students | 430 | × | × | × | |
| Callaway et al., 2014 | SPQBR | University students | 1279 | × | × | × | |
| Campellone et al., 2016 | CAINS | University students | 31 | 24 | × | × | × |
| Cicero et al., 2014 | SIPS, WSS | University students | 160 | × | × | × | |
| Cicero et al., 2017 | WSS and WSS-B | University students | 1056 | × | × | × | |
| Cicero et al., 2019 | SPQ; WSS | Schizophrenics | 288 | 257 | × | × | × |
| Cohen et al., 2011 | SPQ-B; ESAS; | Schizotypal | 71 | 32 | × | × | × |
| Chan et al., 2010 | SPQ; CNI | Schizotypal | 64 | 60 | × | × | × |
| Chan et al., 2019 | SPQ; SIDP | Schizotypal | 250 | 116 | × | × | × |
| Dembińska & Rybakowski 2016 | O-LIFE | Schizophrenics | 167 | × | × | × | |
| Deyo & Langton, 2019 | SPQ | Young adults | 92 | × | × | × | |
| Edmundson et al., 2011 | STPT; SPQ; WISPI; FFSI | University students | 286 | × | × | × | |
| Everett & Linscot, 2015 | WSS, GAF | Psychiatric | 109 | × | × | × | |
| Fluckiger et al., 2019 | WSS | Risk of psychosis | 277 | × | × | × | |
| Fonseca et al., 2018 | SPQ-B | General | 28426 | × | × | × | |
| Giakoumaki et al., 2016 | SPQ; TCIR; PANS; CFQ | Adults | 483 | × | × | × | |
| Gross et al., 2014 | SPQ; WSS | Young adults | 1445 | × | × | × | |
| Gross et al., 2018 | MSS-B; SPQ-B; NEO-FFI | University students | 2719 | × | × | × | |
| Janssens et al., 2016 | CAPE | Family | 703 | 428 | × | × | × |
| Karagiannopoulou et al., 2016 | SPQ | Healthy adults | 200 | × | × | × | |
| Kemp et al., 2019 | MSS; MSS-B | Young adults | 318 | × | × | × | |
| Kemp et al., 2020 | MSS | Young adults | 177 | × | × | × | |
| Kline et al., 2012 | SPQ-B; PQ-B | University students | 355 | × | × | × | |
| Kocsis et al., 2016 | O-LIFE; SANS; SAPS | Schizophrenics | 102 | 29 | × | × | × |
| Kocsis et al., 2017 | SPQ; MASC | Schizotypal | 39 | 47 | × | × | × |
| Kotlicka et al., 2019 | PSST | Family | 107 | × | × | × | |
| Kwapil et al., 2012 | WSS; ESM | Young adults | 412 | × | × | × | |
| Kwapil et al., 2013 | WSS; SADS-L | Schizotypal | 534 | × | × | × | |
| Kwapil et al., 2018 | MSS | University students | 6265 | × | × | × | |
| Li et al., 2020 | MSS | Multiétnica | 2198 | × | × | × | |
| Lin et al., 2013 | O-LIFE | Risk of psychosis | 228 | × | × | × | |
| Linscott et al., 2017 | CAPE | Family | 792 | × | × | × | |
| Mitchell & Cohen, 2017 | SPQ-BR | University students | 137 | × | × | × | |
| Moritz et al., 2019 | SPQ; WSS; MID; STA | Psychiatric | 90 | × | × | × | |
| Nenadic et al., 2015 | SPQ; CAPE | Healthy adults | 59 | × | × | × | |
| Nitzburg et al., 2013 | CAPE; TCI | Healthy adults | 415 | × | × | × | |
| Oezgen and Grant., 2018 | SPQ; WSS; O-LIFE | Healthy adults | 327 | × | × | × | |
| Rabin et al., 2014 | O-LIFE; PANS | Schizophrenics | 39 | × | × | × | |
| Ragsdale & Bedwel, 2013 | SPQ; PPI-R | University students | 212 | × | × | × | |
| Shanon et al., 2014 | SPQ; BACS | Risk of psychosis | 72 | 80 | × | × | × |
| Soler et al., 2017 | SIS-R | Patient & family | 30 | 82 | × | × | × |
| Somma et al., 2019 | SPQ; STA, PID-5 | University students | 1056 | × | × | × | |
| Torbet et al., 2015 | SPQ; EASE | Schizotypal | 30 | 20 | × | × | × |
| Torti et al., 2013 | SWAP-200 | Patients & relatives | 43 | 23 | × | × | × |
| Trask et al., 2019 | WSS | Schizotypal | 112 | 41 | × | × | × |
| Van den Berg et al., 2013 | CAPE; SIS-R | Family | 747 | 341 | × | × | × |
| Wang et al., 2014 | SPQ; PANS | Schizophrenics & Schizotypal | 84.84 | 84 | × | × | × |
| Xi et al., 2019 | SPQ-DC | University students | 980 | × | × | × | |
| Zouraraki et al., 2017 | SPQ | Family | 115 | 112 | × | × | × |
| Bora et al., 2014 | Meta-analysis | Clinic & cognition | 2113 | 1748 | × | × | × |
| Bora, 2020 | Meta-analysis | Theory of mind | 24 | × | × | × | |
| Chau et al., 2019 | Meta-analysis | Continuum | 15 | × | × | × | |
| Haslam et al., 2019 | Meta-analysis | Taxometric | × | × | × | ||
| Siddi et al., 2017 | Meta-analysis | Cognitive deficits | 67 | × | × | × | |
| Kline & Schiffman, 2014 | Review | Risk of psychosis | × | × | × | ||
| Kwapil & Barrantes, 2014 | Review | Dimensionality | × | × | × | ||
| Debbané et al., 2014 | Review | Risk of psychosis | × | × | × | ||
| Mason et al., 2015 | Review | Clinical evaluation | × | × | × | ||
| Giakoumaki, 2016 | Review | Dimensionality | × | × | × | ||
| Nelson et al., 2013 | Review | Dimensionality | × | × | × | ||
Note. Wisconsin Schizotypy Scales (WSS, WSS-B), Schizotypal Personality Questionnaire (SPQ; SPQ-B; SPQBR; SPQ-DC), Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE; O-LIFE-B), Assessment of Negative Symptoms (SANS), and Positive Symptoms (SAPS) Multidimensional Schizotypal Scale (MSS). Personality Inventory DSM5 (PID5) HEXACO-Revised Personality Inventory (HEXACO-PI-R,) Personality Inventory (NEO-PI), International Examination of Personality Disorders (IPDE), Global Evaluation of Functioning Scale (GAF), Interview Clinical Evaluation of Symptoms Negative (CAINS), Five Factor Schizotypal Inventory (FFSI), Wisconsin Personality Disorders Inventory (WISPI), Explicit Social Attitudes Scale (ESAS), Marlowe-Crowne Social Desirability Scale (SDSM-C), Structured Interview for DSM-IV Personality Disorders (SIDP), Community Assessment of Psychic Experiences (CAPE), Program for Affective Disorders and Schizophrenia (SADS-L), Premorbid Schizotypal Traits Assessment Scale (PSST), Anomalous Self-Experience Test (EASE), Shedler-Westen Personality Assessment (SWAP-200), Structured Interview for Schizotypy revised (SIS-R), Psychopathic Personality Inventory-Revised (PPI-R), Brief Prodromal Questionnaire (PQ B), and Structured Interview for Prodromal Syndromes (SIPS); Method: C=quantitative approach; A=reports a statistical analysis; M=evidence of some measure of Validity. Own elaboration.
3.2 Personality tools
Personality approaches respond to the study of temperament and character patterns associated with schizotypal traits in healthy populations. Furthermore, they address how these patterns interact with other variables (Nitzburg et al., 2013), defining a personality structure independent of pathologies (Deyo & Langton, 2019), in addition to the own specification of TPE (Chan et al., 2019).
Some relevant approaches respond to the five-factor model (FFM; Edmundson et al., 2011) and the six dimensions of HEXACO (Ashton et al., 2012); the model of personality disorders presented in the DSM5 is also considered (Somma et al., 2019) or previous derivatives, such as the structured interview of the DSM-IV (SIDP, Chan et al., 2019). Usually, other tools are used due to the incomplete measurement capacity compared to current theoretical models (Ashton et al., 2012).
Consequently, as a personality structure, schizotypy presents various features depending on the model taken, given its heterogeneity and overlap with other phenomena. Therefore, the study of personality by trait becomes fundamental (Cicero et al., 2019). Only with a specific definition of trait, the evaluation criteria for the TPE obtain internal consistency and discriminant validity, and can establish a bridge between normal and pathological (Edmundson et al., 2011).
To define personality disorders, the gold standard seems to be the clinical qualification through structured interviews. However, when trying to correlate them to cognitive or biological factors, the results vary depending on the tool used (Deyo & Langton, 2019). Therefore, the evaluation of schizotypal traits should include selfreport measures, as a complement to interviews rated by clinical criteria (Chan et al., 2019; Torti et al., 2013).
Finally, the dynamic nature of personality traits should be noted, including the decline in TPE symptoms during development in young adulthood (Blanchard et al., 2011). The alternative model for personality disorders is effectively articulated with the complementary use of psychometric and personality tools (Somma et al., 2019).
3.3 Clinical Definition Tools
These scales can be defined as symptomatological, which provide complementary accesses and allow the elaboration of correlates with cognitive and affective parameters (Siddi et al., 2017), which are relevant aspects within the constitution of the schizotypal experience (Bora et al., 2014) and associated neuropsychological functions (Siddi et al., 2017).
From these functions, cognitive deficits that characterize the different schizotypal dimensions are identified. For example, impairment of the shift in attention and working memory in paranoid negative and positive schizotypy, in addition to reduced performance in tasks that require frontotemporal connectivity (Karagiannopoulou et al., 2016; Kocsis et al., 2017; Rabin et al., 2014).
From the perception of cognitive functionality, clear relationships can be established between cognitive experience and clinical states. Individuals with schizotypy as a trait presented cognitive abnormalities in certain domains, which are markedly intensified in individuals at high risk for SSD (Shanon et al., 2014; Fluckiger et al., 2019).
Specifically, deficiencies in planning, problem solving, strategy formation, and working memory are central to the entire spectrum of schizophrenia. Greater difficulties in executive working memory and verbal fluency are associated with paranoid and negative schizotypy (Mitchell & Cohen, 2017; Zouraraki et al., 2017). Additionally, high-trait individuals show greater decreases in performance as the information processing load increases (Shanon et al., 2014).
In extreme groups, it is highlighted that high levels of psychometric schizotypy are equated with high clinical levels. Although, these tests imply a specific sensitivity to cognitive deficiencies that can translate nonsignificant results for the clinic (Shanon et al., 2014). Thus, this high-risk clinical approach is obstructed by a notable presence of false positives that would hinder an effective approach.
Understanding that schizotypy responds mainly to a construct in research, the development of a comprehensive framework could correct these shortcomings at the time of establishing specifically in the clinic (Cícero et al., 2014). Another viable alternative can be the analysis of the content of the discourse, mainly in a population with experiences close to schizophrenia (Trask et al., 2019).
Cognitive depressive symptoms can explain motivations and impairment of pleasure in a population at risk of SSD. Individuals with a high degree of schizotypy report being less emotionally expressive, although their behavior appears to be as expressive as that of subjects with a low degree (Campellone et al., 2016). Given the discrepancies between self-report and behavior, affective deficits in schizotypy may reflect deliberative processes rather than implicit/automatic (Cohen et al., 2011).
Other variables of an emotional nature have been identified as conceptually independent. For example, loneliness represents a variable related but not completely inherent to schizotypy (Badcock et al., 2016). Before this, the independent aspects of each correlate must be considered, since its implications can modulate the way in which we access these clinical notions.
3.4 The Continuum of Psychosis
A notion of origin for the creation of the schizotypy construct is its remarkable relationship with psychosis, currently SSD (APA, 2013). Formulating itself as a previous step to psychosis implies a continuous composition (Debbané et al., 2014). In longitudinal data, the dimensions of schizotypy and its enduring traits significantly predicted the development of SSD, psychotic symptoms, and poor adaptation (Kwapil et al., 2013; Kotlicka et al., 2019). Psychometric tools can be used to carry out an effective screening on the risk and development of pathology (Kline & Schiffman, 2014; Rabin et al., 2014).
Several biological and neurological tools have shown great precision in identifying relationships between brain structure, schizotypy, and the development of SSD (Nenadic et al., 2015). Genetic (Janssens et al. 2016), biological (Cicero et al., 2019) and environmental/familial (Soler et al., 2017) risk factor effects are more likely to be combined with high schizotypy in various cumulative and nonlinear knowledge to determine such a result (Kline & Schiffman, 2014).
Specifically, the bridge between schizotypy and schizophrenia can be explained from the Propensity-PersistenceImpairment (PPD) model that establishes how the psychotic and pseudo-psychotic experiences of schizotypy are more likely to lead to impairment when its expression becomes persistent, which indicates a higher risk of SSD (Janssens et al., 2016; Chau et al., 2019). Schizotype as a range within this continuum finds its value insofar as it contemplates the “normal” human experience, and the midpoints between health and dysfunction (Kline & Schiffman, 2014).
3.5 Taxonomy and Dimensionality
One of the main debates regarding the definition of the construct has been the question of dimensionality vs. categorization. Meehl’s (1992) taxonomic model sought to establish categorical principles in the distinction between the pathological and the normal (Haslam et al., 2020). However, taxonomic findings are scarcely reported in psychopathology and are practically nonexistent in personality (Haslam, 2019).
Since taxonomic findings represent complex processes and much of the taxometric research does not support the presence of a taxon, dimensional results are almost five times more likely (Haslam et al., 2020). Consequently, meta-analytic results have not found evidence that supports latent structures; on the contrary, taxonomic reports seem to blur the idea of a structure that supports categorical distinctions (Rosenström et al., 2019).
In any case, the developments in taxometric identification cannot be ignored, as the field still requires refinement and maintains options for its development (Everett & Linscot, 2015). It is also not ruled out that taxonomy can be integrated into a dimensional and continuous psychosis phenotype (Linscott et al., 2017). Ultimately, the evidence seems to favor schizotypy as a dimensional construct (Haslam et al., 2020).
3.6 Multidimensional Model
Multidimensional profiles have been used to understand the influence of schizotypy on affect, cognition, and schizophrenia (Giakoumaki et al., 2016). Scale scores are incomplete when traits are not compared, since a measure of schizotypy is represented by a generalized disposition (Van den Berg et al., 2013). Single-factor models of the scale versions may fail to fit their data based on fit statistics (Cícero et al., 2017).
The term multidimensionality does not represent a new advance. It can be evidenced through the Multidimensional Questionnaire of Schizotypal Traits (MSTQ; Rawlings & Macfarlane, 1994) or in tools such as OLIFE, which are defined as multidimensional and found operability when establishing cognitive correlates (Álvarez, 2005), but lack a complete and up-to-date rationale (Janssens et al., 2016).
This way, the development of the Multidimensional Schizotypy Scale (MSS; Kwapil et al., 2018) and its short version (MSS-B; Gross et al., 2018) are collected, which is based on current conceptual models that take advantage of the positive, negative, and disorganized dimensions; therefore, combining consolidated factors of the SPQ, WSS, and O-LIFE scales, and integrating new characteristics such as experiences of suspicion, passivity, lack of volition, allegiance, and flattened affect (Kwapil et al., 2018; Gross et al., 2018; Kemp et al., 2019; Li et al., 2020).
In conclusion, although the reports show good reliability for MSS and MSS-B (Kemp et al., 2019), even in different ethnic groups (Li et al., 2020), these results are initial, and have pending to reach levels of validation at the time of correlating their results, expanding to crosscultural samples and that their use becomes generalized as that of the tools on which they are based.
3.7 Clinical Implications
The research results highlight how the findings in this field imply important parameters for the clinic. These relationships include cognitive, functional, affective, family, and social parameters (Barrantes et al., 2013; Brosey & Woodward, 2015; Kwapil et al., 2013; Shanon et al., 2014; Wang et al., 2014). Also, some data suggest comorbidity with other mental pathologies (Dembin´ska & Rybakowski, 2016; Kline et al., 2012).
For example, the quality of interpersonal relationships appears to be protective against the risk of experiencing symptoms, it can act as a buffer against the development of SSD (Barrantes et al., 2013), and it is usually an indicator of the need for care (Lin et al., 2013). Decreasing pleasure experiences in the social environment can help in early identification in at-risk populations (Wang et al., 2014).
The use of preventive assessment tools in clinical settings can predict the possibility of psychotic transition (Kotlicka et al., 2019) and establish parameters of adaptation and functionality (Kwapil et al., 2013). Because of the way in which schizotypy and cognition are related, their evaluation can help establish differential diagnoses between different SSDs (Brosey & Woodward, 2015).
Those deficiencies related to schizotypal traits require individualized interventions, understanding that the three dimensions of schizotypy are related differently. Trait-specific intervention appears to improve outcomes in early intervention and functionality programs in individuals with SSD (Dembin´ska & Rybakowski, 2016; Zouraraki et al., 2017).
Each schizotypal dimension is differentially immersed in the expression and pathological experience; therefore, identifying its presence is not enough to establish clinical criteria. For example, as proposed by Kline et al. (2012), the anhedonia parameters that can modulate the type of interventions include the quantity, frequency, intensity, and persistence of these experiences. All this highlights the importance of a comprehensive evaluation in the multidimensional context and over time (Janssens et al., 2016).
4. Discussion
The development of the evaluation of the schizotypy construct during the last decade has implied the use of various methodologies and tools in order to achieve a greater understanding of the phenomenon. This research rescues how effective and valid measurement models were found, cementing consistent findings in the area, and also highlighting the need to adapt them to new theoretical and application advances.
In response to the research purpose, an updated definition of schizotypy can be formulated, specifying it as a multidimensional construct of personality and embedded within the continuum of psychosis. This complex character, although it brings controversies, allows the construct to be an extensive field for the development of research from psychometry, epidemiology, genetic studies, brain structure, and function.
The contribution of this review is to provide an updated and integrative overview of schizotypy from the psychometric tools that have studied it in recent years, and it has found in its results important advances in the study and definition of the construct from the psychometric, the personality, and the clinical, trying to provide a wellfounded and transparent image of the scope of the current literature, which serves as a platform for future advances.
Furthermore, the advances found in psychometry are expressed in terms of its capacity for the assessment and establishment of a behavioral phenotype, which is an essential component for neuroscience, biological psychology, and psychiatry. Schizotype questionnaires offer promising tools for identifying traits and the risk of developing SSD, as well as expanding phenotypic identification beyond the limits of diagnostic categorization.
Although it has been possible to draw some guidelines for the clinic, the research reports express them with due caution. This implies a challenge in the generation of data that can be translated to the clinic. Additionally, the use of large university samples and small high-risk groups, as well as the fact that quality research is limited to certain geographic spaces, imply local challenges for the development of the construct, not only in terms of converting the results to own, but also because of the wealth of information that diversity can imply for the field in general. One of the limitations of this review is the exclusion of research with adolescents, which represents a wide body of work that is undoubtedly key to understanding the construct from its origin and development. By focusing on the definition of the construct, adolescents were outside the scope of this article, but they represent an important resource that could be integrated into future research.
Accordingly, future lines of research can be established: in the first place, the importance of choosing the right tools, understanding the complexity and multidimensionality of the construct, and taking advantage of the complementary capacity between them; secondly, even with the considerable amount of research already produced, there are still gaps, contradictions, and undefined margins, which require the expansion of the capacity to conceptualize and measure this phenomenon.
Additionally, it is necessary to generate new research that manages to connect the contributions previously formulated, giving them relevance when evaluating, approaching, and intervening in individuals in the clinical, subclinical, and non-pathological ranges. This can occur in the formulation of protocols for prevention and intervention, or when complementing existing resources with the new discoveries achieved.
Finally, it is worth highlighting the usefulness of psychometry for schizotypy in other fields related to mental health such as psychiatry, neurology, and even those related to the well-being of the individual and their relationship with the world. The approach to such complex and intricate phenomena requires interdisciplinary articulations to achieve scientific production that fully understands them.














