1. Introduction
It is estimated that approximately 20% of the world’s population experiences chronic pain (Eccleston et al., 2017). In Europe, the prevalence is 19% (Breivik et al., 2006), while in Spain the rate is 16.6% (Dueñas et al., 2015). Chronic pain has significant repercussions on daily, family, social, and occupational life (De Sola et al., 2016), as well as on emotional wellbeing (Miller & Kaiser, 2018). Chronic pain is associated with the onset of psychopathology, especially depressive and anxiety disorders, and to a lower quality of life (Arango Dávila & Rincón-Hoyos, 2018; Failde et al., 2018; Pérez et al., 2017; Turk et al., 2016), factors that, in turn, maintain and aggravate chronic pain (Vlaeyen et al., 2016). Chronic pain affects medical care, increases disability (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018) and, consequently, affects the economy (Caramés-Álvarez & Navarro-Ribero, 2016; Rice et al., 2016). The personal impact will depend on pain severity and duration and the individual’s attitude (Martucci, 2020), given that coping methods for chronic pain are significantly related to the individual’s psychopathological condition and the influence of their personality (Dixon-Gordon et al., 2018; Ibrahim et al., 2020; Naylor et al., 2017; Vachon-Presseau et al., 2019; Weisberg, 2000).
Chronic pain is defined as that which lasts more than three months or persists for longer than a month after the remission of the initial cause or repeats intermittently over the course of months or years or is associated with chronic diseases or lesions (Bonica, 1953). Taking into account the underlying pathophysiology, chronic nononcologic pain can be nociceptive or neuropathic. Nociceptive pain is caused by the activation of nociceptors (receptors that detect pain sensations caused by tissue damage and transmit the signals to the central nervous system). Nociceptive receptors activate in response to an adverse stimulus, which can be secondary to an injury, disease, inflammation, infection or surgery (Treede et al., 2019). Neuropathic pain occurs as the direct consequence of an injury or disease affecting the somatosensory system (processing circuit structures for tactile, position, pain, and temperature stimuli; Scholz et al., 2019). This impairment hinders treatment, either due to a lack of response or low tolerance to drugs, increasing healthcare costs and the severity of the clinical condition in the presence of neuropathy (Failde et al., 2018; Finnerup et al., 2016; Pérez et al., 2017; Scholz et al., 2019).
Patients with chronic pain actively attempt to adapt to the pain, developing cognitive and behavioral patterns in response to pain. After repeated failed attempts, they feel incapable of generating new resolutive styles by themselves, which leads to a cycle of pain, subjective discomfort, despondency, anxiety, feelings of disability, lack of self-efficacy, reassessment of possibilities and self-concept, negative thoughts, limiting beliefs, defenselessness, exhaustion, and fear (Arango-Dávila & Rincón Hoyos, 2018; D’ippolito et al., 2020; Edwards et al., 2016). The type of strategies and skills for facing stressful situations are influenced by each individual’s personality (Dixon-Gordon et al., 2018; Lennox Thompson et al., 2020; Torres, 2018; Williams et al., 2020), which, in turn, can be affected by the chronic pain itself (Kato et al., 2017; Millon & Davis, 1998; Naylor et al., 2017). The traits and personality patterns when faced with a continuous stressor, in this case chronic pain, create less adaptive responses, boosting each other (Shapiro et al., 2020) and not only jeopardizing the clinical prognosis but also affecting numerous areas of life (Galli et al., 2021).
In the population that experiences chronic pain, the diagnosis rates for depression, major depression, panic attacks, and generalized anxiety disorder are 20%-94%, 20%-30%, and 19%-30%, respectively, and 30%-93% present anxiety symptoms (Arango-Dávila & RincónHoyos, 2018; Dueñas et al., 2015; Pérez et al., 2017; Velly & Mohit, 2018). In pain treatment units (PTUs), depressive disorders are typically detected in more than half of patients, tripling the rate of patients with anxiety in the general population (Turk et al., 2016; Velly & Mohit, 2018), especially for chronic pain that progresses with neuropathy (Colloca et al., 2017; Failde et al., 2018; Finnerup et al., 2016; Park et al., 2020).
Depressive comorbidity in chronic pain impacts the use of strategies for improving the painful process by generating a negative outlook on oneself, others, and the future, especially regarding disability (Velly & Mohit, 2018), given that chronic pain entails greater severity, pain perception and catastrophic and negative thinking, along with less self-control and increased risk of insomnia, suicide, and substance abuse (Baastrup et al., 2016). In the same bidirectional dynamic, comorbid anxiety maintains and boosts chronic pain by increasing muscle tension and raising the self-perception of pain and, in conjunction, its intensity (Arango-Dávila & RincónHoyos, 2018; Lanzara et al., 2020). Both comorbidities are related to low treatment compliance and reduced daily activity (Baastrup et al., 2016; Dippolito et al., 2020; Edwards et al., 2016; Lanzara et al., 2020; Turk et al., 2016), and their presence is a significant determinant of chronic pain-related disability (Palomo-Osuna et al., 2021; Turk et al., 2016). In comparative analyses between chronic nociceptive and neuropathic pain, patients who progress with neuropathy usually show a higher prevalence of psychopathology (Colloca et al., 2017; Failde et al., 2018; Finnerup et al., 2016; Park et al., 2020; Pérez et al., 2017; Scholz et al., 2019).
Depressive, evitative, anxious, introverted, alarmist, and hypochondriac patterns are frequently observed in patients with chronic pain, all characteristics resulting from a high avoidance of harm and low self-directedness, associated with cluster C anxiety-type personality disorders and with greater vulnerability to depressive and anxiety comorbidity (Gustin et al., 2015; Kato et al., 2017; Naylor et al., 2017). In PTUs, approximately 90% of patients have maladaptive scores in one or more personality patterns, with compulsive, dependent, histrionic, and schizoid types the most common (Chang et al., 2017; González et al., 2007; Ibrahim et al., 2020; Soriano & Monsalve, 2018). In addition, greater severity has been reported with the neuropathic component (Aho et al., 2022), with personality disorder rates of up to 30% and higher scores in depressive, borderline, antisocial (Campbell et al., 2015; Park et al., 2020; Yang et al., 2019), paranoid, evitative (Tutoglu et al., 2015) and, in cases of incapacitating chronic neuropathic pain, narcissistic personality patterns with thought and dysthymia disorders (Ajo et al., 2020).
There are currently difficulties in addressing the complexity represented by the confluence of these conditions. Often, psychological interventions are established after failing to consider the psychological and personality factors (Naylor et al., 2017), which are essential in interpreting and processing painful experiences. There is an increasing need to comprehensively analyze these constructs when evaluating patients with chronic pain to individually plan the treatment (Colloca et al., 2017; Eccleston & Crombez, 2017; Edwards et al., 2016; Galli et al., 2021; Ibrahim et al., 2020; Obbarius et al., 2020).
The main objective of this study is to identify and outline the psychopathological and personality aspects of patients with chronic non-oncologic pain (nociceptive and with a neuropathic component) from a PTU and their association with the pain type, intensity, and progression time.
The secondary objective is to compare and determine whether there are substantial differences that could explain the greater severity in the presence of the neuropathic component. Under the hypotheses H1) the longer the pain progression time, the greater the pain intensity; H2) the greater the intensity and the longer the progression time, the greater the psychopathological and personality impairment; and H3) in the presence of the neuropathic component, there is greater pain intensity and psychopathological and personality impairment than in nociceptive pain.
2. Methods
2.1. Design
A cross-sectional, descriptive, and comparative study, with systematic randomized sampling, was conducted in the PTU of Hospital Universitari Sagrat Cor (HUSC). The 2016/63-ANE-HUSC protocol was approved by Comité Ético de Investigación Clínica idcsalud in Catalonia in the proceedings of n◦23/2016 and was designed in compliance with the ethical principles of the Declaration of Helsinki and Organic Law 3/2018, of 5 December on Personal Data Protection and the guarantee of digital rights (OLDP-GDR). Written informed consent was obtained from all surveyed patients.
2.2. Participants
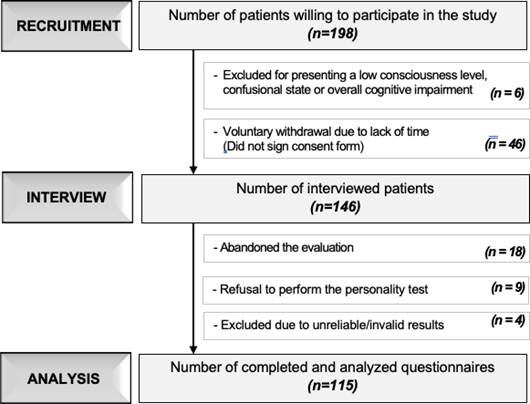
We used the Granmo calculator (IMIM et al., 2012) to calculate the sample size, considering the following parameters: a prevalence of chronic pain of 80% in the patients who attended the PTU of HUSC (5100 consultations/year) with a 5% error and a 90% confidence interval, resulting in a sample of 169 individuals. Of the 198 recruited patients, 146 continued to the evaluation phase, and the final study sample ultimately consisted of 115 patients (Figure 1). The inclusion criteria were a previous diagnosis by the PTU of chronic nononcologic pain (Treede et al., 2019), an age greater than 18 years, and the ability to consent. The exclusion criteria were the presence of pain with oncologic characteristics, refusal to sign the consent form, language barriers and cognitive problems, and comprehension, expression or consciousness problems that could affect the data collection or the proper implementation of the questionnaires.
2.3. Instruments
We collected demographic data regarding sex, age, employment status, educational level, and marital status. We also collected clinical data regarding the progression of the pain. Subsequently, the psychology general practitioner administered the following tools:
Douleur Neuropathique 4 (DN4) questionnaire for detecting neuropathic pain (short version) (Bouhassira et al., 2005), a self-administered test that identifies the presence of the neuropathic component of pain. DN4 contains 10 items with “yes/no” responses on the characteristics of the pain. The score consists of the sum of the responses; scores 3 are considered indicative of the presence of neuropathy. The questionnaire has been validated in the Spanish population, with 83% sensitivity and 90% specificity (Perez et al., 2007).
Verbal numerical rating scale (vNRS) (Downie et al., 1978), a professionally administeredapplication, employed to quantify the perceived pain intensity (from 0 to 10, with 0 = no pain and 10 = the worst pain imaginable), considering scores ≤3 as mild pain, 4-6 as moderate pain, and ≥7 as severe pain. The scale presents minimal adaptation and translation difficulties, is applicable to most of the population, shows high test-retest reliability (.96-.95), and has good correlation (≥0.7) with the visual analog scale (Hawker et al., 2011; Jensen et al., 2019).
Hamilton Depression Rating Scale (HAM-D) (Hamilton, 1960): Mixed application. We used this scale to assess the profile and the depressive symptom severity, categorizing 0-7 as no depression, 8-12 as minor depression, 13-17 as less than major depression, 18-29 as major depression, and 30-52 as more than major depression. Scores between 0-7 are expected for the general population, and scores ≥18 are regarded as indicating the presence of psychopathology. The Spanish version (Ramos Brieva & Cordero, 1988) has good internal consistency (.74-.76) and test-retest reliability (.92-.93), both in hospitalized populations and in the outpatient setting (Bobes et al., 2003).
Hamilton Anxiety Rating Scale (HAM-A) (Hamilton, 1959): Mixed application. Used to assess anxiety symptoms, categorizing 0-5 as the absence of anxiety, 6-14 as minor/mild anxiety, and ≥15 as moderate/severe anxiety. Scores between 0-5 are expected for the general population. The scale has been adapted and validated in Spanish and has good internal consistency (.89), test-retest reliability (.92), and convergent validity with HAM-D (Lobo et al., 2002).
Millon Clinical Multiaxial Inventory III (MCMI-III 4th) (Millon et al., 2009): Self-administered. Provides information on personality and psychopathology patterns (corresponding to disorders of the Diagnostic and Statistical Manual of Mental Disorders [DSM]-IV, DSM-IV-R and DSM-V). The scores are classified as results similar to those of the general population (0-34), low (35- 59), suggestive of presenting the syndrome/trait (60-74), presence of the syndrome/trait (75-84) or prominence of the syndrome/trait (85-115), the latter 2 groups being the instrument’s cutoff (±75-115). The adaptation and assessment to Spanish (Cardenal & Sánchez, 2007) has optimal psychometric properties in terms of reliability for the scales of personality (.66-.89), syndromes (.71-.90), test-retest values (0.840.96), internal consistencym(> .80), and sensitivity (.44-.92) (Millon et al., 2007; Ortiz-Tallo et al., 2011). The inventory’s dimensional and classification approximation to the DSM makes it widely used, serving as an instrument for checking the reliability and validity of others (Rossi & Derksen, 2015).
2.4. Procedures
The data collection process was performed during consultations in the PTU of HUSC, conducted once a week during the study period between December 2016 and December 2018. We proceeded to recruit the first two consecutive patients diagnosed with chronic nononcologic pain who attended consultations at the PTU. Those patients who met the inclusion criteria were interviewed by the reference practitioner on their interest in participating. Those who responded positively were transferred to the adjacent office in the same PTU. There, a general clinical research psychologist outlined the study, assessed the exclusion criteria, requested the participant’s informed consent, and administered the evaluation individually, ensuring the participant’s comfort and privacy during the evaluation. In the process of collecting sociodemographic and clinical data, we used the information in the participants’ medical history along with their oral responses (entering them into the computer at that time). The vNRS, HAM-D, and HAM-A scales were applied by the practitioner, collected in physical format, adjusted manually, and computerized. The DN4 and MCMI-III scales were self-administered, in physical format, under the supervision of the practitioner who answered any of the participant’s questions. The DN4 scale was manually adjusted and computerized; the MCMI-III was adjusted using the tool’s specific software and subsequently computerized. The duration ranged from 60 to 90 min.
Table 1 Participants’ Sociodemographic and Clinical Data
| Ne (n= 64) | Nc (n= 51) | Total (N= 115) | χ2/t/U | rφ/d/g | p-value | |
|---|---|---|---|---|---|---|
| n(%)/M±SD | ||||||
| Sex | ||||||
| Female | 43 (67.2) | 37 (72.5) | 80 (69.6) | |||
| Male | 21 (32.8) | 14 (27.5) | 35 (30.4) | χ2(.385) | −.058 | .535 |
| Age, years | 58.95±14.22 | 62.10±13.25 | 60.35±13.82 | t(−1.214) | .228 | .227 |
| Range | 21-84 | 22-87 | 21-87 | |||
| 18-34 | 3 (4.7) | 2 (3.9) | 5 (4.3) | χ2(.040) | .019 | .841 |
| 35-54 | 18 (28.1) | 13 (25.5) | 31 (27) | χ2(.100) | .029 | .752 |
| 55-64 | 18 (28.1) | 11 (21.6) | 29 (25.2) | χ2(.647) | .075 | 421 |
| 65-74 | 16 (25) | 16 (31.4) | 32 (27.8) | χ2(.574) | −.071 | .449 |
| ≥75 | 9 (14.1) | 9 (17.6) | 18 (15.7) | χ2(.276) | -.049 | .599 |
| Marital status | ||||||
| Single | 4 (6.3) | 10 (19.6) | 14 (12.2) | χ2(4.737) | −.203 | .030* |
| Married/Partnered | 46 (71.9) | 27 (52.9) | 73 (63.5) | χ2(4.389) | .195 | .036* |
| Divorced/Separated | 8 (12.5) | 4 (7.8) | 12 (10.4) | χ2(.659) | .076 | .417 |
| Widowed | 6 (9.4) | 10 (19.6) | 16 (13.9) | χ2(2.481) | −.147 | .115 |
| Occupational status | ||||||
| Employed | 16 (25.0) | 11 (21.6) | 27 (23.5) | χ2(.186) | .040 | .666 |
| Temporarily dis. | 12 (18.8) | 4 (7.8) | 16 (13.9) | χ2(2.819) | .157 | .093 |
| Permanently dis. | 4 (6.3) | 2 (3.9) | 6 (5.2) | χ2(.311) | .052 | .577 |
| Unemployed | 4 (6.3) | 3 (5.9) | 7 (6.1) | χ2(.007) | .008 | .935 |
| Home/family | 4 (6.3) | 8 (15.7) | 12 (10.4) | χ2(2.704) | −.153 | .100 |
| Retired | 24 (37.5) | 22 (43.1) | 46 (40.0) | χ2(.376) | −.057 | .540 |
| Studying | 0 (0) | 1 (2) | 1 (.9) | χ2(1.266) | −.105 | .261 |
| Education / Training | ||||||
| No formal education | 4 (3.5) | χ2(0.629) | .074 | .428 | ||
| Primary | 15 (23.4) | 13 (25.5) | 28 (24.3) | χ2(.065) | −.024 | .799 |
| Secondary | 29 (45.3) | 25 (49.0) | 54 (47.0) | χ2(.157) | −.037 | .692 |
| University | 17 (26.6) | 12 (23.5) | 29 (25.2) | χ2(.138) | .035 | .710 |
| Progression, years | 5.64±9.16 | 4.93±8.06 | 5.33±8.66 | U(1598) | .080 | .848 |
Note. Ne, chronic neuropathic pain; Nc, chronic nociceptive pain; N, universe;n, subsample; M, mean; SD, standard deviation; dis., disabled;χ2, Pearson’s chi-squared; t, Student’s t-test; U, Mann-Whitney Utest; rφ,Phi coefficient; d, Cohen’sd;g, Hedgesg; p-value, statistical significance; *p<.05; **p<.01and ***p<.001.
2.5. Data analysis
To characterize the quantitative variables, we employed the mean, standard deviation (SD), 95% confidence interval (95% CI), and range. The categorical variables are described using absolute and relative frequencies and percentages and were compared between groups using Pearson’s chi-squared test. We used Phi coefficient criteria to interpret the effect size, with the sign establishing the direction of the relationship, with r ϕ = .00 .09, r ϕ = .10 .29, r ϕ = .30 .49, and r ϕ ≥.50, indicating no, low, medium, and high effect size, respectively (Brennan & Kane, 1977). We applied the Kolmogorov Smirnov test to assess the normality of the distribution and applied Levene’s test for the homogeneity of variances. To determine differences between the quantitative variables, we applied the Mann-Whitney U test for the non-normal distribution, indicating the effect size with the Hedges’ estimator, with g < .49, g = .50 .79, and g .80, indicating a small, medium, and large effect sizes, respectively (Hedges, 1981). We employed Student’s t-test for those that met the criteria of normality, using the Cohen criteria (Cohen, 1992) to interpret the effect size, with d < .49, d = .50 .79 and d . ≥80, indicating small, medium and large effect sizes, respectively. To determine the associations between variables, we employed Spearman’s correlation coefficient, with the sign establishing the direction of the correlation, with rho = .00 29, rho = .30 -.49, rho = .50 .69, rho = .70 .89, and rho = .90 1, indicating very low, low, moderate, strong, and very strong/perfect associations (Hinkle et al., 2003). Statistical significance was set a p . ≥05. The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM Corp. Released, 2011).
Table 2 Results of the clinical variables evaluated using the vNRS, HAM-D and HAM-A scales
| Ne (n= 64) | Nc (n= 51) | Total(N= 115) | χ2/t/U | rφ/d/g | p-value | |
| n(%)/M±DT | ||||||
| VNRS (0-10) | 6.50±2.06 | 5.45±2.33 | 6.03±2.24 | U(1120) | 2.198 | .004** |
| Mild pain | 6 (9.4) | 8 (15.7) | 14 (12.2) | χ2(1.057) | −.096 | .304 |
| Moderate pain | 20 (31.3) | 27 (52.9) | 47 (40.9) | χ2(5.526) | −.219 | .019* |
| Severe pain | 38 (59.4) | 16 (31.4) | 54 (47.0) | χ2(8.935) | .279 | .003** |
| HAM-D (0-52) | 12.95±6.69 | 11.20±6.92 | 12.17±6.82 | U(1382) | .257 | .158 |
| Absence (0-7) | 12 (18.8) | 22 (43.1) | 34 (29.6) | χ2(8.106) | −.265 | .004** |
| Minor D. (8-12) | 21 (32.8) | 7 (13.7) | 28 (24.3) | χ2(4.414) | .196 | .036* |
| < Minor D. (13-17) | 12 (18.8) | 12 (23.5) | 24 (20.9) | χ2(.141) | −.035 | .707 |
| Major D. (18-29) | 18 (28.1) | 10 (19.6) | 28 (24.3) | χ2(1.118) | .099 | .290 |
| > Mayor D. (30-52) | 1 (1.6) | 0 (.0) | 1 (.9) | χ2(.804) | .084 | .370 |
| Psychopathology (18-52) | 19 (29.7) | 10 (19.6) | 29 (25.2) | χ2(1.529) | .115 | .216 |
| Melancholy I. (0-22) | 5.83±3.41 | 5.33±3.43 | 5.61±3.41 | U(1465) | .146 | .346 |
| Anxiety I. (0-12) | 3.77±2.75 | 3.45±2.57 | 3.63±2.67 | t(−..626) | .120 | .533 |
| Sleep I. (0-6) | 2.58±1.91 | 1.92±1.74 | 2.29±1.86 | t(−1.899) | .361 | .060 |
| HAM-A (0-56) | 12.34±6.41 | 10.31±6.15 | 11.44±6.35 | U(1335) | .322 | .094 |
| Absence (0-5) | 11 (17.2) | 18 (35.3) | 29 (25.2) | χ2(4.934) | −.207 | .026* |
| Mild A. (6-14) | 27 (42.2) | 17 (33.3) | 44 (38.3) | χ2(.942) | .091 | .332 |
| Mod./Severe A. (15-56) | 26 (40.6) | 16 (31.4) | 42 (36.5) | χ2(1.048) | .095 | .306 |
| Psychological I. (0-28) | 7.16±3.68 | 5.45±3.12 | 6.40±3.53 | U(1191) | 0.496 | .013** |
| Somatic I. (0-28) | 5.19±3.74 | 4.86±3.49 | 5.04±3.62 | t(−.476) | .091 | .635 |
Note. Ne, chronic neuropathic pain; Nc, chronic nociceptive pain;N, universe;n, subsample;M, mean;SD,standard deviation; vNRS, verbal numerical rating scale; HAM-D, Hamilton depression rating scale; HAM-A,Hamilton anxiety rating scale; D., depression; A., anxiety; I, index;χ2, Pearson’s chi-squared;t, Student’st-test;U, Mann-WhitneyUtest;rφ, Phi coefficient;d, Cohen’sd;g, Hedgesg;p-value, statistical significance;*p<.05; **p<.01and ***p<.001.
3. Results
The analyzed sample consisted of 115 patients, 64 (56%) and 51 (44%) of whom were classified by the DN4 as having chronic neuropathic and nociceptive pain, respectively.
3.1 Sociodemographic and clinical data of the pain
The demographic data met the normality of distribution criteria, showing a predominance of the female sex in both groups, with a mean age of 58.95 (SD, 14.22) years in the neuropathic group and 62.10 (SD, 13.25) years in the nociceptive group. The percentage of un married/unpartnered participants in the nociceptive group was statistically larger [19.6%;χ2(1,N= 115) = 4.73,p=.030], with a low negative association (rφ=−.203),while the percentage of married/partnered participants was statistically larger in the neuropathic group [71.9%;χ2(1,N= 115) = 4.38,p=.036], with a low positive association (rφ=.195). The pain progression, in years, was longer in the neuropathic group (mean, 5.64;SD, 9.16)than in the nociceptive group (mean, 4.93;SD, 8.06), al-though it was not statistically significant (ns) (Table 1).
3.2. Perceived pain intensity (vNRS)
The neuropathic group showed a pain intensity (median 7; range 0-9) significantly greater than that of the nociceptive group (median 5; range 1-10;U= 1120; p=.004), with ago f 2.19, indicating a large effect size. There were statistically significant differences in the largest percentages of individuals of the neuropathic group who perceived severe pain [59%;χ2(1,N= 115) =8.93,p=.003], with a low positive association (rφ=.279), as well as in the percentages of participants of the nociceptive group (53%) who perceived moderate pain[χ2(1,N= 115) = 5.52,p=.019], with a low negative association (rφ=−.219) (Table 2).
3.3. Depressive(HAM-D)andanxiety(HAM-A)symptoms
The evaluated depressive symptoms showed no significant differences between the groups’ mean scores or in the internal indices. The percentage of the nociceptive group (43%) in the without depression category was statistically larger than that of the neuropathic group(18%;χ2(1,N= 115) = 8.10,p=.004), with a low negative association (rφ=−.265). The percentage of the nociceptive group (33%) in the without depression cate-gory was statistically larger than that of the neuropathic group (14%;χ2(1,N= 115) = 8.10,p=.004), with a low negative association (rφ=−.265). The analyzed anxiety symptoms revealed significant differences in the per-centage of the nociceptive group (35%) in the without anxiety category compared with the neuropathic group [17%;χ2(1,N= 115) = 4.93,p=.026], with a low negative association (rφ=−.207). The score on the internal indices of mental anxiety was also significant when comparing the neuropathic group (median 7.5; range 0-15) with the nociceptive group (median 6; range 0-13;U= 1191;p=.013), with agof .49, indicating a small effect size (Table 2).
3.4. Relationship between the progression and perceivedintensity of pain (vNRS) with the depressive (HAM-D) and anxiety (HAM-A) symptoms
We obtained statistically significant positive low correlations for the neuropathic group’s vNRS and the HAM-Dscore (rho(62)=.392;p=.001) and with its internal in-dices of melancholy (rho(62)=.417;p=.001). With the internal indices of HAM-A mental anxiety (rho(62)=.254;p=.043), the correlation was positive and very low. For the nociceptive group, the vNRS showed a significant, positive and very low correlation with the internal indices of HAM-D sleep disorder (rho(49)=.288;p=.040).
3.5. Clinical syndromes (MCMI-III)
The scores averaged below 60, which corresponds tothose expected for the general population (0-34) and low(35-59, higher than the general population but not suggesting a disorder), with the highest scores for anxiety clinical syndrome (not significant). There were greater significant differences for the neuropathic group (median60; range 0-93) compared with the nociceptive group(median 9; range 0-92) in the delusional disorder scores(U= 1248;p=.028), with agof .037, indicating a small effect size. The neuropathic group showed significantly larger percentages in the 75-84 score range for the presence of the dysthymic clinical syndrome [26% vs. 9%for the neuropathic and nociceptive groups, respectively;χ2(1,N= 115) = 5.15,p=.023], with a low positive as-sociation (rφ=.212), and in the 60-74 score range suggestive of thoughts disorder [29% vs. 9%, respectively;χ2(1,N= 115) = 6.79,p=.009], with a low positive as-sociation (rφ=.243) (Figure 2).
3.6. Clinical personality patterns (MCMI-III)
Suggestive scores (60-74) were achieved in the narcissistic personality pattern for the nociceptive group [statis-tically larger (72% vs. 53% for the nociceptive and neuropathic groups, respectively);χ2(1,N= 115) = 4.53,p=.033], with a low negative association (rφ=−.199),and in the compulsive personality pattern of both groups(not significant). The neuropathic group had significantly higher percentages in the scores suggestive of the dependent [34% vs. 15% for the neuropathic and nociceptive groups, respectively;χ2(1,N= 115) = 5.14,p=.023;rφ=.211] and paranoid [54% vs. 33%;χ2(1,N=115) = 5.22,p=.022;rφ=.213] personality patterns, with positive and low associations (Figure3).Ninety-nine percent of the sample achieved scores suggestive (60-74) of one or more personality patterns (98%and100%fortheneuropathicandnociceptivegroups,respectively). Sixty-five percent of the sample achieved scores in the psychopathology presence range (75-84)for at least one pattern (62% and 68% for the neuropathic and nociceptive groups, respectively), and 26%achieved scores in the psychopathology prominence category (85-115) of a personality pattern (89% and 94%,respectively) (not significant).
3.7. Relationship between the syndromes and clinicalpersonality patterns (MCMI-III) and the perceivedpain intensity (vNRS), progression and depressive(HAM-D) and anxiety (HAM-A) symptoms.
The clinical syndrome scales (Table 3) revealed significant, positive, and strong correlations for the neuropathic group, which related the somatoform clinical syn-drome with the HAM-D score (rho(62)=.751;p=.000)and the major depressive clinical syndrome with the HAM-A score (rho(62)=.716;p=.000) and with its internal indices of mental anxiety (rho(62)=.714;p=.000). The neuropathic group showed 28 moderate positive correlations for HAM-D and HAM-A with clinical syndromes (anxiety, somatoform, dysthymic, PTS, thoughts, and major depressive). The nociceptive groups howed 15 moderate positive correlations for HAM-Dand HAM-A with clinical syndromes (anxiety, dysthymic, thoughts, and major depressive). The personality pat-tern scales (Table 4) showed 10 moderate positive correlations for the neuropathic group, relating the depressive personality pattern with HAM-D scores, internal indices of melancholy and with the measures of HAM-A; relating the borderline personality pattern with the scores for HAM-D, HAM-A and internal indices of mental anxiety; and relating the evitative personality pattern with the HAM-A scores and the paranoid personality pattern with the internal indices of mental anxiety.
4. Discussion
The present study on psychopathological and personality profiles and their relationship to pain progression and intensity in PTU patients with chronic non oncologic pain (nociceptive and with a neuropathic component) obtained sociodemographic results comparable to those of other studies that share sample characteristics(Failde etal.,2018; Pérez et al.,2017; Soriano & Monsalve,2018).
The pain intensity was significantly greater in the neuropathic group, with 60% presenting severe pain, which agrees with other studies in which neuropath y recorded greater daily pain(Dueñas et al.,2015; Faildeet al.,2018; Pérez et al.,2017), as the result of chronicity, low treatment response and difficult management, which adds the neuropathic component(Finnerup et al.,2016;Scholz et al.,2019). Pain intensity was not related to the progression of chronic pain but was related to depressive symptoms, melancholy, mental anxiety (in the neuropathic group), and sleep disorders (in the nociceptive group), exemplifying the reported bidirectional relation-ship(Arango-Dávila & Rincón-Hoyos,2018; Baastrupet al.,2016; Velly & Mohit,2018).
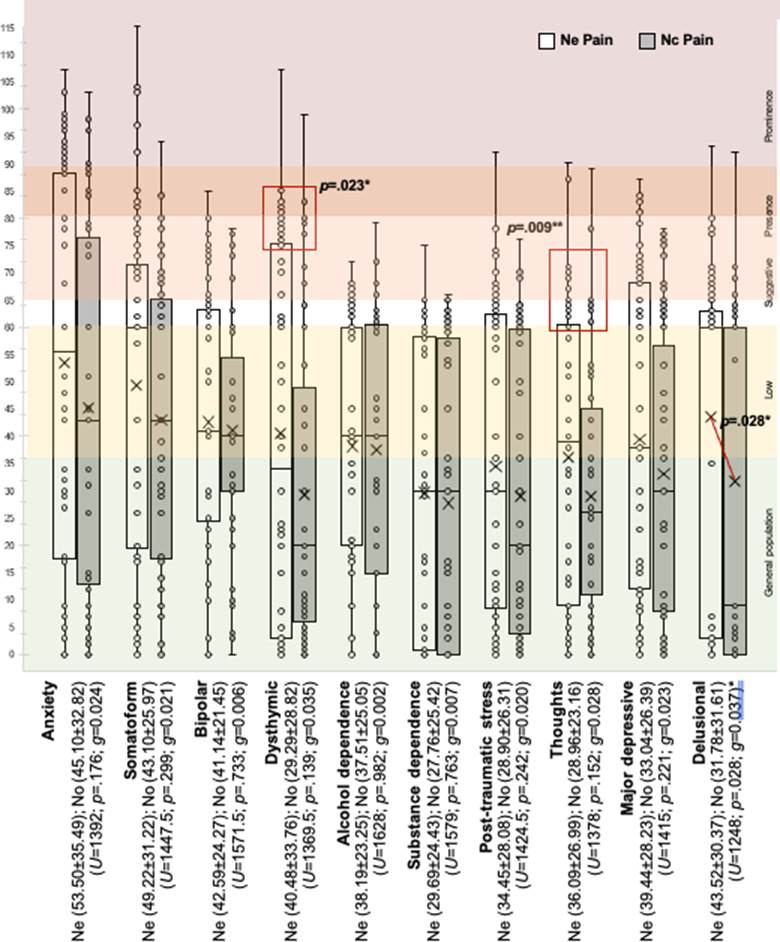
Figure 2 MCMI-III Clinical Syndrome Scores by pain group. Note. MCMI-III, Millon Clinical Multiaxial Inventory III; Ne, chronic neuropathic pain; Nc, chronic nociceptivepain; (Mean ± Standard Deviation);U, Mann-Whitney Utest; g, Hedges’g; p-value, statistical significance;*p<.05; **p<.01.
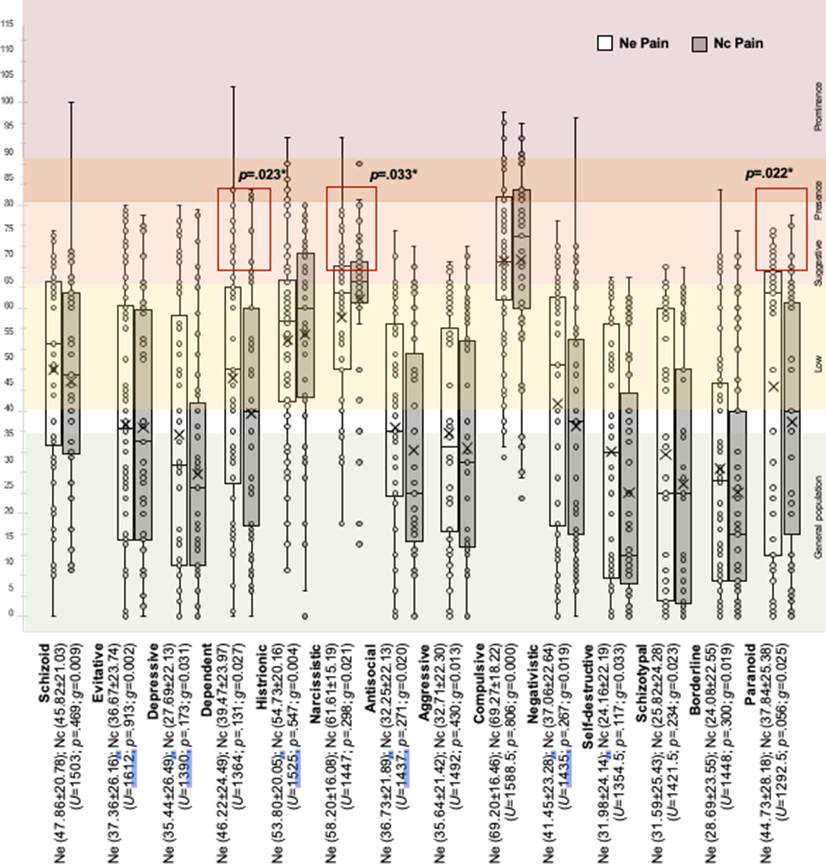
Figure 3 MCMI-III Clinical Personality Pattern Scores by pain group. Note. MCMI-III, Millon Clinical Multiaxial Inventory III; Ne, chronic neuropathic pain; Nc, chronic nociceptivepain; (Mean±Standard Deviation);U, Mann-WhitneyUtest;g, Hedges’g;p-value, statistical significance;*p<.05.
Table 3 Relationship between the results of the MCMI-III clinical syndromes and progression, vNRS, HAD-D and HAD-A, by pain group
| Progression | vNRS | HAM-D | HAM-A | ||||||||||||||||
| Score | Melancholy | Anxiety I. | Sleep I. | Score | Mental I. | Somatic I. | |||||||||||||
| rho | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | |
| Anxious | ↑ | ↑ | ↑.28 | .30 | ↑↑↑.69* | .59* | .61* | .49 | .50 | 43 | −.38 | .37− | ↑.57* | 55*↑↑ | −.61* | .55*− | .49 | .44 | |
| Somatoform | .28 | ↑ | .39 | ↑↑.75 | .48 | 65* | 47 | .53* | 34 | .46 | .30 | ↑↑.65 | .44 | .69* | .44 | 52* | 39 | ||
| Bipolar | ↑↑ | .39 | .34 | .33 | .28 | .39 | .26 | .31 | .26 | .44 | |||||||||
| Dysthymic (Ne↑) | .25 | .42 | ↑↑↑.59* | .57*↑↑ | .55* | .56* | .45 | .47 | .29 | .31 | ↑↑.61* | .45↑↑↑ | .61 | .50* | 53* | 39 | |||
| Alcohol D. | ↑ | .42↑ | .30 | .44 | .29 | .28 | .34 | .28 | .38 | ||||||||||
| Substances D. | .33 | .37 | .33 | .28 | .28 | ||||||||||||||
| PTS | ↑ | ↑.63* | 45↑ | .59* | .36 | .48 | .34 | .26 | .29 | .63* | .41 | .59* | .44 | 57* | .33 | ||||
| Thoughts | .58* | .53* | .61* | .49 | .46 | .53* | |||||||||||||
| Depressive M. | .26 | ↑ | ↑.68* | 63*↑ | .60* | 60* | .54* | 49 | .42 | .42 | ↑↑.71 | 57*↑↑↑ | .71 | .56* | 60* | .53* | |||
| Delusional (NeM∗) | ↑ | ↑↑ | ↑ | .26 | .29 | .34 |
Legend.Spearman’s correlation coefficient (rho) was employed for the quantitative scores (Ne=rho(62) and Nc=rho(49)). All data shown revealed statistically significant correlations (p<.05). The interpretation of the correlations has been indicated as follows: very low rho=.00-.29 (italics), lowrho=.30-.49 (normal), moderaterho=.50-.69 (*), strongrho=.70-.89 (bold), very strong rho=.90-1 (underlined). Pearson’s chi-squared was employedfor the scores (±75-115) of each of the clinical syndromes clinicians with the qualitative variables of progression, vNRS , HAM-D and HAM-A; its interpretation is as follows:↑=p<.05;↑↑=p<.01;↑↑↑=p<.001. (Ne↑) = Significant differences in the percentage of individuals with Ne (±75-115)in dysthymia. (Ne M*) = Difference statistically greater than the mean of the Ne group in the delusional score.Note.Ne, chronic neuropathic pain; Nc, chronic nociceptive pain; vNRS, verbal numerical rating scale; HAM-D, Hamilton depression rating scale; HAM-A, Hamilton anxiety rating scale; I, index; D, dependency; PTS, post-traumatic stress; M, major.
Table 4 Association between the results of the MCMI-III clinical personality patterns and progression, vNRS, HAD-D and HAD-A, by pain group
| Progression | vNRS | HAM-D | HAM-A | ||||||||||||||||
| Score | Melancholy I | Anxiety I. | Sleep I. | Score | Mental I. | Somatic I. | |||||||||||||
| rho | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | Ne | Nc | |
| Schizoid | ↑↑ | ↑ | ↑ | .34 | .27 | .28 | .30 | ||||||||||||
| Evitative | .39 | .34 | .41 | .30 | .51* | .46 | .48 | ||||||||||||
| Depressive | .32 | .62* | .47 | .58* | .38 | .48 | .38 | .31 | .35 | .64* | .41 | 58* | .39 | .58* | .35 | ||||
| Dependent | .25 | ↑.47 | ↑ | .42 | .41 | .32 | .37 | .26 | |||||||||||
| Histrionic | −.32 | −.45 | −.43 | −.29 | −.46 | ||||||||||||||
| Narcissistic | −.43 | −.36 | −.27 | −.49 | −.38 | −.29 | ↑−.47 | −.32 | −.39 | −.49 | −.38 | ||||||||
| Antisocial | .29 | .31 | .31 | ||||||||||||||||
| Aggressive | .33 | .34 | .34 | .35 | .37 | ||||||||||||||
| Compulsive | ↑ | −.30 | |||||||||||||||||
| Negativistic | ↑ | ↑ | .31 | .42 | .48 | .44 | .46 | .44 | .41 | .34 | |||||||||
| Self-destructive | .39 | .34 | .40 | .37 | .38 | .39 | .32 | .34 | .28 | .39 | .33 | ||||||||
| Schizotypal | .30 | .35 | .31 | .33 | .30 | .33 | .46 | .34 | .49 | .33 | .32 | .29 | |||||||
| Borderline | ↑↑ | ↑.51* | 46 | .42 | .34 | .49 | .46 | .27 | .56 | .45 | 53* | .43 | .49 | .42 | |||||
| ParanoidG | .36 | ↑↑↑ | .48 | .44 | .39 | .47 | .52* | .34 |
Legend. Spearman’s correlation coefficient (rho) was employed for the quantitative scores (Ne=rho(62) and Nc=rho(49)). All data shown revealedstatistically significant correlations (p<.05). The interpretation of the correlations has been indicated as follows: very lowrho=.00-.29 (italics), low rho=.30-.49 (normal), moderate rho=.50-.69 (*), strong rho=.70-.89 (bold), very strongrho=.90-1 (underlined). Pearson’s chi-squared was employed for the scores (±75-115) of each of the clinical syndromes clinicians with the qualitative variables of progression, vNRS, HAM-D and HAM-A; its interpretation is as follows:↑=p<.05;↑↑=p<.01;↑↑↑=p<.001.Note. Ne, chronic neuropathic pain; Nc, chronic nociceptive pain; vNRS, verbal numerical rating scale; HAM-D, Hamilton depression rating scale; HAM-A, Hamilton anxiety rating scale; I, index.int.j.psychol.res|doi: 10.21500/20112084.563161
In terms of affectivity, almost two-thirds of the nociceptive group presented scores indicating depressive psychopathology, compared with 81% of the neuropathic group. Minor depression was the most common condition, and consistent with previous studies, a third of the patients had major depression (Arango-Dávila & Rincón-Hoyos, 2018; Velly & Mohit, 2018). In terms of anxiety, our results also coincide with those of previous studies (Turk et al., 2016), given that 64% of the nociceptive group and 82% of the neuropathic group presented mild to moderate anxiety, with the neuropathic group reaching the highest levels, increasing their perception of the pain as the depressive symptom score increased (especially if they progressed with melancholy) and when they experienced mental anxiety. For the nociceptive group, the pain intensity did not increase by psychopathological variables but rather by sleep impairment.
The results of the study sample, extracted from a PTU, agree with and corroborate those of previous studies (Arango-Dávila & Rincón-Hoyos, 2018; Colloca et al., 2017; Dueñas et al., 2015; Failde et al., 2018; Finnerup et al., 2016; Lanzara et al., 2020; Pérez et al., 2017), thereby confirming the comorbidity reported between chronic pain and anxiety and depressive psychopathology. We also confirmed the added risk of presenting depressive and anxiety disorders that represent the neuropathic component in pain chronicity (Colloca et al., 2017; Finnerup et al., 2016; Pérez et al., 2017; Scholz et al., 2019). Similarly, the levels of both psychopathological conditions were directly related to the severe pain type, which is consistent with previous studies that suggest a bidirectional relationship (Arango-Dávila & Rincón-Hoyos, 2018; Dippolito et al., 2020; Edwards et al., 2016; Tabor et al., 2017) between increased pain intensity, which worsens the depressive and anxiety symptoms and, in turn, between the severe anxiety states and depressive symptoms that favor and aggravate the presence of pain. These results help identify the challenges of the therapeutic strategies, given that they need to combine relief for the pain intensity (which entails depressive symptoms) with the increase in muscle tension and self-perception of the pain intensity in the affected area (which entails anxiety) (Edwards et al., 2016; Velly & Mohit, 2018).
Along the same line of psychopathological analysis, the scores on the MCMI-III clinical syndrome scales showed a higher frequency of hostile attitudes, persistent tension, suspicion, and watchfulness when faced with possible betrayal in the neuropathic group, typical attitudes in delusional disorder described by Millon, categorized as severe and referenced in studies of disruptive chronic pain (Ajo et al., 2020; Yang et al., 2019). The results also showed a dysthymic mood, characterized by feelings of despondency and guilt, lack of initiative, apathy, and low self-esteem, revealing pessimistic feelings towards the future, social isolation, fatigue, anhedonia, and reduced efficacy in completing ordinary tasks (Millon et al., 2009), which have been described as a predictor of chronicity and changes in treatment (Ajo et al., 2020; Shahar et al., 2018). There is also a tendency to present confusing thoughts, inappropriate emotions, and feelings of being misunderstood or isolated (symptoms recorded in thought disorder) reported in disruptive chronic pain (Ajo et al., 2020). Lastly, the same neuropathic group also showed greater somatoform symptoms the longer their time with chronic pain, characterized by difficulty expressing emotions, preoccupation with health, and manifesting numerous complaints that this condition entails. This can be explained by the multitude of physiological and vegetative symptoms, the imprecision and changes in the pain and the consequent difficulty in specifying and describing them, along with the complexity at the sensory level, which imparts the neuropathic nature (Colloca et al., 2017; Failde et al., 2018), coinciding with previous studies (Lanzara et al., 2020; Park et al., 2020; Tutoglu et al., 2015). All of the impairment of the neuropathic group coincides with the results from assessing the depressive symptoms and once again emphasizes the greater psychopathological impairment of the group with pain that progresses with neuropathy versus nociception (Baastrup et al., 2016; Colloca et al., 2017; Dueñas et al., 2015; Finnerup et al., 2016; Pérez et al., 2017; Scholz et al., 2019).
In terms of pain progression and intensity, the nociceptive group was affected when the progression exceeded three years, showing anxiety symptoms, somatoform disorders, emotional lability, and delusional disorders. The intensity of their pain is related to the anxiety and dysthymic states; when faced with severe pain, they can present thought disorder symptoms and those of major depression. The neuropathic group is affected per se, given that any time their progression is related to somatoform and anxiety symptoms. Their pain intensity (whether mild, moderate or severe) is related to anxiety, somatoform, dysthymic, major depressive, and even post-traumatic stress clinical syndromes, experiencing the pain as life-threatening, producing intense fear, and defenselessness (Millon et al., 2009), which coincides with the probability of presenting the syndromes three times more often than the general population when in the presence of chronic pain (Turk et al., 2016).
In terms of the study of the MCMI-III clinical personality patterns, the nociceptive group revealed a marked tendency towards egoistic and arrogant attitudes, feeling pleasure by focusing on themselves (similar to the narcissistic personality disorder of DSM-5; American Psychiatric Association, 2014; Millon et al., 2009). The tendency to empower this condition could be explained by the need for distraction from pain, using self-absorption and subsequent interaction/expression as a tool for managing pain (Ajo et al., 2020; Campbell et al., 2015; Soriano & Monsalve, 2018). The neuropathic group tended to adopt a passive/submissive role, searching for external guidance, with the goal of receiving affection/protection, which is consistent with the reported low self-directedness (Naylor et al., 2017). The group also frequently showed distrust, anticipated defensiveness, rigidity, and resistance to control (despite being therapeutic for controlling the pain) (Park et al., 2020; Yang et al., 2019), traits similar to the dependent and paranoid personality disorder of DSM-5 (American Psychiatric Association, 2014; Millon et al., 2009).
When the nociceptive group was faced with a long progression of the pain, they presented paranoid, negativistic and compulsive attitudes. As pain intensity increased so too did the irritable, negativistic, and antisocial attitudes (denial of chronic pain; Campbell et al., 2015), as well as the depressive and compulsive attitudes, which are inverse to the pain intensity and can exemplify how control and rigidity of obsession and compulsion serve as a tool to distract from and minimize the pain (González et al., 2007; Ibrahim et al., 2020; Millon et al., 2009; Soriano & Monsalve, 2018). In the neuropathic group, there was no relationship with the intensity of the pain, but there was with the progression, showing dependent and paranoid tendencies (boosting both conditions with the passage of time), as well as schizoid, negativistic, and limiting behaviors, going from patterns with dysregulated affectivity (Cluster B) to inhibited and isolated patterns (Cluster A and C), which support the tendency to lability when faced with chronic pain (Campbell et al., 2015; Cavicchioli et al., 2021; Shapiro et al., 2020). This group also shows a reverse association (as a possible tool for coping with chronic pain) regarding histrionic and narcissistic patterns with depressive and anxiety symptoms (Ajo et al., 2020; Campbell et al., 2015; Soriano & Monsalve, 2018).
Most of the study participants tended to show a controlling, demanding, and perfectionist behavior, possibly resulting from a conflict between hostility (due to being forced to accept the imposition of chronic pain) and the fear of social disapproval (due to stigmatizing beliefs), increasing the demands and rigidity, with the idea of compensating for and minimizing the discomfort (Millon et al., 2009). This is similar to obsessivecompulsive personality disorder and coincides with previous results describing difficulties in acquiring coping strategies for pain (Ibrahim et al., 2020), manifesting with harm avoidance and low self-directedness (Gustin et al., 2015; Ibrahim et al., 2020; Kato et al., 2017; Naylor et al., 2017). Moreover, both groups tend to show narcissistic, histrionic, and schizoid attitudes. Therefore, the high prevalence of maladaptive scores could suggest that the stable predispositions that constitute personality have been affected by the chronic pain (Chang et al., 2017; González et al., 2007; Gustin et al., 2015; Ibrahim et al., 2020). Although both groups show multiple relationships, the scores indicative of depressive and anxiety psychopathology suggest greater involvement for the clinical syndromes and personality patterns of the neuropathic group, showing that when faced with neuropathy and comorbidity, the clinical condition is aggravated and the prognosis worsened (Aho et al., 2022; Chang et al., 2017; Colloca et al., 2017; Galli et al., 2021; Park et al., 2020; Yang et al., 2019).
Nevertheless, the results of this study should be interpreted considering the study’s limitations. It is important to note that only those participants who completed the assessment constituted the final sample and that the assessment did not record their psychiatric history or drug treatments. Given that this was a descriptive study aimed at studying numerous clinical aspects beyond the main objective, an adjustment by multiple comparisons was not performed. The results are not generalizable because the sample came from a specialized unit and do not allow causal attributions due to the study’s cross-sectional nature, which could change to longitudinal in future studies with the aim of assessing the psychopathology and personality patterns, as the pain progresses or intensifies, and determining whether these values change with specific mental health treatment. However, we observed the relationship between the progression times of chronic pain and the intensity and type of pain, with distinct psychological indicators such as depressive and anxiety symptoms, clinical syndromes, and personality patterns. These findings provide the opportunity for identifying detailed psychopathological aspects linked to the temporality or intensity of pain, which can be considered by practitioners when treating patients and preparing specific interventions. Various intervention approaches can be created: an approach to chronic nociceptive pain focusing, initially, on pain intensity in the early phases of the diagnosis and, subsequently, a psychological assessment on its progression. Another perspective is for chronic pain with a neuropathic component, which from its start can be addressed with specific psychological care for the disease, increasing the psychological intervention with the passage of time. Moreover, it is apparent that future studies need to assess the role of psychological interventions adapted to the most common personality patterns, according to the pain type, intensity, and progression and when to apply the intervention in the various moments of the painful experience, with the aim of specifying the most appropriate and efficient point at which to apply the psychological intervention in chronic pain.
5. Conclusions
The group with the neuropathic component had greater psychopathological severity scores in all the administered scales and was related to more clinical syndromes and personality patterns, thereby showing the presence of substantial differences between the two types of pain when treating the psychopathology and reinforcing the severity entailed by neuropathy.
The nociceptive group showed scores indicative of psychopathology only starting at three years of developing chronic pain and/or when the pain was severe. The group with a neuropathic component showed scores in delusional thoughts with a tendency to dysthymic moods and to thought disorders that did not necessarily relate to other variables. This also reflects psychopathology against the passage of time with chronic pain and to the intensity of pain; unlike the other group, however, it happens at any time during the progression or at any pain intensity. In terms of personality patterns, both groups revealed compulsive tendencies (followed by narcissistic, histrionic, and schizoid); nevertheless, pain intensity was only related to the nociceptive group, while progression only interacted with the group that progressed with neuropathy.
In conclusion, for a comprehensive approach when treating chronic pain, the presence ofvarious psychopathological indicators requires an individualized strategy.