Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
CES Psicología
On-line version ISSN 2011-3080
CES Psicol vol.8 no.1 Medellín Jan./June 2015
Normality and Mental Health: analysis of a multivalent relationship
Normalidad y Salud Mental: análisis de una relación multivalente
Juan Carlos Jaramillo Estrada1, Diego Alveiro Restrepo-Ochoa2
1 Magíster en Psicología. Psicólogo. Docente Investigador Universidad CES. Medellín, Colombia jjaramilloe@ces.edu.co
2 Ph.D. en Salud Pública. Psicólogo, Docente Investigador Universidad CES. Medellín, Colombia drestrepo@ces.edu.co
Citation: Jaramillo, J.C. & Restrepo-Ochoa, D.A. (2015). Normality and Mental Health: analysis of a multivalent relationship. Journal of Psychology CES, 8(1), 37-46.
Abstract
The categories "Normality" and "Mental health" are closely related. What is considered "mentally healthy" is linked with what is estimated as "normal" in every historical and cultural context. There are at least four ways to comprehend "normality" which determinate the forms of conceptualization and intervention in mental health: adjustment/ maladjustment understood as the subject’s adaptation to the social expectation; health/illness determined by biological factors under the medical model; statistics normality/ statistics abnormality defined from statistics criteria of population distribution and wellbeing/ discomfort related with the assessment that subjects make about their own life experiences. This paper shows discussion about the relationship between the categories "normality2 and "mental health" from the perspective of these four antithetical pairs and the analysis of the theoretical and practical implications of each one of these perspectives.
Keywords: Mental Health, Normality, Adaptation, Adjustment, Wellbeing.
Resumen
Las categorías de "Normalidad" y "Salud Mental" se encuentran estrechamente relacionadas; aquello que se considera "mentalmente sano", está ligado a una idea de lo que se estima como "normal" en cada contexto histórico y cultural. Existen al menos cuatro formas de entender la "normalidad", que determinan las formas de conceptualización e intervención en salud mental: adaptación/inadaptación, entendida como el ajuste del sujeto a las expectativas sociales; salud/enfermedad, determinada por factores biológicos, bajo la lógica del modelo médico; normalidad estadística/anormalidad estadística, definida a partir de criterios estadísticos de distribución poblacional, y bienestar/malestar, relacionada con la valoración que los propios sujetos hacen sobre sus experiencias vitales. En el presente artículo se discute la relación entre las categorías de normalidad y salud mental a partir de estos cuatro pares antitéticos, señalando algunas implicaciones teóricas y prácticas derivadas de cada uno de ellos.
Palabras clave: Salud Mental, Normalidad, Adaptación, Bienestar.
Introduction
The World Health Organization (WHO) has recognized mental health as an essential aspect of welfare and development of individuals, societies and countries (World Health Organization, 2008). From the slogan "There is no health without mental health" (WHO European Ministerial Conference on Mental Health, 2005), WHO has stressed out the need to integrate mental health in all aspects of health and social policy (Prince et al, 2007; WHO, 2008). So much for the magnitude of the problems related to mental illness, such as the costs involved and above all, for their impact at individual, familiar, communitarian and social levels, in terms of a suffering that goes beyond the figures and disability generated (Ministry of Social Welfare & Social Foundation FES 2005).
WHO defines mental health as "a state of welfare in which the individual realizes his own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his community "(WHO, 2007).
Meanwhile, the Canadian Ministry of Health and Welfare has defined it as:
The ability of individuals and groups to interact with each other and with the environment; a way to promote subjective well-being, development and optimal use of psychological potentialities, whether cognitive, emotional or relational. Also, the achievement of individual and collective goals, according with justice and common welfare (Republic of Colombia. Ministry of Health, July 13, 1998).
More recently, the Colombian National Law of Mental Health (Law 1616, 2013), presents the following approach in relation to the definition of mental health:
Mental health is defined as a dynamic state that is expressed in daily life through the behavior and interaction in such a way that allows individuals and collective subjects to display their emotional, cognitive and mental resources to transit through everyday life, to work, to establish meaningful relationships and to contribute to the community. Mental health is of national interest and priority for the Republic of Colombia, it is a fundamental right, it is a priority public health issue and an essential component of the general welfare and improvement of the quality of life of Colombians (Congress of Colombia, January 21, 2013, p.1).
All these definitions of mental health, involve at least, three fundamental problems: the conceptual eclecticism, operational difficulties and the gap between concepts and practice.
The eclectic conceptual refers to the mixture of theoretical reference points at the moment of providing content to the central categories of each definition (i.e. welfare, abilities, performances and so on.) Since many of these categories have a counterpart in the world of common sense, the presentation of these definitions seem fairly clear and understandable; notwithstanding, to make a critical analysis of them, they will highlight significant inconsistencies, inaccuracies and gaps.
From this eclecticism, a second problem arises: the operational difficulty. Different from the mental disorders, that following the precepts of the biomedical model, may be objectified and intervened within a certain margin of certainty, prediction and control (using for them diagnostic manuals such as DSM and ICD), the definitions of mental health developed from categories like "welfare" and "abilities" are vague and bring with them significant challenges to move from the conceptual and ideological level to the practical field of assessment and intervention.
Finally, and as a result of the above, there is a gap between the notion of mental health - defined in "positive" terms - and the practices in the field of mental health, that usually concentrate on the area of risk and mental health. So, mental health has become in a socially acceptable "label" to refer to research, policies, interventions and services that address mental illness.
One of the roots of this problematic situation is the notion of normality understood as a criterion of demarcation between what is considered "healthy" or "sick", "adapted" or "maladjusted", "welfare" or "discomfort".
The notion of normality is multivalent and relative, product of the socio-historical context in which it is conceptualized, and is anchored in the interests of different groups of power (scientific, political, and economic) (Canguilhem, 1981, 2004). Consequently, the way "normality" is understood is a conceptual problem with serious ethical and political connotations that define -at great scale- the economic, social, educational and professional aspects of those who work in the mental health field, their roles, resources and social recognition (Ardila, 2008; Eisenberg, 1977; Vergara Quintero, 2007).
The purpose of this article is to discuss the relationship between categories of normality and mental health from four antithetical pairs: adapted/ maladjusted, health/ disease, statistical normality/ statistical abnormality and wellness/ discomfort, pointing out some theoretical and practical implications arising from each one of them.
Mental Health in History
The ways in which "mental health" and "mental illness" have been understood has been closely tied to contextual conditions of each historical moment, so these conditions (social, economic, cultural, political, religious, etc.), have defined what is considered mentally sane or ill (Berlinguer, 1994; Holtz, Holmes, Stonington, & Eisenberg, 2006; Ricón, 1991). According to Guinsberg (2001), all cultures have an ideology of the deviation from which the repressive management is justified according to some religious, social codes etc.
For example, in the stories and histories of many Aboriginal communities are found a number of assumptions. They were understood and classified today as sick, from religious magical logic, for which the bizarre behavior was interpreted as an effect of possession - be it divine or devilish- or, in many cases, as the dialogue of higher entities who expressed through a chosen one (Ardila, 1967).
Further on In the Middle Ages, the concept of normality and with it, what we now understand as mental health, was permeated by a strong Christian religious conception in which sin emerged as the backbone of any reflection about daily living (Rezk & Ardila, 1979; Shorter, 1997). Thus, any behavior that transgressed the standards defined by the Church and then by the Holy Inquisition, was understood from the logic of sin and grace and, therefore, its treatment should be addressed by various purification strategies such as torture or fire (Franz, 1970; Shorter, 1997).
Finally, in cultures secularized -predominantly scientific-, the social order is justified by the objectivity of the natural laws and in this case the deviation is associated with the disease (Guinsberg, 2001).
In the context of the nineteenth-century, at the time of the second industrial revolution, normality began to be linked with specific aspects of scientific logic. They were articulated with objective perspectives that sought to find the cause of its alteration a wide range of neuro-biochemical elements, correctable through medical/psychiatric techniques, among which could be included pharmacotherapy, electroconvulsive therapy (Guinsberg, 2007) and even psychosurgery or surgery for mental disorders (Pedrosa-Sanchez & Sola, 2003).
In the first decade of the twentieth century a different look came forcefully, alternative to the one indicated above, which sought to find in the psychic structure of people the reasons for the change in normality (Ardila, 2008; Franz, 1970; Rezk & Ardila 1979; Shorter, 1997). Back in the fifties, the perspective of normality found in neurotransmitters a promising alternative to explain the determinants of behavior, and with it, pharmacology as a strategy to correct its imbalances. The biological, now understood from this perspective became the model of normality that prevails in the conceptualization of what is meant by Mental Health (Carrillo Ibarra, 2008; Villa Rodriguez, 2008).
Analysis of Normality Concept
In this brief tracking, different historical conceptions of normality can be observed; whether they were linked to animistic, religious, biological -anatomic functional-, psychic or biological, -neuro-biochemical- aspects. Each one of them has determined what is defined as healthy or ill and, in themselves, the different social, cultural, political, economic, conceptual and applied alternatives that have intervened those who have entered the field of abnormality. (Gómez, 2002; Gonzalez, 2007).
The following four perspectives from which you can understand the relationship between "normality" and "mental health" are proposed. They are presented as antithetical pairs, each of which is supported in different anthropological foundations and with conceptual implications and differentiated practices (Gómez, 2011; Gómez & González, 2004).
1. Adjustment-maladjustment:
The concept of adjustment is closely linked to reproduction, whether biological reproduction (in the case of life sciences) or social reproduction (in the case of social and human sciences). In other words, it is considered socially "adjusted" that who can play the social order. These adjustment criteria are of ideological, philosophical or religious nature, although often presented as scientific facts, and give rise to an ideal definition of mental health (Guinsberg, 2001).
According to the adjustment criterion of mental health, people who deviate totally or partly from the established social norms, are not seen only as maladjusted, but as mentally ill (Guinsberg, 2001). Adjustment is a non-disruptive operation, accepted by the community in which the life of the person passes. In this sense, it is considered normal that who adjusts to the dominant rules, does not show serious problems and does not give serious problems to others (Jervis, 1977).
Therefore, that who works more or less well in the social sphere, that is, who works, produces, purchases his home, invests its resources in a profitable way, has a family with whom to spend the remainder of time after work, keeps good relations with neighbors and has no behaviors that create problems for the community where he lives, may be seen as appropriate and, in some way, be seen as a being with mental health.
On the contrary, those who do not comply with the social standards set by the community, generating disruptive behavior in context and that do not conform to that expected by most, could become qualified as a person lacking mental health and therefore, would be a good candidate to be subject to professional intervention (Fierro, 2000, 2004; Fierro & Cardinal, 1993, 2001; Garcia Martin, 2002; Mebarak, De Castro, Salamanca, & Quintero, 2009; Rodriguez Rossi, 2005).
2. Health-disease:
Linked to a biomedical perspective, this way of thinking about normality/abnormality is supported in the assumption of universal and objective existence of the disease, defined as a diagnosable entity that can be delimited and thus intervened using standardized ideal methods through scientifically proven validation exercises. Thus, nosotaxies are created which describe in detail the diagnostic criteria by which one can determine the existence of some kind of disease and consequently with it, the most appropriate treatment options to alleviate the disease. As is the medical logic behind this concept, it is understood that the causes of the disease mainly fall into some kind of biological or Neuro-biochemistry alteration, so it is expected that interventions can be made through standardized guidelines and protocols, objectively defined and with the fundamental support of psychopharmacology as basic treatment.
3. Statistical normality-statistical abnormality:
Linked to a statistical perspective, this antithetical pair focuses its reflection on mathematical criteria, statistically verifiable objectives that explain the presence/absence of mental health through the placement of individuals with regards to means and standard deviations to determine if their behavior is within expected ranges (social perspective) or scientifically defined (health perspective) or, on the contrary, is outside them. Statistical notion suggests that the behaviors that frequently occur in a population are normal, while infrequent behaviors are abnormal (Rogers & Pilgrim, 2010).
As Guinsberg states, the statistical criterion arises under the influence of social anthropology and breaks with the idea of a "model" of mental health because it is assumed that each town has various features appropriate to their concrete reality, and therefore "healthy" is defined by agreement with the behavior of most of the population. In this case, the rules are not philosophical or ideological, but statistical, that is, what is considered as abnormal is something that deviates from the average statistical behavior or the general characteristics of a group (Guinsberg, 2001).
For a phenomenon to be considered "normal", statistically speaking, must meet four conditions: a degree of typological uniformity, a certain degree of frequency, a maximum and minimum variation and a certain correspondence between the phenomenon, the context in which it is manifested and the time of manifestation (Pittaluga, 1983).
This perspective is perhaps the most widespread among the entities responsible for defining and guiding policies on mental health at global and regional level, and allows approaching in an explanatory way to the mental situation of the great human conglomerates without being able to move directly their results and conclusions to individual cases.
4. Welfare-discomfort:
From this perspective, the defining criterion of mental health is the assessment that the subject makes of his life, either from a hedonic view (seeking pleasure, avoidance of suffering) or eudaimonic (realization of virtue). While welfare is what allows the subject to be a subjective experience of intrapersonal, interpersonal, social and environmental integration, discomfort indicates a rupture of the subject with himself, with others or with some aspect of family life (work, family, social, environmental) that causes suffering or displeasure. Since mental health refers to a psychological subjective and social welfare the interventions are not intended to supersede the symptoms neither to create an individual totally adjusted to the standards, but to build an individual happily integrated with himself, enthusiastic, efficient, productive, with initiative and imagination, spontaneous, calm and free. (Jervis, 1977).
This alternative responds to an ideographic, subjective perspective, which cannot be universal or objectified and that forces contextual readings through which one tries to understand, from the point of view of the actors, their subjective experience of comfort or discomfort. Accordingly, interventions cannot be standardized, but must be made on an emergency basis, as the assessment is made in each case (Casullo & Castro Solano, 2000).
Discussion
As can be seen, it is not possible to think of an unambiguous relationship between normality and mental health, since in this way, they are generically referencing these concepts obey a vague logic (Calventus, 2000; Munné, 1995), with multiple meanings determined by factors that are of contextual, historical, political, economic and cultural nature. They also include very different anthropological and epistemological elements, and thus conceptual possibilities and radically different intervention.
Thus, the perspective adjusted/maladjusted involves an anthropological perspective in which the individual must conform to the standards and rules established by a collective of which he is part. Therefore, the mental health interventions will aim to achieve the adaptation of the individual to the reference group through educational-instructional strategies or of restrictive type objectively defined and recognized as valid by the group.
In the perspective health/ illness, the human being is assumed as an organism-machine that when ill it will break down, either by an alteration of functional type or because of the attack of some external entity. From this perspective, the intervention in pursuit of mental health should be based on a diagnosis based on nosotaxies and subsequent application of scientific guidelines, defined for each of the disorders, seeking healing disease through biomedical devices.
The statistical perspective of normality/ abnormality is based on the analysis of population data, from which it seeks to impact individuals through normalization strategies trying to return as many possible cases to the range determined by the mean or, in other cases, the diminishment in prevalence and incidences. This perspective has been widely accepted from a utilitarian view of public action, becoming a key factor in the plans, policies and projects that focus their action on mental health.
Finally, the welfare/ discomfort perspective involves a broad anthropological view, that tries to return to the concept of mental health seen from an existential, subjective and ideographic concept, making man "a being in the world" with autonomy and selfmanagement. For these reasons, it is only possible to tell if someone "has" mental health or not according to the reference that the same person makes of their subjective experience. In this manner, that who has mental health concerns who is referred so, framing their assumptions within contextual readings that go deeply into the subjective in inter-subjective relationship frames.
Thus, one has different notions of what a mentally healthy or sick man or woman is, as the antithetical pair from which it is read, with the criterion of demarcation, the context, statistics, the scientific community or the subjective experience. Each, in turn, involves several reference frameworks: social, mathematical, scientific or hermeneutical.
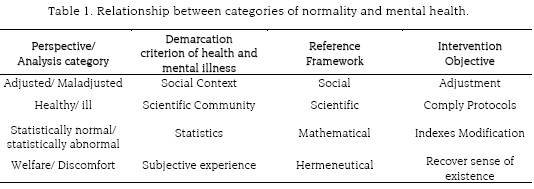
Consequently, interventions that flow from each of these perspectives of normality/abnormality are also diverse: some are aimed at adapting and to changing statistical indexes, compliance with treatment protocols and the recovery of the sense of the existence (Chart 1).
En atención a lo anterior, se hace necesario un abordaje riguroso de la noción de normalidad, tanto en el plano epistemológico como antropológico, para clarificar los discursos y prácticas sobre salud mental en el ámbito científico, profesional y político. A lo anterior se suma la necesidad de una reflexión crítica sobre los intereses ligados a cada una de estas nociones de normalidad y su función en términos de control social. Tabla 1. Relación entre las categorías de normalidad y salud mental.
In response to this, a rigorous approach to the notion of normality, both at epistemological and anthropological level is necessary to clarify the discourses and practices on mental health in the scientific, professional and political fields. To what exposed is added the need for a critical reflection on the interests linked to each of these notions of normality and their role in terms of social control.
Referencias
Ardila, R. (1967). La psicología en Colombia. Interamerican Journal Of Psychology, 1, 239 - 251. [ Links ]
Ardila, R. (2008). Psychology in Latin America. International Journal Of Psychology, 43(3/4), 531. [ Links ]
Berlinguer, G. (1994). La enfermedad: sufrimiento, diferencia, peligro, señal, estímulo. Buenos Aires: Lugar Editorial. [ Links ]
Calventus, J. (2000). La lógica borrosa como aporte a una nueva epistemología en ciencias sociales: una aproximación conceptual. Revista Psicología, 1(2), 1-18. [ Links ]
Canguilhem, G. (1981). Lo normal y lo patológico. México: Siglo XXI Editores. [ Links ]
Canguilhem, G. (2004). Escritos sobre la medicina. Buenos Aires: Amorrortu. [ Links ]
Carrillo Ibarra, J. (2008). La evolución del pensamiento científico, la medicina y las funciones mentales. Revista Mexicana de Neurociencia, 9(1), 61-69. [ Links ]
Casullo, M. M., & Castro Solano, A. (2000). Evaluación del bienestar psicológico en estudiantes adolescentes argentinos. Revista de Psicología, 18, 37-68. [ Links ]
Congreso de Colombia. (2013). Ley 1616 por medio de la cual se expide la ley de Salud Mental y se dictan otras disposiciones. Retrieved from http://www.presidencia.gov.co/Normativa/Leyes/Documents/2013/LEY%201616%20DEL%2021%20DE%20ENERO%20DE%202013.pdf. [ Links ]
Eisenberg, L. (1977). Disease and illness. Distinctions between professional and popular ideas of sickness. Culture, Medicine and Psychiatry, 1(1), 9-23. [ Links ]
Fierro, A. (2000). Salud (comporta) mental: un modelo conceptual. Revista de Psicología General Y Aplicada, 53, 147-163. [ Links ]
Fierro, A. (2004). Salud mental, personalidad sana y madurez personal. Revista UCSD, 4(7), 87-107. [ Links ]
Fierro, A., & Cardenal, V. (1993). Estudio dimensional de la personalidad madura. Revista de Psicología General Y Aplicada, 46(4), 411-419. [ Links ]
Fierro, A., & Cardenal, V. (2001). Pertinencia de estilos de personalidad y variables cognitivas a indicadores de salud mental. Revista de Psicología General Y Aplicada, 54(2), 207-226. [ Links ]
Franz, A. (1970). Historia de la psiquiatría. Barcelona: Expaxs. [ Links ]
García Martín, M. A. (2002). El bienestar subjetivo. Escritos de Psicología, 6, 18-39. [ Links ]
Gómez, R. D. (2002). La noción de "salud pública": Consecuencias de la polisemia. Revista Facultad Nacional de Salud Pública, 20, 101-116. [ Links ]
Gómez, R. D. (2011). Atención primaria en salud y políticas públicas. Revista de La Facultad Nacional de Salud Pública, 28(3), 283 - 293. [ Links ]
Gómez, R. D., & González, E. (2004). Evaluación de la prevención de la enfermedad y la Promoción de la Salud: factores que deben considerarse. Revista de La Facultad Nacional de Salud Pública, 22(1), 87-106. [ Links ]
Gonzalez, E. R. (2007). La salud pública como campo transdisciplinar. Revista Facultad Nacional de Salud Pública, 25(1), 71-77. [ Links ].
Guinsberg, E. (2001). La salud mental en el neoliberalismo. México: Plaza y Janés. [ Links ]
Guinsberg, E. (2007). Salud mental y subjetividad como aspectos sustantivos de la salud colectiva. In E. Jarillo & E. Guinsberg (Eds.), Temas y desafíos en salud colectiva (pp. 245-272). Buenos Aires: Lugar. [ Links ]
Holtz, T. H., Holmes, S., Stonington, S., & Eisenberg, L. (2006). Health Is Still Social: Contemporary Examples in the Age of the Genome. PLoS Medicine, 3(10), e419. http://doi.org/10.1371/journal.pmed.0030419. [ Links ]
Jervis, G. (1977). Manual crítico de psiquiatría. Barcelona: Anagrama. [ Links ]
Mebarak, M., De Castro, A., Salamanca, M. del P., & Quintero, M. F. (2009). Salud mental: un abordaje desde la perspectiva actual de la psicología de la salud. Psicología Desde El Caribe, 23, 83-112. [ Links ]
Ministerio de la Protección Social, & Fundación FES Social. (2005). Estudio Nacional de Salud Mental Colombia 2003. Cali: C&C Gráficas Ltda. [ Links ]
Munné, F. (1995). Las teorías de la complejidad y sus implicaciones en las ciencias del comportamiento. Revista Interamericana de Psicología, 29, 1-12. [ Links ]
Organización Mundial de la Salud [OMS]. (2007). ¿Qué es la salud mental? Retrieved from http://www.who.int/features/qa/62/es/index.html. [ Links ]
Pedrosa-Sanchez, M., & Sola, R. G. (2003). La moderna psicocirugía: un nuevo enfoque de la neurocirugía en la enfermedad psiquiátrica. Revista de Neurología, 36(9), 887-897. [ Links ]
Pittaluga, G. (1983). Temperamento, carácter y personalidad (7a reimp.). México: Fondo de Cultura Económica. [ Links ]
Prince, M., Patel, V., Saxena, S., Maj, M., Maselko, J., Philliphs, M., & Rahman, A. (2007). No health without mental health. Lancet, 370(9590), 859-877. [ Links ]
República de Colombia. Ministerio de Salud. Resolución 2358 de 1998 por la cual se adopta la Política Nacional de Salud Mental (1998). Diario oficial, 43338 (jul. 13 1998). [ Links ]
Rezk, M., & Ardila, R. (1979). Cien años de psicología. México, D.F.: Trillas. [ Links ]
Ricón, L. (1991). Problemas del campo de la salud mental (1a. ed). Buenos Aires: Paidós. [ Links ]
Rodríguez Rossi, R. O. (2005). El hombre como ser social y la conceptualización de la salud mental positiva. Investigación En Salud, 7(2), 105-111. [ Links ]
Rogers, A., & Pilgrim, D. (2010). A sociology of the mental health and illness (4th ed.). United Kingdom: McGraw Hill. [ Links ]
Shorter, E. (1997). A history of psychiatry: from the era of the asylum to the age of Prozac. New York: John Wiley & Sons. [ Links ]
Vergara Quintero, M. del C. (2007). Tres concepciones históricas del proceso salud-enfermedad. Hacia La Promoción de La Salud, 12, 41-50. [ Links ]
Villa Rodriguez, M. A. (2008). ¿Qué es y qué no es la neuropsicología? Revista Mexicana de Neurociencia, 9(3), 227-230. [ Links ]
WHO European Ministerial Conference on Mental Health. (2005). Mental health: facing the challenges, building solutions. Report from the WHO European Ministerial Conference. Copenhagen Denmark: World Health Organization Regional Office for Europe. [ Links ]
World Health Organization [WHO]. (2008). Mental Health Gap Action Programme: scaling up care for mental, neurological, and substance use disorders. Geneva: WHO Press. [ Links ].