Introduction
Despite the widespread of proton pump inhibitors that greatly lowered surgical intervention for peptic ulcer disease, perforated peptic ulcer is remaining a serious life-threatening condition with high morbidity and mortality rates 1. The affected population with perforated peptic ulcer has been changed throughout the history. In the 19th century women had the higher incidence of perforation and it was in the cardia. In the early 20th century middle aged men had a higher incidence of perforated ulcer in the duodenum. Today most patients show increasing age and comorbidities that resulted in higher morbidity and mortality 2.
Perforated peptic ulcer (PPU) is of particular interest to general surgeons because since 1800s, surgery had been remained the standard approach of its management. Omental patch repair is the mainstay of surgical management. It was first described by Johan Mikulicz-Radecki in1885 3.
Leakage after omental patch repair significantly increases postoperative morbidities and carries a high risk of mortality that may reach up to 27% 4. Many risk factors are incriminated in leakage like old age, associated comorbidities, malnutrition, time of presentation, septic shock presentation, extent of peritonitis, site and size of perforation 5.
The aim of our observational study was to detect the main risk factors that may predict the incidence of leakage after omental patch repair in cases of perforated peptic ulcer.
Methods
This retrospective observational study was conducted at Mansoura University Hospital. All patients who had repair of perforated peptic ulcer with omental patch in the period between January 2019 and January 2022 were included.
Inclusion criteria
All patients who had omental patch repair of perforated peptic ulcer either by open or laparoscopic approach.
Exclusion criteria
Patients with perforated peptic ulcer who died in the early postoperative period without evidence of leakage from repair. Also, patients who were operated on because of post-traumatic duodenal or gastric perforation (blunt, penetrating or post ERCP).
Definition
Leakage was defined as failure of healing of duodenal or gastric perforation after omental patch repair within the first 10 postoperative days leading to septic peritonitis that required re-exploration.
Statistical analysis
Patient’s data were retrieved from the patient’s discharge summary reports and medical records during the period of inpatient admission. Patients included in the study were compared as regard to age, gender, associated comorbidities (diabetes mellitus, hypertension, chronic liver disease), interval between onset of symptoms and presentation to the hospital, signs of septic shock upon admission, and preoperative organ failure. Signs of generalized peritonitis, preoperative hypoalbuminemia, site of perforation (duodenal or gastric), and size of perforation (< 0.5cm or >0.5cm) were also assessed.
Postoperative clinical conditions, especially vital signs, need for postoperative ICU admission, and incidence of different postoperative complications were assessed. Laboratory parameters, such as total leucocyte count (TLC) and inflammatory markers as C reactive protein (CRP) were also evaluated. Incidence of leakage, time of incidence, modality of presentation, and investigations done to confirm the leakage were also assessed. All peri and postoperative variables were collected for each patient in the datasheet. Incidence of leakage was reported and data were analyzed accordingly.
Data analysis and interpretation were done using SPSS v-26 (IBM, Armonk, NY). Continuous data were applied in the form of mean and standard deviation or as median and range when applicable, while categorical variables were presented as numbers and percentages. Fisher’s exact test and Pearson’s chi-square test were used to compare categorical variables. Student’s t-test, the Manne Whitney U test, and one-way ANOVA were employed to compare quantitative variables. Potential relative risks for peri and postoperative parameters and predictors of repair leakage were assessed by univariate and multivariate analysis. Risk factors which were statistically significant in univariate analysis were assessed in the form of multivariate analysis so that the factors which level of significance is not below 5% (p<0.05) were excluded.
Results
Out of 128 patients operated by omental patch repair for perforated peptic ulcer, 123 patients were included in our study after exclusion of five patients who did not meet the inclusion criteria. Leakage from the primary site of repair was detected in seven (5.7 %) patients.
Patient’s demographic data and preoperative laboratory results showed that age and gender did not reveal any significant difference between leakage and non-leakage groups whereas patients with associated comorbidities and those presented in severe sepsis or septic shock due to delayed presentation to the hospital had significant higher incidence of leakage. Preoperative laboratory data did not show any difference between both groups except for serum albumin, which was significantly lower in leakage vs non leakage group (Table 1).
Table 1. Preoperative demographic and laboratory data.
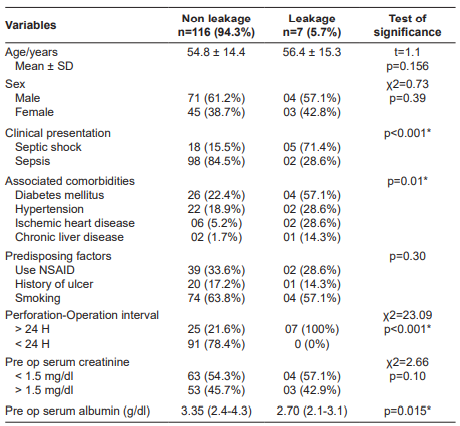
*NSAID: non-steroidal anti-inflammatory drug.
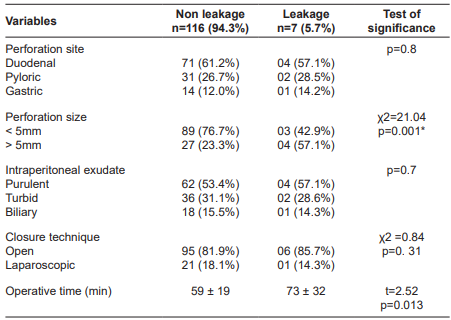
Assessment of intraoperative variables in both groups (Table 2) revealed that the size of perforation significantly affects the healing power so that patients in the leakage group had large size perforation compared to those in non-leakage group and it was statistically significant. Other intraoperative parameters like the site of perforation, nature of intraperitoneal exudate, or operative time did not have any significant difference in both groups.
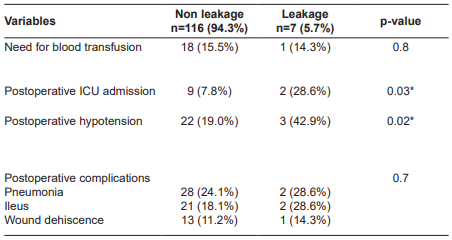
Evaluation of postoperative parameters in both groups showed that leakage incidence was found higher in patients with postoperative hypotension and persistent shock parameters that necessitated ICU admission. The incidence of other postoperative complications and postoperative anemia were of significance in both groups (Table 3).
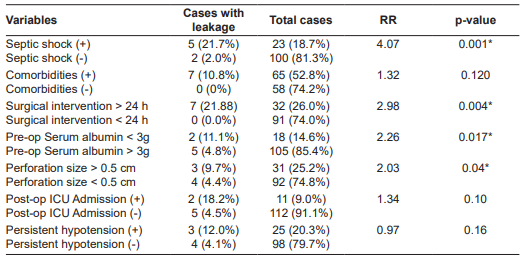
Multivariate analysis of the statistically significant parameters for leakage as shown in Table 4, showed that only presentation in severe septic condition, prolonged perforation, operation interval, preoperative hypoalbuminemia, and perforation size >5mm were found independent risk factors for leakage.
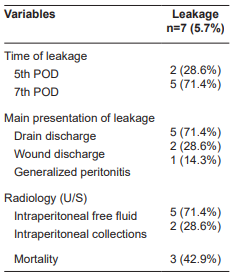
Upon assessment of the data of the patients with leakage as shown in Table 5, leakage had happened during the first week and presented via discharge of biliary secretion thoughout the drain in most of the patients. All the patients had undergone surgical re-exploration, but mortality had occurred in three (42.8%) patients.
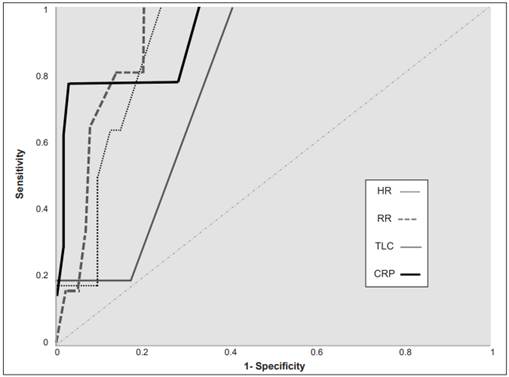
Postoperative clinical and laboratory parameters were compared in both groups as early indicators for leakage as shown in Tables 6 and 7 and figure 1. In the 5th and 7th postoperative day there was significant elevation of TLC and CRP in patients with leakage, with 98% sensitivity and 63% Specificity for TLC, and 80% sensitivity and 89% specificity for CRP predictive value. Also, a significant increase in heart rate and respiratory rate was found in patients with leakage during the 5th and 7th postoperative days. Heart rate had 77% sensitivity and 86% specificity, while respiratory rate had 84% sensitivity and 91% specificity for prediction of leakage (Figure 1).
Table 6. Postoperative clinical and laboratory predictors for leakage.
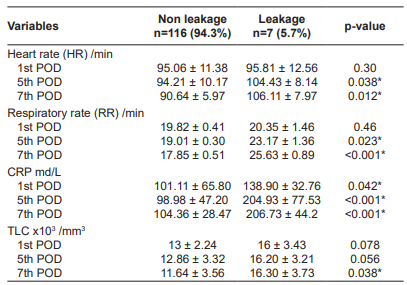
*POD: postoperative day; CRP: C reactive protein; TLC: total leucocyte count.
Table 7. Analysis of predictive clinical and laboratory parameters.
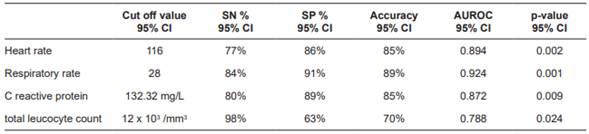
*SN: sensitivity; SP: specificity; AUROC: area under Receiver Operating Characteristic curve.
Discussion
Mikulicz-Radecki in 1880 is refered as the first surgeon repaired a PPU by performing a simple closure of the defect. Early presentation to the hospital, proper diagnosis and urgent surgical intervention are considered as the corner stone for successful management and better outcomes. Leakage after PPU repair is considered one of the devastating postoperative complications that may increase the risk of mortality 6.
The objective of our study was to identify the risk factors for leakage after PPU repair as well as the early predictors for leakage. Retrospective evaluation of 123 patients who were operated for PPU; overall incidence of leakage after omental patch repair was 5.7%.
Upon assessment of preoperative data of our patients, we found that the mean age of the patients who had post opererative leakage was higher than those in non leakage group (56.40± 15.3 vs 54.8 ± 14.4). However, there was no statistically significant difference. Also gender of the patients and the presence of predisposing factors for perforation like smoking or steroids or NSAID use did not have any significant effect on the incidence of postoperative leakage.
Maghsoudi et al. 7, Kumar et al. 8, and Lunevicius et al. 9 reported that patients between 65 and 70 year-old tended to be associated with a higher incidence of post operative morbidity and mortality, but there was no specific relation to the incidence of post op leakage.
In our study, associated comorbidities, presentation in septic shock status, prolonged perforation, operation interval, and preoperative hypoalbuminemia were significant risk factors for leakage, but upon multivariate analysis patient´s comorbidities were ruled out. Wang et al. 10 found that diabetes mellitus, preoperative hypoalbuminemia and septic peritonitis presentation were associated with increased risk of omental patch leakage on univariate analysis only.
Preoperative systolic blood pressure below 90 mmHg and low serum albumin below 2.5 grams/dl were recognized as risk factors for leakage. Serum albumin, was independent risk factors for prediction of releak upon multivariate analysis 8. Lund et al. 11 reported that malnutrition and hypoalbuminemia had been previously identified as a risk factor for increased mortality after PPU repair; this may be secondary to an increased likelihood of development of leak. Weidermann 12 reported that serum albumin level has been shown to be a vital prognostic factor of healing enteric fistulas, and preoperative hypoalbuminemia increased the risk of infection and leak.
Vázquez et al. 13 showed that associated major comorbidities (ASA score 4 and 5), pre-operative shock presentation and delayed surgical intervention were accurate predictors of increased morbidity and mortality after PPU repair.
Lunevicius et al. 14 also reported that delayed septic presentation, prolonged perforation, and operation interval are associated with increased incidence of suture leakage. Our study showed that 74.8% of the patients had a perforation < 5mm in diameter while 25.2% had perforation > 5mm. Leakage was significantly higher in patients with larger perforation size (57.1% vs 23.2%) in non-leakage patients. Kumar et al. 8 reported also perforation size >5mm as an independent risk factor for releak following omental patch repair.
Maghsoudi et al. 7, Wang et al. 10, and Bertleff et al. 15 had found that large perforations are associated with two to three times fold-increased risk of leakage. Gupta et al. 16 recommended that large perforations >2.5 cm better not to be repaired by omental patch because of higher risk of leakage.
The effect of the site of the perforation on the postoperative outcome is a controversial issue. In our study the site of perforation, the nature of intraperitoneal fluid, operative time and the technique (open or laparoscopic) for omental patch repair were not significant risk factors for leakage matching as was reported by Lunevicius et al. 14. On the contrary, Maghsoudi et al. 7 and Lund et al. 11 had reported that significant higher incidence of leakage was found in perforated duodenal (73%) than gastric ulcers (27%) that may be attributed to the difficulty in mobilization and visualization of the perforation during repair.
In our study, the need for postoperative blood transfusion due to intraoperative blood loss was not associated with increased incidence of leakage as reported by Wang et al. 10. Gona et al. 17 also found that hemoglobin level was not a risk factor for development of post operative morbidity and mortality after PPU repair. On the other hand, Kumar et al. 8 considered the hemoglobin level as indepenant risk factor for postoperative leakage.
Although a higher incidence of leakage was noted in patients with postoperative persistence shock parameters that required admission to the surgical ICU in early postoperative period, upon multivariate analysis this was not considered as independent risk factors for leakage. Liu et al. 18 detected significant correlation between shock and incidence of postoperative leakage, while Irwin 19 considered shock as risk factor for leakage in patients older than 70 years.
Diagnosis of leakage from PPU repair was mainly based upon clinical evaluation and it was detected in the 5th and 7th postoperative days. The main presentation of leakage in our study was in the form of biliary discharge from the drain in five patients (71.4%), wound discharge was detected in two patients (28.5%), and generalized peritonitis was detected in only one patient (14.2%). Maghsoudi et al. 7 reported only 4% of the patients with leakage after PPU omental patch had experienced generalized peritonitis. Also, in the study done by Khalil et al. 20, the diagnosis of leakage after omental patch was based mainly on the clinical features, doing an additional investigation like CT is not required in most of the cases. This can be explained by the proximity of perforation site that makes it high output discharge so that can be early and easy to diagnose any leakage.
Luo et al. 21 reported significant increase in the vital signs, especially heart and respiratory rate in patients developed leakage after intestinal surgery consistent with our study, in which there was a significant increase in the mean heart rate during the 3rd (p=0.038) and 5th (p=0.012) postoperative days in patients developed leakage compared to those in non-leakage group. There was also a significant difference in the mean respiratory rate between both groups during the 3rd (p=0.023) and 5th (p<0.001) postoperative days.
Regarding laboratory parameters, we found that the difference between TLC in both groups was only sifnificant on the 5th postoperative day (p=0.038) while CRP level was significantly increased in leakage group on 3rd (p<0.001) and 5th (p<0.001) postoperative days. Elkerkary et al. 22 had demonstrated in their studies the value of CRP, TLC and PCT in predicting leakage following intestinal and colorectal surgeries.
Conclusion
Delayed and septic presentation of patients with PPU especially with large perforation >5 mm are considered as the main risk factors for postoperative leakage. Leakage should be predicted and suspected when patients had tachycardia, tachypnea and elevated serum levels of inflammatory markers (CRP and TLC).