INTRODUCCIÓN
Stump appendicitis is a rare entity, characterized by inflammation of the appendicular remnant after an incomplete appendectomy 1,2; it is not usually considered at first 3, which delays its diagnosis and treatment, causing morbid complications related to an acute abdomen.
The clinical picture is very similar to appendicitis, and it should be suspected in patients with a history of appendectomy. There are several diagnostic aids available in case of doubt, such as ultrasounds and tomography, which in some case series have shown good results. The hypothesis of an increased number of cases in patients undergoing laparoscopic appendectomy generates different opinions and is a controversial issue 4,5,6,7.
This paper presents a case report regarding stump appendicitis in a pediatric patient, as well as a review of the literature. Due to the low incidence of cases, the treatment and recommendations expressed here are based on the experience obtained from case reports; there are no guidelines for the diagnosis and treatment of this entity.
Case report
Two-year old male toddler, admitted to the emergency room with a diagnostic impression of intestinal obstruction. Surgical history included admission to another institution due to acute abdomen six months before the new admission. As a result, he underwent laparotomy, where generalized peritonitis caused by perforated appendicitis was found, as well as intestinal perforation associated with the inflammatory process; in consequence, intestinal resection and end-to-end anastomosis were conducted. Due to sepsis of abdominal origin, the patient required laparostomy with several subsequent peritoneal lavages and hospitalization in the ICU. The patient was discharged in good general conditions, and further data on management are unknown.
At the moment of the consultation, the mother reported symptoms of a day of evolution that began with increasingly diffuse abdominal pain, followed by abdominal distention, multiple episodes of vomiting of gastric contents, and febrile peaks quantified in 39°C, in that order. During physical examination, the patient was found in poor general condition, with grade II dehydration, signs of respiratory distress, alertness, weight of 9.4 kg and vital signs as described in Table 1. The positive findings were enophthalmos; nose with nelaton catheter in permeable right nostril; dry oral mucosa; tachycardia; tachypnea; distended globular abdomen with abolished intestinal noises and tympanic to percussion; voluntary muscular defense, and pain on palpation. Paraclinical tests were requested, yielding the results summarized in Table 2.
Table 1 Vital signs on admission to the emergency room.
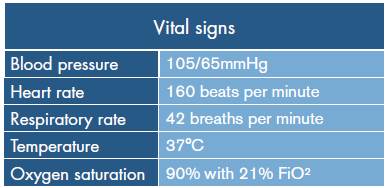
Source: Own elaboration based on the data obtained in the study.
Table 2 Reports of paraclinical tests performed.
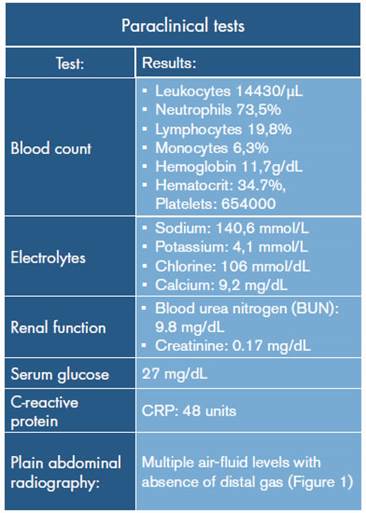
Source: Own elaboration based on the data obtained in the study.
Source: Own elaboration based on the data obtained in the study.
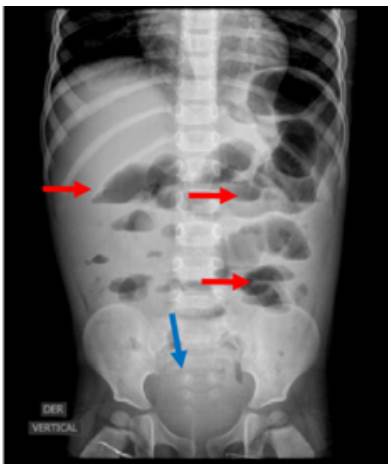
Fig 1 Plain abdominal x-ray (red arrows). Absence of distal gas (blue arrow); air-fluid levels (red levels).
The first suspicion was intestinal obstruction, so a non-surgical medical treatment was initiated. However, the clinical symptoms of the patient were persistent with clinical signs of systemic inflammatory response, and physical examination showed deterioration of abdominal pain despite initial management; for this reason, the patient was referred to the pediatric surgery service for an emergency exploratory laparotomy due to acute abdomen. Performing an abdominal ultrasound or a tomography of the abdomen and pelvis was not possible because of the rapid deterioration of the patient.
The findings during surgery were severe adhesion syndrome, contained intestinal perforation of 5 mm in the anti-mesenteric border at 1 m from the Treitz angle, acute perforated stump appendicitis based on generalized peritonitis (Figure 2), and unperforated Meckel's diverticulum at 50 cm of the ileocecal valve (Figure 3). Based on these findings, laparotomy, appendectomy, generalized peritonitis drainage with cavity lavage, adhesion release, diverticulectomy, enterorrhaphy, and skin closure were performed.
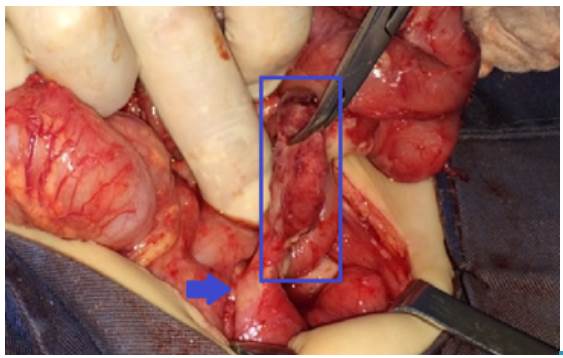
Source: Own elaboration based on the data obtained in the study.
Fig 2 Stump appendicitis, intraoperative findings. The length of the stump, which is greater than 1 cm (blue square), and the cecum (blue arrow) can be seen.

Source: Own elaboration based on the data obtained in the study.
Fig 3 Meckel's diverticulum (blue circle). Intraoperative findings.
The patient was referred to the ICU for postoperative care under the diagnosis of abdominal septic shock; piperacillintazobactam was used for treatment. Subsequently, the patient underwent a new intervention, and two new abdominal cavity lavages were performed. A 14-day antibiotic scheme was completed, and finally, the patient presented satisfactory evolution and was discharged.
DISCUSSION
The main postoperative complications associated with appendectomy include surgical site infection, intra-abdominal abscesses, intestinal perforation, bleeding and adhesions; nevertheless, the frequency of stump appendicitis is low, since only one case is reported in every 50000 patients (0.002%) with a history of appendectomy 6,8 or even less, 0.0014% 9. This figure may be higher since there are cases that are not reported 10, and because only population in general is mentioned, without making a clear distinction of the pediatric population.
Stump appendicitis is a rare cause of acute abdomen in children; therefore, considering this condition is not common for emergency physicians while diagnosing a patient with abdominal pain 5. The length of the appendicular stump 11,12 is considered as a predisposing factor, when the length is equal to or greater than 6 mm 6,13,14. This pathology can appear from 4 days 6,7,15 to 50 years after appendectomy, at any age 1. The review by Bing Tang et al., shows that, until 2010, there were only 10 cases reported in the English literature regarding the pediatric population, ranging between ages 8 and 15, and with an onset of symptomatology between 2 months and 5 years after surgery 13.
Some causes for atypical stump length include extensive inflammation, inadequate surgical exposure, insufficient surgeon experience, or insufficient stump inversion 13. In the case presented here, the extensive inflammatory and necrotic process presented during the acute appendicitis made it difficult for the surgeon to adequately visualize the base of the appendix and, therefore, a long stump was left.
There is a discussion on whether the increase in this entity is related to laparoscopic surgery 6, although there is no proven evidence. Some authors argue that the absence of tactile perception and two-dimensional view predispose to a long appendiceal stump, thus causing a new process of appendicitis 10; however, a retrospective study by Liang et al. showed that 66% of patients presented with a history of open appendectomy 14,16,17,18. The experience at Fundación Hospital de la Misericordia, a pediatric referral hospital where 1348 appendectomies were performed in 2013 and 1100 in 2014, shows that only one case was presented in the mentioned period.
This pathology has a very similar picture to that of acute appendicitis, characterized by abdominal pain (may be predominant in the lower right quadrant), anorexia, vomiting and fever 2,3,5,10,15. About 70% of the cases are associated with perforations generated as complications of the pathology 16, in contrast to 16 to 30% of the perforations caused by acute appendicitis 19. Furthermore, the formation of an infected fistula, inflammatory masses in the lower right quadrant, and presence of signs of peritoneal irritation 13 can be related as well.
In some cases, the condition may present subacute abdominal pain; Roberts et al. concluded, after reviewing different case reports, that abdominal pain is the main symptom and that it occurs in up to 77% of cases 15. Diagnosis is based on clinical suspicion, and the use of diagnostic imaging may help increase certainty 17. Diagnostic aids include ultrasound, tomography, and barium enemas 7,13.
While performing ultrasounds, the same criteria for acute appendicitis can be used to diagnose stump appendicitis: diameter greater than 6 mm in a transverse section of the appendix, edema of the mucosa or presence of a fecolith in the right iliac fossa 2,13,20. Meanwhile, during abdominal-pelvic axial tomography, the findings may be non-specific because of appendectomy or abscess, thickening with inflammatory changes at the base of the cecum, inflammatory mass, increased edema in peripheral adipose tissue and tubular thickening, among others. Tomography is recommended as the initial choice because of the speed with which it can be performed and because it is not a dependent operator 5,7,11,13,14,21.
Barium enema may be useful when abdominal-pelvic tomography is not conclusive, and especially when the surgical incision has had a torpid evolution; with this imaging modality, a pathognomonic sign of "bird-beak" can be observed as an evidence of appendicular retention, although it actually demonstrates the presence of a long stump and not of inflammation. Barium enema is not recommended in the acute phase of the pathology since it can generate perforation and transitively worsen the condition 13. It is important to consider that the images are not diagnostic, but they help the surgeon in decision-making and should always be accompanied by clinical suspicion.
Management in all case reports is always surgical and may be open or laparoscopic depending on the surgeon's decision and the extent of the condition 13. Since this diagnosis is associated with a high rate of complications, it is best to prevent by leaving a stump smaller than 5 mm, since a greater length may cause a fecolith 15,18.
Subramanian et al. propose some recommendations to obtain a "critical view" of the anatomical structures during laparoscopic cholecystectomy, for example, thus reducing to the maximum the chances of a long stump. First, they recommend to clearly locate the union of the cecum with the appendix and transitively the base, for which the teniae coli must be followed to the base, and then, to establish the union of three virtual axes corresponding to the terminal ileum, cecal appendix and teniae coli to obtain the "critical view" of the base; the appendix must be located at 10 o'clock, the teniae coli at 3 o'clock and the terminal ile-um at 6 o'clock. Finally, the mesoappendix can be dissected and the appendicular base can be located more easily 18,22.
The use of antibiotics and the correction of other disorders is at the discretion of the attending physician, who must make a decision according to intraoperative findings and patient evolution. However, post-surgical management and complications are very similar to those of an appendectomy, so it all depends on the surgeon's criteria.
It should be noted that, due to the low incidence of cases, there are no guidelines for the diagnosis and treatment of this entity; therefore, the therapeutic management performed and the recommendations formulated are based on the experience described in the published case reports. The increase in costs is related to the increase in hospitalization days, the need for hospitalization in the ICU in some cases, as well as to surgical reinterventions, and a greater use of medications, among others.
CONCLUSIONS
Stump appendicitis is a rare condition, although it should be considered in patients with abdominal pain and a history of appendectomy, due to the high risk of morbid complications and the possible sequelae, along with increased attention costs. A length greater than 5 mm in the stump has been identified as a risk factor, and some authors associate it with laparoscopic surgery, although there is no evidence to support this assertion.
The clinical picture is similar to classical appendicitis, and some diagnostic images help to reinforce the diagnostic suspicion; tomography is considered the initial examination of choice due to its ease and speed. Management is always surgical and postoperative treatment depends on the surgeon's judgment and surgical findings. As a preventive measure, therefore, leaving a stump equal to or less than 5mm during surgery is advisable, as well as obtaining a critical view of the anatomical structures in order to properly locate the base of the cecum appendix.











 text in
text in 


