INTRODUCTION
Splenic rupture associated with infectious mononucleosis (IM) occurs in 0.1-0.5% of cases and is a very rare complication. Its association with thrombocytopenic purpura is extremely rare, since it only occurs in 0.2-0.6% of the total cases. The causative agent is the Ep-stein-Barr virus (EBV) with positive heterophile antibodies 1,2.
The following case is presented considering the low incidence of this condition and its aggravating influence on a disease that is usually benign.
CASE REPORT
Female 12-years-old mestizo patient from Perote, Mexico, the third child of a healthy 33-year-old mother, eutocic delivery, without perinatal complications. She was a high school student, of low socio-economic conditions and fed with an adequate quantity of food, with predominance of carbohydrates and vegetables. The onset of symptoms occurred 2 days before consultation, presenting with diffuse abdominal pain, distension, nausea, tegument pallor and unquantified fever; in consequence, she was taken to the emergency service of the General Hospital of Zone Number 11 of Instituto Mexicano del Seguro Social in Xalapa, Mexico.
Physical examination revealed tegument pallor, hyperemic oropharynx, tonsil hypertrophy, cervical adenitis, cardiopulmonary signs without compromise, distended abdomen painful on palpation predominantly in left flank with splenomegaly 3-3-3 below costal margin, no hepatomegaly on palpation, peritoneal irritation, diminished peristalsis, petechiae on the limbs and ecchymosis, no edema and good capillary refill. Medical history revealed a traumatic brain injury a year earlier when another child threw a stone that accidentally hit her while they were playing. During that episode, the girl presented with a subarachnoid hematoma that was drained without complications, and was prescribed a treatment with magnesium valproate. Furthermore, she had a history of recurrent upper respiratory infection; the last episode occurred three weeks before developing the current symptoms.
On admission to the emergency service, complementary tests were performed, reporting Hb 7g/dl, Ht 22%, thrombocytopenia 94 000/mm3, leukocytes 5 900/mm3, neutrophils 2 700/mm3, and lymphocytes 2.66/mm3. Liver function tests reported TGO 66 UI/L, TGP 94 IU/L, LDH 1 375 IU/L, prolonged prothrombin time PT of 17.1 seconds, and aPTT 29.5 of seconds. Abdominal ultrasound revealed hepatopathy of origin to be determined, free fluids in cavity greater than 100mL, enlarged spleen (138x74mm) with hypoechoic area in the upper pole suggesting hematoma and accessory splenic lobe. The abdominal X-ray showed distended colon and an image suggestive of splenic hematoma already confirmed by ultrasound.
During her stay in the emergency room, a hematologic assessment was requested, revealing non-immunological thrombocytopenia secondary to hypersplenism. The patient was also assessed by general surgery when hemodynamic instability and hemoglobin decrease were observed, leading to decide an exploratory laparotomy before a possible hemoperitone-um occurred, and was transferred to the operating room.
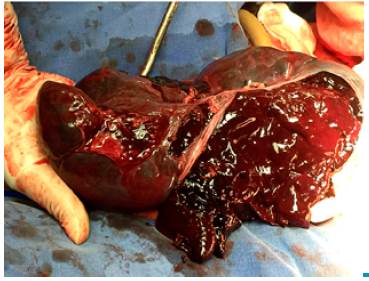
Hemoperitoneum was observed during the surgery, so 4000mL of blood were aspirated and systematic cavity revision was initiated. Splenomegaly (20x10cm), broken subcapsu-lar hematoma and splenic accessory lobe were found (Figure 1). Splenectomy was performed in which broken subcapsular hematoma was observed (Figure 2).
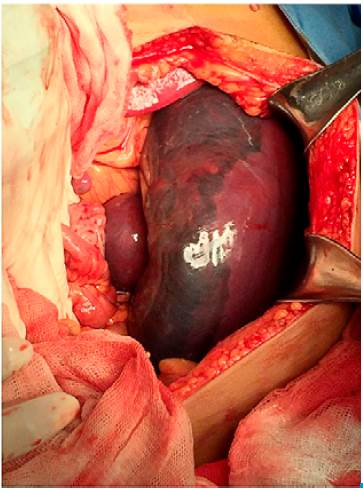
Source: Own elaboration based on the data obtained in the study.
Figure 1 Subcapsular hematoma and splenic accessory lobe.
Three units of erythrocyte concentrates (750mL) were transfused urgently and cefotaxime and metronidazole were administered. Pathology reported chronic passive splenic congestion and subcapsular hematoma.
The Paul-Bunnell test, which yields a positive result when it detects heterophilic antibodies in the blood and a negative result when the suspicion of MI and the investigation of heterophile antibodies are persistent, was positive in this patient, so it was not necessary to look for specific EBV antibodies. The evolution of the patient was satisfactory, the lesions in the lower limbs disappeared, as well as the symptoms. Vaccination against pneumococcus and influenza was applied without complications, ferrous fumarate supplement was administered for 6 months, hospital discharge was given 5 days after the surgery, and the patient was followed by external consultation at one the month, when an adequate health status was observed.
DISCUSSION
Patients with infectious mononucleosis associated with EBV do not require specific therapeutic interventions. This infection occurs at any age, but most cases associated with this virus occur during adolescence or early adulthood. Therefore, the age of the patient has a profound influence on the clinical expression of the infection. Young children tend to present signs such as dermatitis, neutropenia or pneumonia more frequently, while heterophile antibodies are negative in about half of the cases. As age increases, the disease develops more symptoms, with an increase in serological positivity. At 25 years of age, most people are seropositive and not susceptible to reinfection 3.
The typical clinical manifestations of MI are pharyngitis, fever and lymphadenopathy. In more than 50% of cases, pharyngitis is the most frequent symptom and can be severe. The onset may be abrupt, but usually prodromal symptoms occur such as chills, diaphoresis, low-grade fever, anorexia, and malaise 4,5. Fever occurs in more than 90% of patients with MI, usually showing peaks during the afternoon with values of 38-39°C, although they can be up to 40°C; in most cases, the fever resolves within a period of 10 to 14 days 6,7,8.
Dermatitis can be macular, erythematous, petechial, scarlatiniform, urticarial, herpertiform or similar to erythema multiforme, mainly involving the upper limbs and the trunk, and is observed in 5% of patients 9,10. The symptoms are well tolerated and have a low frequency of complications. Most cases have a benign course and patients should receive only symptomatic management and be warned of potential hematological, neurological, cardiac, respiratory, dermatological, renal, splenic, hepatic, immunological and gastrointestinal complications, which, in general, are very rare 11,12.
MI diagnosis is clinical, but laboratory tests are essential to confirm the cause or determine the diagnosis in atypical presentations. The association of heterophile antibodies response during the acute phase of MI was observed by Paul and Bunnell in 1932. They stated that, after infection, 85-90% of the patients produce IgM heterophile antibodies, which agglutinate when they are mixed with ram or horse red blood cells. This procedure was called the Paul-Bunnell test; it was the first serological test developed for this disease, and is currently used to establish a diagnosis. Heterophile antibodies receive this name because they can react with antigens from unrelated species 8,13.
The patient was assessed according to her age group (adolescence) and presented the most symptomatic form of the disease with increased serological positivity, and dermatological and hematological complications with purpuric lesions and ecchymosis in the lower limbs due to a low platelet count. Moreover, she presented thrombocytopenic purpura secondary to infection. Immunological balance breakdown between B lymphocytes and the subtypes of T lymphocytes observed in this patient may lead to the appearance of antibodies against platelets that would explain the purpura. 14.
Trombocytopenia associated with mononucleosis may promote bleeding due to the decrease of the manganese dismutase enzyme. Also, protection against free radicals decreases because of the antibodies, altering the capillary endothelium and increasing the fragility of the spleen, leading to hypersplenism 15.
Subsequently, the patient presented hemodynamic instability with shock, anemia and splenic rupture with ruptured subcapsular hematoma that may have been preceded by an intermittent subcapsular hemorrhage. Splenic rupture is rare and presents as a picture of acute abdominal pain 12; in consequence, an emergency splenectomy was recommended for this patient.
Most cases of infectious mononucleosis are benign and self-limited, and resolve spontaneously within 2-3 weeks 5,10.
CONCLUSION
Spontaneous splenic rupture is a rare complication, but possible due to infectious diseases, being malaria and infectious mononucleosis the most frequent. Appropriate identification and treatment of this emergency requires a multidisciplinary approach and rapid action due to its high morbidity and mortality rates.