INTRODUCTION
SPM is defined as the presence of air in the mediastinum without an apparent secondary cause 1. It is rare, benign and self-limiting, and affects mostly young adults with an average age of 25 years 2, ranging between 13 to 35 3; a study by Cáceres et al.4 reported a similar incidence between men and women. In 1944, Macklin et al. suggested that SPM originates after an alveolar rupture caused by increased intrathoracic pressure, with subsequent passage of air into the interstitium and bronchovascular tissues of the tracheobronchial tree 5.
The most frequent symptoms are chest pain, dysphagia, persistent cough and dyspnea, while risk factors include chronic obstructive pulmonary disease, asthma, and tobacco and illicit drugs use. In addition, precipitating factors such as nausea, vomiting, cough, upper respiratory tract infection and strenuous physical exercise have been observed 3. SPM cases have also been reported as complications of pneumonia by influenza A (H1N1) in children, mainly during the pandemic period of this infection in 2009 6.
The goal of treatment is to control symptoms and may require observation. The length of hospital stay varies from a few hours to several days 2,4. This article presents a SPM case in a young adult.
CASE DESCRIPTION
21-year-old male patient from Garagoa (Boyacá), resident of Bogotá D.C. Colombia, an industrial automation student, mestizo, socioeconomic stratum 3, who presented a clinical picture of four days of evolution consisting of cough with greenish expectoration, dyspnea, chest pain, and unquantified fever. On physical examination he did not have respiratory distress and his vital signs were normal. Bilateral supraclavicular subcutaneous emphysema, decreased vesicular murmur and bilateral intermittent wheezing were identified; no other abnormal findings were observed. The patient had no relevant medical history.
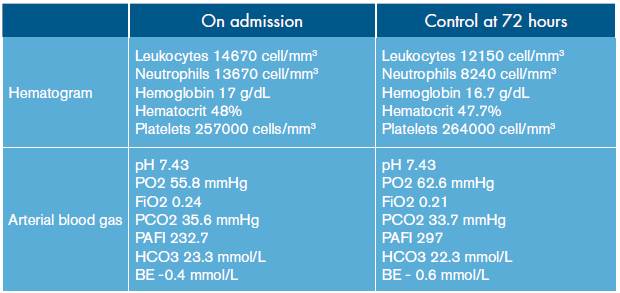
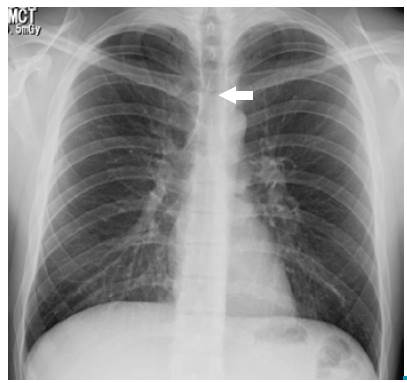
Based on the clinical and epidemiological characteristics, an acute respiratory infection of viral origin was considered; in addition, due to the presence of subcutaneous emphysema and alterations in pulmonary auscultation, spontaneous pneumothorax was suspected. Leukocytosis with neutrophilia and mild oxygenation disorder was found in the requested paraclinical exams (Table 1), while left chest and left supraclavicular soft tissues were observed on the chest radiograph (Figure 1).
Source: Own elaboration based on the data obtained in the study.
Figure 1 PA chest x-ray: pneumomediastinum, delimitation of anatomical structures allowing a neat visualization of its contours (arrow).
Later, a chest tomography was performed, which showed air in the anterior, middle, posterior and superior mediastinum, reaching the lower neck (Figure 2). Due to the absence of risk factors related to secondary causes, SPM secondary to an acute respiratory infection of viral origin was diagnosed; the patient was maintained under observation, and treatment including oxygen through nasal cannula, respiratory therapy, analgesia and rest was indicated.
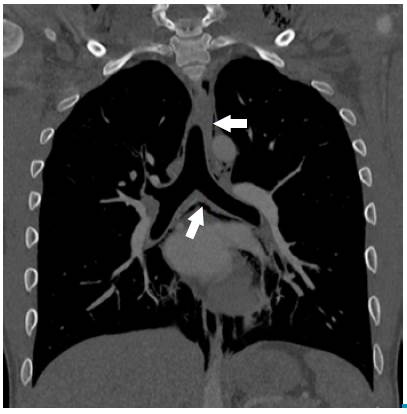
Source: Own elaboration based on the data obtained in the study.
Figure 2 Chest tomography, coronal plane: pneumomediastinum, presence of infracarinal and paratracheal air (sepia arrow). Left supraclavicular subcutaneous emphysema is also observed.
The patient improved during follow-up, period in which leukocytosis and oxygenation disorder were corrected (Table 1), and was discharged after six days of hospitalization. Outpatient radiographic monitoring was requested and he was given recommendations and warning signs. The patient did not present adverse drug reaction or other events during hospitalization.
DISCUSSION
Pneumomediastinum was first reported in 1819 by René Laennec while spontaneous pneumomediastinum was described in 1939 by Louis Hamman 7. Its incidence is less than 0.01% and has a recurrence rate of 1.6% per year 8,9. SPM is a differential diagnosis in patients with chest pain and dyspnea, and is believed to be caused by alveolar rupture due to increased intraalveolar pressure 1,10; therefore, its association with pneumothorax is frequent, being found in 32% of patients 11. In 44% of cases, patients have a history of congestive lung disease, such as asthma, chronic obstructive pulmonary disease, interstitial disease, pulmonary fibrosis, pneumonitis, among others 11.
The mean age at diagnosis is 25 years 11, similar to that of patients with spontaneous pneumothorax 9. In 34% to 49% of the cases, precipitating factors, such as in haled drug abuse, acute respiratory infection, vomiting, asthmatic crisis and intense exercise are observed 9,11.
The most common clinical manifestations include chest pain (68-78.1%), dyspnea (28.1-44%), sore throat (14.1-28%) and cervical pain (54.7%) 9,12. Furthermore, subcutaneous emphysema is the most frequent symptom in about 40 to 100% of patients 9,12,13; in contrast, Hamman's sign (systolic crackle heard with a stethoscope at the left sternal border) is found in only 20% of cases 14,15.
Its presentation is usually masked because of the low specificity of the symptoms and the lack of knowledge of this entity 16. The diagnosis is made based on clinical manifestations and radiological confirmation, in addition to searching for triggers 4,17. 79% of the patients are diagnosed in the emergency room, 11% in the critical care unit, 2% during hospitalization, and 8% in outpatient consultations 11.
Radiological studies of the thorax are important in the evaluation and exclusion of secondary causes 9, and are sufficient to confirm the diagnosis 18. Not all patients with pneumomediastinum require contrast radio-graphic imaging, which is reserved for patients who are suspected of having a tracheobronchial or esophageal injury, especially when vomiting, dysphagia, known gastrointestinal disease, trauma, fever, hemodynamic instability, pleural effusion or pneumoperitoneum are involved 19.
Around 70% to 90% of SPM cases can be identified by chest X-ray 20. The presence of mediastinal air creates an interface with the anatomical structures that allows to visualize its contours neatly. Radiological signs depend on the quantity and location of the air 21: when it surrounds the vascular structures, the ring sign and the tubular artery sign appear. The delimitation of the inner and outer wall of the bronchus is possible due to the presence of intra and extraluminal gas, generating a double wall sign. The continuous diaphragm sign is caused by air posterior to the pericardium.
Other radiological signs include subcutaneous emphysema, radiolucent lines in the upper mediastinum, pneumoprepericardium, "Naclerio V", extrapleural air sign and, thymic wing sign caused by the delimitation of the thymus in children 16,21. Chest tomography delimits the extension of the pneumomediastinum, and provides information about its etiology and differential diagnoses 21,22.
In most cases studies that look for secondary causes are unnecessary, since, in general, there are no alterations of the respiratory or digestive tracts. Advanced diagnostic procedures, restricting diet, administering antibiotics and prolonging hospitalization stay are not appropriate measures 19. SPM has a good prognosis and can be treated conservatively 18, which has shown good results in different studies 2,9,19,23. Such treatment consists of analgesia, rest, oxygen and bronchodilators 24.
In theory, oxygen supplementation is of great importance for treatment, regardless of the presence of an oxygenation disorder, since it increases the pressure of nitrogen diffusion in the interstitium and promotes the absorption of free air 16 accelerating the resolution time.
The mean time of hospitalization is 4.6 days 9 and its management in a critical care unit is unnecessary unless required or in cases in which esophageal rupture is highly suspected 19. Once the patient is discharged, radiological follow-up can be performed until full resolution 16.
The case described here corresponds to a patient, whose epidemiological, clinical and radiological characteristics are the most frequently reported in the literature. This is a typical case that contributes to the diagnostic approach in young patients who present chest pain on arrival to the emergency room. It is important to mention that this case had several limitations, including the lack of microbiological isolation of the germ responsible for the acute respiratory infection, radiological control, and information on outpatient follow-up to objectify the resolution of pneumomediastinum. However, this report is important because it illustrates a radiologically confirmed clinical case of a rare disease causing chest pain.