INTRODUCTION
Marfan syndrome is a rare connective tissue disorder that equally affects men and women (autosomal dominant), with an approximate incidence rate of 1 in 5 000 people. It is characterized by an alteration in the production of fibrillin due to a mutation in the FBN1 gene of chromosome 15, which weakens the connective tissue of the body, whether tendinous, ligamentous, cartilaginous, vascular or heart valves. 1. It is worth noting that not all patients with this syndrome develop the same symptoms or severity (allelic heterogeneity) 2. Since the aorta wall is weak, a dilatation of the aorta occurs leading to an aortic aneurysm. In addition, if there is a rupture in the vascular wall, a double lumen may be formed, with the consequent passage of blood, which is called aortic dissection.
Acute thoracic aortic dissection is the result of a tear in the wall of the aorta that allows blood flow between its layers separating them, which leads to the appearance of a double light within the same vessel, causing the blood flow through a false light to exert an occlusive effect on the light itself and condition the flow to the vessels that derive directly from the aorta. The importance of early diagnosis directly affects the chances of survival, since it is a medical emergency that can lead to death, even with optimal treatment.
The Stanford classification is used to better understand aortic dissection. It is divided into types A and B. Group A includes the dissections that involve the ascending aorta, which is why they are considered to pose higher risk because the dissection and false light that is generated can rapidly affect the coronary ostium and compromise the blood flow to the myocardium, leading to a massive and fulminating infarction, hence the importance of timely diagnosis and appropriate surgical treatment.
In many cases, if the aortic root is dilated, and depending on the degree of the dilation, the apparatus of the aortic valve is affected, which implies a backward flow of blood to the ventricles with the consequent decrease in the volume of ventricular ejection. To compensate this anomaly, the cavities of the heart increase their size, in other words, a cardiac dilation occurs.
The estimated mortality rate for type A aortic dissection is directly related to the time of evolution, being of 1% per hour within the first 24 hours, 29% at 48 hours, 44% after a week, and reaching 50% at two weeks. Therefore, emergency surgery is the best option.
Despite the advances for early diagnosis and the innovations in surgical management, type A aortic dissection of the ascending aorta has a high morbidity and mortality both in the short term and in the long term: at the hospital level, it ranges between 15% and 35%, with a 5-year survival rate in 65-75% of cases.
Type B dissections involve the aorta posterior to the left subclavian artery, with no compromise of the ascending aorta. Usually, its management is not urgent, although it is equally important since relevant organs may also be affected, in which case other therapeutic options should be analyzed.
CASE PRESENTATION
26-year-old male, mestizo, single patient from Guayaquil (Ecuador), with a basic level of education, a history of Marfan syndrome and hypertension in treatment, who attended consultation reporting a clinical picture of 48 hours of evolution characterized by intense lancinating retrosternal pain and medium effort dyspnea that evolved to orthopnea. The vital signs on admission obtained after physical examination were: BP: 120/50 mmHg, HR: 108/min, RR: 22/ min, oxygen saturation: 95%, temperature: 35.4°C, and height: 180 cm. He presented with disproportionate upper limbs in relation to thoracoabdominal structure, pale skin, aranodactyly, perioral cyanosis, and piriform thorax with sternal depression. Auscultation revealed systolic and diastolic murmur and mitral systolic murmur.
Complementary diagnostic exams
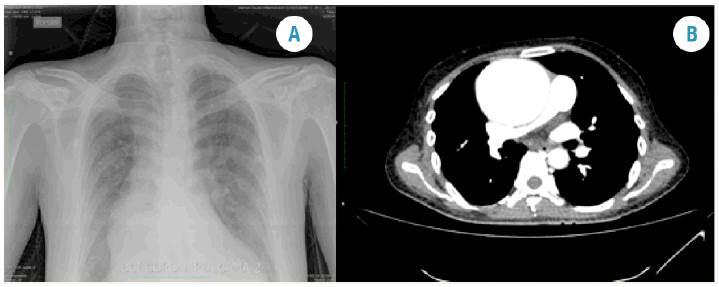
Chest x-ray: cardiomegaly, mediastinal widening at the expense of ascending aorta (Figure 1a).
Electrocardiogram: sinus tachycardia, left ventricular hypertrophy with signs of diastolic overload.
Echocardiogram: significant aortic valve regurgitation with severe dilatation of the valve ring.
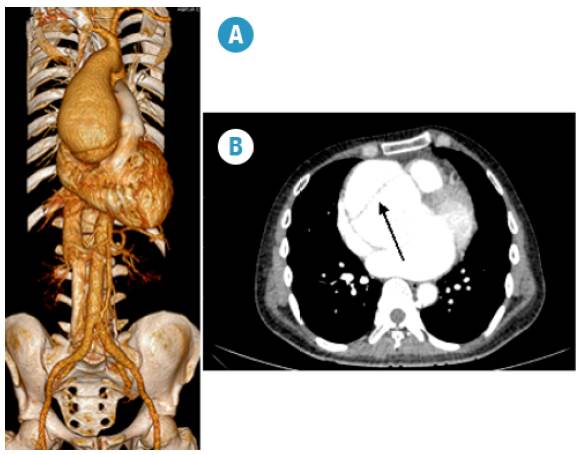
Computed tomography angiogram of the chest: aortic root of 90.2 mm, ascending aorta of 80.8 mm, double lumen observed at aortic root level correlating with aortic dissection (inti-mal flap) with visible leakage of contrast material towards false lumen. Normal mitral, tricuspid and pulmonary valves; insufficient tricuspid aortic valve and increased pulmonary systolic pressure (60 mmHg) (Figures 1b and 2).
Source: Own elaboration based on the data obtained in the study.
Fig 1A Posteroanterior chest radiograph. Grade 4 cardiomegaly and mediastinal widening at the expense of ascending aorta. Fig 1B. Computed tomography angiography: sagittal section. Aortic root of 90.2 mm, ascending aorta of 80.8 mm, insufficient tricuspid aortic valve and increased pulmonary systolic pressure (60 mmHg).
Source: Own elaboration based on the data obtained in the study.
Fig 2A 3D reconstruction of computed tomography angiography of the chest. Dilation of the ascending aorta. Aortic root 90.2 mm, anteroposterior diameter of ascending aorta of 80.8 mm. Fig 2B. Arrow. Intimal flap.
Evolution
One of the most important aspects is the length of hospital stay, since this is directly related to morbidity and mortality. In this case, approximately 48 hours passed between the completion of the complementary examinations, the confirmation of Stanford type A ascending aortic dissection as definitive diagnosis, and the decision to start surgical treatment through Bentall and De Bono surgery, which represented an increase of about 29% in the mortality rate.
The clinical management of the patient was holistic, and one of the parameters actively treated was blood pressure through carvedilol 6.25 mg VOc/12h, which kept the values within normality ranges.
Surgical procedure
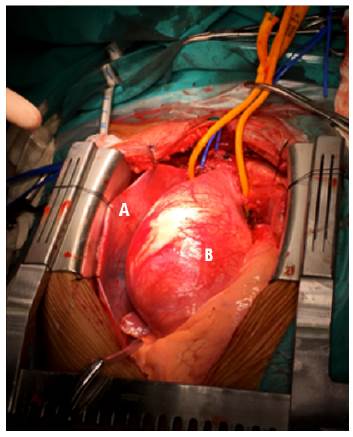
Once the patient was under general anesthesia and strict asepsis, proximal and distal control of the right axillary artery was performed by cannulation for extracorporeal circulation (ECC), followed by medial stereotomy, exposing the pericardial sac through an inverted T incision, which exposed the ascending aortic aneurysm from the aortic annulus, with a diameter greater than 100 mm that deformed the base of the heart and extended to the distal third of the ascending aorta. Cardiomegaly IV/IV was found in both right and left cavities, along with global dilation of the ventricles and intraoperative pulmonary artery pressure over 60 mmHg according to Swan-Ganz catheter measurements.
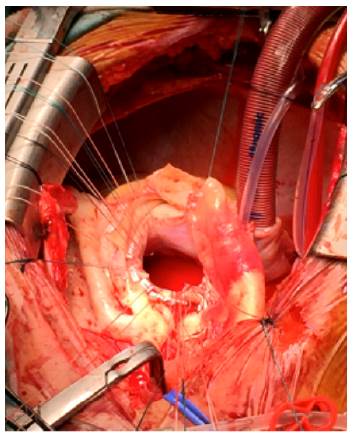
The extracorporeal circulation entrance was then isolated by aortic clamping and the dissected aortic wall was opened longitudinally, which allowed to identify false and true lumen. Then, through a partial resection of the dissection focus, the distal end of the aorta was verified and the false lumen was sealed with BioGlue 1. Resection of the tricuspid aortic valve was continued, isolating left and right coronary buttons and implanting a valved tube sj # 27. Once the normal function of the prosthetic discs was confirmed, the left and right coronary button reimplant was placed and its permeability was checked. Immediately, distal anastomosis was performed from the valved tube to the distal ascending aorta. Finally, a prosthetic neo-ostium venous bypass implant was placed since the right coronary button was unstructured with suture dehiscence, which caused an acute intraoperative myocardial infarction.
Upon removing ECC, acute right ventricular distension and sustained ventricular fibrillation were observed, which required de-fibrillation (20-30 joules) together with antiarrhythmic therapy. Finally, arrhythmia was controlled. The patient presented three episodes of ventricular fibrillation which responded to electrical cardioversion.
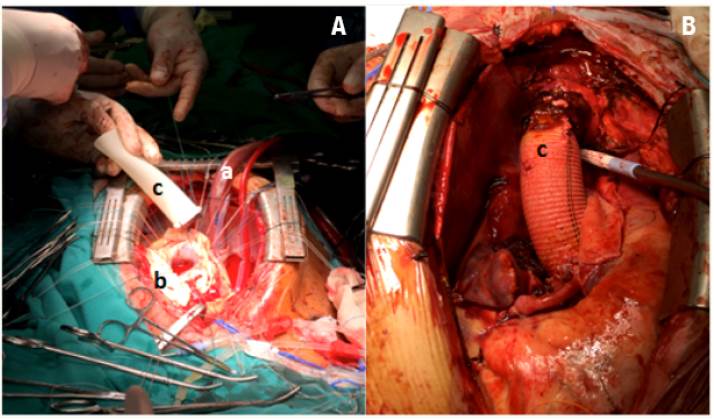
ECC removal was attempted on three occasions, but low expenditure was observed despite maximum inotropic support, then the patient suffered refractory ventricular fibrillation and later asystole despite an epicardial pacemaker and died. The aortic clamping time was 150min and ECC time, 305 min (Figures 3, 4 and 5).
Source: Own elaboration based on the data obtained in the study.
Fig 3 Surgery. Exposure by median sternotomy. A. Pericardial sac. B. Aneurysmal ascending aorta.
Source: Own elaboration based on the data obtained in the study.
Fig 4 Exposure of the aortic ring with appropriate fixation points for subsequent placement of prosthetic
Source: Own elaboration based on the data obtained in the study.
Fig 5A Exposure of the aortic ring with the appropriate fixation points after prosthesis placement. Fig 5b. Replacement of the aortic root using composite prosthesis and Bentall coronary reconstruction. a: extracorporeal circulation system. b: aortic ring with corresponding fixation points. c: prosthetic material.
DISCUSSION
The Marfan syndrome is an autosomal dominant pathology with a relatively low frequency, which tends to cardiovascular complications in most cases. The evolution of Marfan syndrome leads to an aneurysmal dilation of the aorta, which may be added to a rupture of its wall with the subsequent development of aortic dissection. In this case, a type A dissection was diagnosed based on the Stanford classification, the most frequently used nowadays, or DeBakey type II 3.
The ascending aortic aneurysms have a relatively low prevalence, as well as an important variability that can be accompanied by an aortic dissection or rupture of the aorta, increasing its mortality rate to almost 100%. The complications observed in the patients who suffer from this condition are closely related to the diameter of the aorta, its growth rate and the time of evolution. In vessels with a diameter greater than 5 cm, the risk of rupture and dissection increases by up to 45% 4. The symptomatology is variable and depends on the type of aneurysm, as well as on its location and relationship with neighboring structures. An aortic aneurysm can cause fatigue, hoarse or strained voice and pain in the left shoulder. If it is accompanied by aortic dissection, it can cause intense lancinating pain in the anterior chest, which usually radiates towards the back in the interscapular region.
Aortic dissection is characterized by the creation of a false lumen in the middle layer of the aortic wall. It is classified according to the presence and location of the first tears, as well as the retrograde or anterograde extension of the dissection 5.
If coronary vessels are compromised since birth, associated acute coronary syndrome symptoms are added, which constitutes an emergency and modifies both the management and the necessary times.
Opting for surgical treatment depends on several factors and choice is based on the anatomical conditions of the aorta, the underlying disease, the risk of anticoagulation, the age of the patient, the presence of an active infection, among others. Several surgical techniques have been developed that reflect the evolution in the management of the ascending aortic aneurysms; each has its own advantages, limitations and risks. The replacement of the aortic root and the ascending aorta with valved tubular grafts, known as the Bentall procedure, along with annuloaortic ectasia is the most appropriate choice of the treatment for this condition. 6.
The literature reports that the Bentall procedure has a low morbidity and a mortality of 13%, being septic shock and ventricular fibrillation the most common causes of death 7. These figures vary considerably depending on the moment when surgery is performed: if surgery is scheduled, mortality rates range between 1.7% and 17.1%, but if surgery is the consequence of an emergency, the values increase to between 23% and 50% 7. The survival rate at 5 years ranges between 73 and 92%, while survival at 10 years is between 60 and 73% 8. However, surgical mortality can vary greatly depending on the hospital center, the experience of the medical team, the available resources and the heterogeneity of the patients 9. It is worth noting that dissection distal to the operated segment persists in 60% to 75% of the patients who undergo a dissection of the ascending aorta 10.
Due to its comorbidity rates and its degree of evolution, Bentall procedure is the most favorable choice for this type of patients. In this case, the procedure consisted in performing a prosthetic replacement that compensated aortic valve deficiency as a result of the large dilatation of the aortic annulus and subsequent replacement of the damaged aortic wall. Finally, the aortic buttons were reimplanted to the prosthesis.
However, there are other surgical options. For example, David's technique, developed by the Canadian surgeon Tirone David in 1992, achieves a greater stabilization of all the components of the root of the aorta, which requires the proper function of the aortic valve 6. In this case, the patient had a large dilatation of the aortic annulus that made this procedure difficult to use.
It is important to consider the need for developing new therapeutic options for this type of patients in order to improve their survival rates and quality of life.
CONCLUSION
The case reported here demonstrates that the treatment of patients with Marfan syndrome should be done from a multidisciplinary and joint approach, where timely diagnosis together with follow-up by specialized services and a qualified team allow a timely action and, thus, avoid that the patients with this condition look for care when it is already at a late stage.














