INTRODUCTION
Carl Freiherr von Rokitansky, Austrian anatomo-pathologist, first described appendiceal mucocele in 1842 1. It is defined as a cystic dilatation of the vermiform appendix, whose causes include benign and/or malignant processes. It has a low incidence estimated at around 0.3% of appendectomies 2,3. From a histological perspective, it can be classified into four types: simple mucocele (accumulation of mucus in the appendicular cavity with obstruction), focal or diffuse hyperplasia of the mucosa, mucinous cystadenoma, and mucinous cystadenocarcinoma; when a spontaneous perforation of the appendix occurs, pseudomyxoma peritonei can be observed 4.
The clinical picture is not necessarily characteristic, since it can be asymptomatic and, in some cases, it is incidentally discovered through radiological-endoscopic studies or during surgical procedures. Half of the cases present pain in the right iliac fossa 5. This can be a benign or malignant process, so each case must be individualized to know its nature. Complications are rare and include intestinal obstruction or digestive bleeding, being peritoneal pseudomyxoma the most severe form, which occurs when mucinous material disseminates in the peritoneum.
The preoperative diagnosis is essential for planning the surgery and includes imaging techniques such as ultrasound and contrasted tomography (CT) of the abdomen and pelvis, which allow a better characterization of the tumor. An ultrasound can confirm the cystic aspect, while abdominal and pelvic CT scan with contrast defines the wall, the presence of calcifications and the density of the content. Other tests available, although less useful for diagnosis, are barium enema and colonoscopy 6,7.
The treatment indicated for appendiceal mucocele is the surgical removal of the appendix, even if the affected mucocele compromises the terminal ileum or the cecum. Cystadenocarcinoma cases with mesenteric involvement or an adjacent organ require hemicolectomy 8.
The objective of this work is to report a case of this rare pathology, discuss its particular characteristics and present a brief literature review.
CLINICAL CASE
69-year-old mestizo, male patient, without a relevant medical history, who attended the emergency room with a clinical picture of 5 days of evolution characterized by colicky abdominal pain of slight intensity, which progressed to moderate, at the right iliac fossa level. The pain was accompanied by nausea, malaise and unquantified fever.
The patient reported that he was unable to pass flatus and was constipated, which led him to self-medicate with oral analgesics. After realizing that the picture did not improve, he decided to visit the emergency room of the Luis Vernaza Hospital. Physical examination showed the following vital signs: blood pressure 140/80 mmHg, heart rate 103 bpm, SpO2 98%, temperature 37.5°C, conscious state, orientation in space, time, and person, afebrile and semi-moist mucous membranes. The abdomen was soft, depressible, and painful in the right iliac fossa, with positive McBurney's point and Blumberg's sign. The results of the laboratory tests were: leukocytes 10,440/ul, segmented of 76.1%, and CRP: 249.97 mg /L.
An abdominal ultrasonography was performed, which showed a dilatation of the cecal appendix of 93.9mm x 35.9mm, thickening of the wall and laminar fluid in the right iliac fossa (Figure 1).
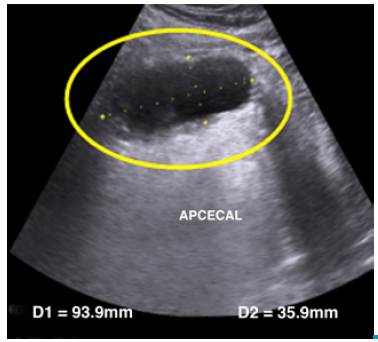
Source: Own elaboration based on the data obtained in the study.
Figure 1 Abdominal ultrasound: dilatation of the cecal appendix (circle).
An exploratory laparotomy was decided with conventional appendectomy plus raffia with appendicular base, similar to the Parker-Kerr technique. Findings included appendiceal tumors with a wide base of thick walls and mucoid content. The samples taken were sent to pathology (Figure 2).
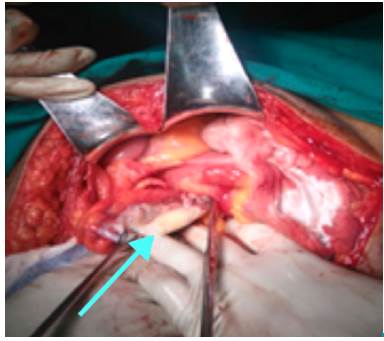
Source: Own elaboration based on the data obtained in the study.
Figure 2 Sample of dilated cecal appendix compatible with mucocele.
The macroscopic study revealed a cecal appendix of 8x6x5cm, appendiceal space reaching 4.5cm in diameter, and serous surface completely occupied by a whitish plate with fibrinous appearance. The parietal bone thickness ranged between 0.2 and 1 cm (Figure 3).
The histopathological study showed a cecal appendix with coagulative necrosis in the mucosa and the wall, mucous membrane with focal mucoid deposit that did not invade the parietal thickness, fibrinonecrotic and hemorrhagic exudate that extended to serosa and periapendicular mesentery, and multiple microabscesses. The final diagnosis was acute gangrenous appendicitis and appendiceal mucocele. Finally, the patient was discharged after 8 days, without further complications.
DISCUSSION
Appendiceal mucocele is a cystic dilatation of the appendiceal lumen with accumulation of mucus. It is caused by an obstruction of the appendix due to the excessive accumulation of mucus with abnormal dilatation. However, the term mucocele does not describe the potential aggressiveness or biological behavior and, therefore, is a descriptive term that does not have a diagnostic character and does not correspond to a defined clinical-pathological entity.
Appendiceal mucocele is a rare pathology, found in 0.2% to 0.3% of appendectomies, which corresponds to 8% of the total appendiceal tumors, with a higher incidence in women (ratio 4: 1) and average age of presentation of 55 years 9,10.
This report describes the case of 69-year-old male patient, that is, in the seventh decade of life, which coincides with the literature. The pathology report revealed simple mucocele, which is found in 20% of cases 11. The histopathological result described acute gangrenous appendicitis and acute fibrinopurulent periappendicitis, appendiceal mucocele and omentum without histopathological alterations.
The form of presentation is non-specific and incidentally appears in 25% of cases. The most frequent symptoms include abdominal pain (27%), palpable abdominal mass (50%), weight loss (13%), nausea or vomiting (9%), and less frequently, dysuria, hematuria or complications such as perforation 12, bleeding, intussusception or torsion 13.
This patient presented a picture similar to acute appendicitis with pain in the right iliac fossa, anorexia, nausea, and positive Mc Burney' point and Blumberg's sign, which led to a differential diagnosis of acute appendicitis, which is very frequent.
Laboratory tests may be useful to determine an infectious disease, but not to suspect mucocele. For this reason, it is advisable to perform imaging tests, including ultrasounds, which, in this case, served to observe an elongated and tubular structure (also known as chicken drumstick) compatible with the appendix, with a diameter greater than 1.5cm, a thin wall and calcifications 14. Nuclear magnetic resonance (NMR) is also useful for studying this picture. In this case, ultrasound showed a dilated tubular image, with a diameter of 35mm, which led to suspect appendiceal mucocele, although the result was not conclusive.
The treatment for this entity is surgical by laparotomy or laparoscopy; the careful handling of the piece is very important to avoid its rupture and consequent dissemination (pseudomyxoma peritonei). When only the appendix is affected without local or cecal invasion, it can be treated with appendectomy and mesoappendix excision, but if the caecum or an adjacent organ is involved, a right hemicolectomy should be performed 5.
Since the condition of the patient resembled an acute abdomen of 5 days of evolution, an exploratory laparotomy was performed, in which a dilated tumor-like appendix was found, as well as necrosis in its lower third and broad base, which led to suspect mucocele. The caecum was in good condition, so a conventional appendectomy was performed.
The patient was finally discharged at 8 days without further complications.
The final result was mucocele without histopathological alteration of the omentum. Based on this finding, periodic check-ups by external consultation were indicated without the need to perform any other surgical procedure until now.
CONCLUSION
Mucocele has a low incidence of 0.2-0.3% among the total of appendectomies. The treatment is surgical due to the potential risk of malignant transformation and to prevent other complications such as rupture and dissemination. It is important to consider the diagnosis prior to surgery and to perform a careful resection, either by laparoscopy or laparotomy.















