INTRODUCTION
Gastroschisis can be defined as a congenital defect of the anterior abdominal wall, characterized by evisceration of the abdominal organs through an opening in the absence of membranous coverage; this defect is usually observed to the right of the navel 1-3, involving, in all cases, the small intestine 3 and sometimes the stomach, colon or gonads. 1,3 As they are not covered by membranes, the eviscerated structures are exposed to amniotic fluid and external substances after birth, which increases the risk of infection and injuries. 1,3,4 This is a low-prevalence disease 5-7 of great importance due to the excellent prognosis and survival of patients 8-10 when providing adequate management. 11,12
CASE PRESENTATION
This paper reports the case of a full-term male infant born at 37 weeks, who was transferred from Florencia, Colombia to the Neonatology Service. The child was born by vaginal delivery at a primary care center, with an incidental finding of protruding, violaceous and wet intestinal loops, associated with respiratory distress.
The patient received oxygen therapy through cannula and nasogastric tube. Ophthalmic prophylaxis was performed and then, he was referred to a secondary care institution, where gastric lavage was performed, a polyethylene bag was placed, and antibiotic treatment with ampicillin-gentamicin was initiated. Ringer's lactate solution and dextrose 10% in distilled water at 100 cm3/kg/day were administered with a metabolic flow of 6.7 mg/kg/min, and inotropic management was initiated due to hemodynamic instability. The child was referred to a tertiary care institution for management by Pediatric Surgery.
The child was the firstborn of a teenager (17 years old) with O+ blood type, who underwent eight prenatal care checkups, serology and protocol blood tests with negative results. Obstetric ultrasounds at weeks 19 and 29 of pregnancy did not report alterations and fetal movements were positive since month two. The infant was a vaginal delivery product with cephalic presentation and without premature rupture of ovular membranes; Apgar: 6/8/10. The child was fully vaccinated. No pathological, infectious, pharmacological or transfusion history were observed other than maternal poisoning during the first trimester of pregnancy with insecticide, since the mother lives in an area where constant fumigations are performed.
On physical examination, the patient presented with stable vital signs and normal anthropometric measurements (abdominal perimeter was not assessed due to the protrusion of intestinal loops). The thorax showed a slight intercostal retraction and the abdomen, a protrusion of intestinal loops covered with a viaflex container, pink, well perfused and with a foul odor; the skin was pale and poorly perfused.
Table 1 Synthesis of the evolution of the patient.
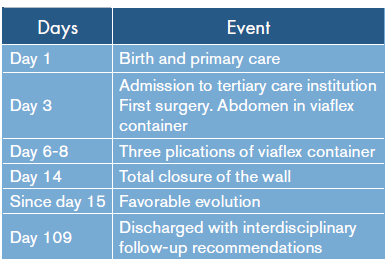
Source: Own elaboration based on the data obtained in the study
Based on clinical findings, gastroschisis, respiratory distress syndrome and early neonatal sepsis were diagnosed. Renal ultrasound and echocardiogram were requested to rule out associated congenital malformations; the results were normal. Clinical genetics determined a chemical teratogenic disruptive process during the first trimester of pregnancy as probable etiology. Taking into account his history, a k-band karyotype was requested, which was not authorized by the health service provider, so it was not possible to use it as a diagnostic tool to establish management. This case report does not address the importance of the denied examination.
The patient required mechanical ventilation and inotropic support. The Pediatric Surgery Service proposed closing the abdominal wall gradually and adding metronidazole to antibiotic management. During surgery, severe gastro schisis was found with exposure of stomach, small and large intestines, intestinal malrotation with thickened meso, and leaky and thickened intestine due to intrauterine exposure.
The umbilical border was cleared, the umbilical and vesical arteries were ligated and a Bogota bag was attached to the skin covered with gauze impregnated with Furacin®.
The procedure was well tolerated at first, but a deterioration of the clinical condition was observed subsequently with hemodynamic instability, which required inotropic support with dopamine and dobutamine; mechanical ventilation with high parameters; sedation with fentanyl and morphine; relaxation with rocuronium, and follow-up with antibiotic therapy with ampicillingentamicin and metronidazole.
The Pediatric Surgery Service decided to perform plications of the viaflex container. The first was done 3 days after the first surgery and the second and third were performed at intervals of 24 hours after the first plication.
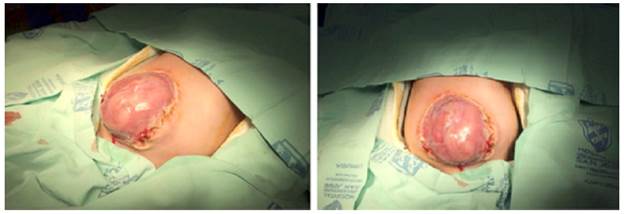
A second surgery was planned 24-48 hours after the last plication. However, chest x-ray findings were interpreted as possible acute disseminated candidiasis, so the procedure was postponed. Pediatric Pneumology ruled out said infection, so the second surgery was performed 4 days after the last plication (Figure 1). During the procedure, gastroschisis was corrected with myocutaneous and fasciocutaneous flap. After removing the viaflex container, a thickened, dysmorphic and malrotated intestine was observed.
If gastroschisis is a small defect (only a part of the intestines protrudes from the abdomen), it is usually treated with surgery soon after birth (Figure 1). However, if gastroschisis is a large defect (many organs protrude from the abdomen), repair could be done slowly, in stages, covering the exposed organs with a special material and placing them slowly in the abdomen. After the organs have been arranged inside the abdomen, the opening is closed.
In the postoperative period, the patient remained hemodynamically stable, achieving inotropic and vasoactive weaning. Pharmacological relaxation and morphine were discontinued and fentanyl was administered only at analgesic doses. Mechanical ventilation was continued in a controlled assisted manner with minimal parameters and intra-abdominal pressure between 6-11 mmHg. Trophic stimulation with dextrose at 5% was initiated.
The patient remained hospitalized for 109 days; his evolution was satisfactory and the food was well tolerated with normal stools and adequate weight gain (reaching 3 875 grams). The patient was discharged with breastfeeding on demand, supplemented extensively with hydrolyzed milk formula. Currently, the child continues to be monitored by Highrisk Pediatrics, Clinical Genetics, Pediatric Cardiology and Nutrition.
DISCUSSION
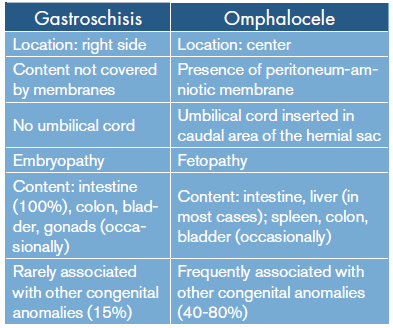
The first gastroschisis report was published in 1773. 4,6 Around 1894, Taruffi coined this term to group diseases of different etiology (omphalocele, bladder exstrophy, amniotic hernia, gastroschisis). 4 The distinction between gastroschisis and other abdominal wall defects, especially omphalocele, was successfully achieved at the beginning of the 21st century with the implementation of the International Classification of Diseases, tenth edition (ICD-10). 4 Table 2 summarizes the differences between gastroschisis and omphalocele. 1-3,5,6
EPIDEMIOLOGY
In recent decades, the incidence of gastroschisis has increased worldwide 1,5,10 and is observed in 1/3 000 to 1/10 000 births. A review of the 1991-2001period in the Clinical Hospital of the University of Chile showed that the figure was 2.1/10 000 births. 1-4 In Colombia, an incidence of 7.8/10 000 births was reported, more frequently seen in 37-week-old male newborns. 13,14 The risk factors associated with the disease are prematurity; small for gestational age newborns; maternal age <20 years; being born to a primigravida mother; Caucasian race; Hispanic mothers; maternal malnutrition; exposure to nitrosamines; teratogens and agrochemicals; consumption of nonsteroidal anti-inflammatory drugs and acetaminophen in the first trimester; cigarette, alcohol and illicit drugs consumption; low socioeconomic class; absence of prenatal checkups, and short cohabitation with the father of the child. 1,2,5,7-11,13 The average age of mothers with affected children is 21.1 years; women aged 14 to 19 have a 7.2 times higher risk of having a child with gastroschisis compared to 25 to 29-year-old mothers. 15
It should be noted that the mother of the studied patient was 17 years old, primigravida, exposed to a toxic substance (insecticide) in the first trimester of pregnancy and of low socioeconomic status.
ETIOPATHOGENESIS
There is no certainty about the exact cause of gastroschisis, since it is a multifactorial disease. Embryologically, the abdominal wall originates from the lateral mesoderm and by the fusion of four folds (cephalic, caudal and two lateral foldings), which grow towards the midline, con verging in the umbilical ring that is completed around the fourth week. 2,12
Current accepted causal theories affirm that gastroschisis is caused by vascular disruptions, either by intrauterine occlusion of the omphalomesenteric artery or by early atrophy (<28 days) of the right umbilical vein, which causes wall infarction with rupture of the umbilical ring and eventration of the intestine. 2,16-18
A new theory proposes that there is a defect in the inclusion of the yolk sac in the fetal body stem, with the consequent formation of an additional opening through which the intestine is eventracted, instead of doing it through the umbilical cord. 16-18 The final outcome is the eventration of abdominal contents in utero that, regardless of the size and quantity of viscera exposed, is associated with a mortality of 5% and 3-15% after birth. 5,7,8,12 However, these deaths may be associated with complications and significant morbidity, prolonged hospital stays, need for mechanical ventilation, prolonged parenteral nutrition, multiple surgical interventions and diseases such as intestinal atresia, short bowel syndrome, neonatal sepsis and necrotising enterocolitis. 7-9,12
DIAGNOSIS
A gastroschisis diagnosis can be achieved in the prenatal stage by means of an ultrasonography, which has high sensitivity and specificity for its detection. Detecting the disease is possible since week 12 19 with rates of up to 90%, depending on the quality of the equipment used, the institution were the examination is performed and the experience of the staff 19-22, which would explain why, in this case, the pathology was not detected prenatally, despite the adequate number of controls and two ultrasound scans taken after week 12.
Prenatal detection of this disease is important because it allows timely genetic counseling, since performing a karyotype is not recommended in these patients given the limited association of this defect with other genetic syndromes. 9 Furthermore, diagnosis facilitates a better monitoring of pregnancy, which avoids complications. 19,23
There are useful ultrasound predictors to estimate the possibility of neonatal complications, such as intestinal atresia. 7,23 Some predictors are intra-abdominal dilation of the bowel 7,8, intrauterine growth restriction 8, thickness of the abdominal wall 8 and liver herniation. 8
MANAGEMENT OF GASTROSCHISIS AT PRIMARY CARE
Once the prenatal diagnosis is made, a multidisciplinary approach (obstetrician, neonatologist, pediatric surgeon) and bi-monthly sonographic controls are required to monitor markers to predict complications. 23 Although some studies postulate that there are no differences in the outcome of neonates in relation to prenatal diagnosis 20, these reports come from developed countries, where care delivery is done in centers of medium or high complexity, while in Colombia undetected cases may be handled in centers that do not have technological resources and adequate personnel, as in this case.
Several studies suggest that early caesarean section (36-37 weeks) decreases morbidity with respect to vaginal delivery due to the supposed risk of infection or perforation of the viscera exposed during the latter, while other authors do not find significant differences. 20,23,24
The scheme presented below should be followed after the birth of a child without a prenatal diagnosis, which is similar to what was presented in this clinical case.
First, adequate resuscitation and oxygen support should be initiated, for which up to 170 mL/kg of dextrose solutions may be required within the first 24 hours, since the metabolic demands of these patients are greater due to the exposure of intestinal loops, with consequent loss of fluids and hypothermia. 23-25 Then, gastric decompression is performed using a probe, washing the intestinal loops with 0.9% saline and covering them with plastic bags or sterile viaflex 23,24, thus reducing the risk of infection. 23-25 The patient is placed in the right lateral decubitus position to reduce the risk of intestinal ischemia 24 and empirical antibiotic management is initiated, preferably with ampicillin-gentamicin, adding vasoactive support if required. These basic measures help to decrease mortality in patients -a study in Africa found that 25% of neonatal deaths with gastroschisis were related to some deficiency in initial management in primary care. 26 Once stabilized, the patient should be referred to a more complex level with Pediatric Surgery and Neonatology Services, maximum 4-7 hours later, since this is the preferred time to perform the surgical closure. 23
There are two types of closures: primary and gradual. Some of the factors associated with the success of primary closure include patients classified as low risk and born intrainstitutionally and in reference centers. 27 On the other hand, gradual closure has some advantages over the primary closure, such as lower incidence of compartment syndrome and intra-abdominal hypertension, lower requirement of mechanical ventilation and vasoactive support. 28 Regarding the surgical technique, in recent years the sutureless closure technique has been implemented using flaps with autologous tissue, mainly umbilical cord. Several studies have found that this technique has an effectiveness profile similar to conventional closure, and that, in fact, in low-risk patients, it is associated with a lower requirement of mechanical ventilation and a decrease in the incidence of surgical wound infections.
In addition, the closing without sutures technique, using flaps with autologous tissue, can be performed outside the operating room, decreasing anesthesia requirements and costs for health institutions. 15,29,30
ETHICAL CONSIDERATIONS
According to bioethical parameters, the efforts during any procedure should be directed to achieve the optimal resolution of the beneficence, nonmaleficence, autonomy, justice and equity principles, which guarantee adequate interdisciplinary management. 31
When analyzing the conflict of principles, the lack of a timely prenatal diagnosis was evident 20, thus preventing adequate follow-up at an appropriate level of complexity and the choice of early cesarean section, which has shown effects on mortality. 23,24 This leads to an initial transgression of the justice and equity principles, since no adequate equipment or human resources were available for prenatal diagnosis in ultrasound after week 12. Regarding the management of this case, it is worth highlighting the optimal initial treatment, timely referral from the primary care institution, adequate information to relatives and the successful interhospital communication, which demonstrate full support to the beneficence and autonomy principles.
This research was authorized by the legal guardian of the minor and respected the confidentiality of the patient and his relatives.
CONCLUSION
Gastroschisis is a congenital defect that, despite its low frequency, requires adequate knowledge not only from specialized personnel, but also from primary care physicians, taking into account that they are obliged to ensure an appropriate and timely referral of the patient to a higher complexity level to avoid complications.