INTRODUCTION
Gallstone ileus (GI) refers to a mechanical obstruction of the gastrointestinal tract caused by impaction of one or more gallstones in the bowel lumen. This condition accounts for 1-4% of all intestinal occlusions in adults. In most cases, obstruction occurs in the terminal ileum (60%), followed by the proximal ileum (25%), and less frequently by the jejunum (9%), the sigmoid colon (4%) and the duodenum (2%). 1
Bouveret syndrome (BS) is a very rare form of gallstone ileus caused by the passage and impaction of a gallstone through a cholecys-toduodenal fistula into the duodenum, which results in gastric outlet obstruction; this condition was first described by Leon Bouveret in 1896. 2,3
Six risk factors are involved in BS presentation: 1) history of cholelithiasis; 2) repeated episodes of cholecystitis; 3) female gender; 4) age >60 years; 5) comorbidity, and 6) gall stones >2.5cm in diameter. 4 This disease usually occurs in elderly women, and in people with an average age of 70-75 years due to the presence of a large gallstone (only one in more than 90% of cases) within the pyloric or duodenal canal. 5
The clinical picture of BS is usually nonspecific, and may present with clinical symptoms of intestinal obstruction characterized by abdominal pain, nausea, vomiting, food intolerance and absence of flatus and stools. 6 The objectives of this work are to report a case of this rare pathology, to comment on its particular characteristics and to present a brief literature review.
CASE PRESENTATION
A 63-year-old male, mestizo patient, who works as a farmer, from the rural area of Milagro-Ecuador, with a history of cholelithiasis 3 years before consultation, visited the emergency service of the Luis Vernaza Hospital due to a clinical picture of 15 days of evolution characterized by moderate epigastric pain that exacerbated after the excessive intake of food. Symptoms included nausea, countless bilious vomiting and malaise.
The patient reported that he had been hospitalized in another institution for about 4 days and had been scheduled for laparoscopic cholecystectomy, but it was cancelled due to the presence of a mass around the gallbladder that involved the liver. Physical examination revealed pale facies, symmetrical thorax (clear and ventilated lung fields), abdominal distension, pain on deep palpation in the upper abdomen, positive Murphy's sign, and increased hydroaeric noises on auscultation. No megalies were observed.
Vital signs on admission were: blood pressure of 120/80 mmHg, temperature of 38°C, oxygen saturation of 98%, pulse of 80 bpm, and respiratory rate of 19 per minute. Blood count test reported leukocytes 19.05 x103/ul; neutrophils 82.3%; 9% lymphocytes; red blood cells 3.78 M/ul; hemoglobin 10.1 g/dl; hematocrit 29.9%; platelets 626 x103/ul; bilirubin: total 0.49 mg/ dl, direct 0.21 mg/dl and indirect 0.28 mg/dl; electrolytes: sodium 147 mEq/L, potassium 3 mEq/L and chlorine 99 mEq/L; gamma glutamyl transferase 120 M/L; alkaline phosphatase 107 U/L; Amylase 102 U/L; lipase 142 U/L, and PCR 47.69 mg/L. After the tests were performed, imaging was requested, revealing the presence of the large gallstone in the second part of the duodenum (Figure 1).
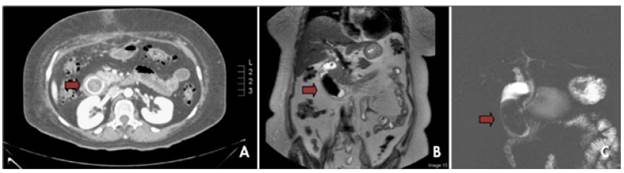
Source: Own elaboration based on the data obtained in the study.
Figure 1 A) Three-phase computed tomography of the abdomen in venous phase; B) and C): T2-weighted SPAIR magnetic resonance cholangiography.
The patient underwent surgery, during which the abdominal cavity was approached by exploratory laparotomy, observing a plastron in the gallbladder topography that involved the greater omentum, the duodenum and the hepatic flexure of the colon. An exploration was made from the angle of Treitz to the duodenum, palpating a 10x5cm stone tumor, which was manually taken to the jejunum at 50cm from the Treitz angle (Figure 2).

Source: Own elaboration based on the data obtained in the study.
Figure 2 Hard mass found in the second part of the duodenum.
Once the stone was taken to the jejunum at 50 cm from the Treitz angle, a longitudinal enterotomy, parallel to the major axis of the stone, was performed (Figure 3A). The stone was extracted (Figure 3B), and suturing was performed transversely with prolene 3/0.
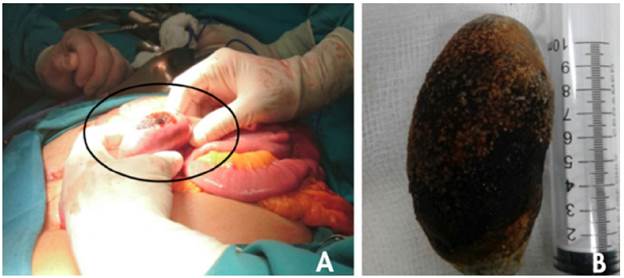
Source: Own elaboration based on the data obtained in the study.
Figure 3 A) Enterotomy parallel to the major axis of the stone (circle); B) Extraction of the biliary stone, with dimensions of 10x5cm.
Within the first two post-operative days, the patient did not present any complications. On the third day, he was able to pass flatus and evacuate the bowel, so he started oral refeeding with clear liquids. On the next day, the patient was able to start a general diet that was satisfactorily tolerated. He did not report any symptoms or fever, so he was discharged on the fifth day. Outpatient postoperative controls were scheduled at 15 days. A second surgery was not considered since there was no evidence of any intestinal obstruction complication that required a new hospitalization.
DISCUSSION
Currently, biliary lithiasis is one of the most common digestive diseases, with prevalence between 10% and 20% in western countries, being more frequent in seniors and women. Although most biliary stones are clinically silent, symptoms or complications appear in 20% of cases. The most frequent location is the gallbladder (85%), but they can be found anywhere in the biliary tract. 7 Cholecystoduodenal fistula and GI are the least frequent complications. 8
The formation of the fistula between the gallbladder and the lumen of the digestive tube may be related to a chronic inflammatory process, which produces less vesicular arterial flow and venous and lymphatic drainage. This situation may cause an increase of the vesicular intraluminal pressure that would favor necrosis and fistulization of the biliodigestive barrier. Cholecystoenteric fistulas occur in 0.3-0.5% of patients with cholelithiasis, and most of them are cholecystudymal (60%), cholecystocolonic (17%), cholecystogastric (5%) and choledochoduodenal (5%). 9
BS is a rare and high risk complication of cholecystitis that affects only 0.9-3.2% of patients with a history of gallstones. 10 Its clinical picture is nonspecific and its most common symptoms are epigastric pain, nausea and vomiting. In the most severe cases, upper gastrointestinal bleeding can occur due to the erosion of the duodenal mucosa as a consequence of gallstone migration. 11 The most frequent complication is electrolyte imbalance. 12
The diagnosis of this disease is delayed because it can be mistaken with other causes of gastroduodenal obstruction. For this reason, differential diagnosis should be made to rule out bezoar, tumors, peptic stenosis and superior mesenteric artery syndrome, among others. 13 An intestinal obstruction occurs when the size of the gallstone is at least 2.5cm in diameter, but, in general, for BS to occur, the dimensions must be larger. 14
Since the symptoms are nonspecific, a high level of clinical suspicion is required to achieve a diagnosis. Complementary exams can be useful; for example, abdomen radiography can show the Rigler triad (aerobilia, dilated small bowel loops with air-fluid levels and ectopic biliary lithiasis), which is pathognomonic of GI, although it is observed in less than 15 % of the cases.
In case of diagnostic doubts, imaging tests can be used, such as upper gastrointestinal endoscopy, which allows direct visualization of the stone causing obstruction in 69% of patients. Also, abdominal ultrasound can reveal gallstones in 75% of BS patients, of which 23% can be visualized in the duodenum, while pneumobilia can be seen in 45%. Computed tomography can find perivesicular inflammatory changes, pneumobilia, cholecistoduodenal fistula, filling defects, level of obstruction and features of the gallbladder. Finally, magnetic resonance cholangiography can be useful to describe fluids and stones. Other echographic signs are contraction of the gallbladder, thinning of the wall of the gallbladder and dilatation of the duodenum. 4,15,16
The ideal treatment of BS is to resolve the digestive obstruction and the biliary disease during the same surgery through gastrotomy or enterotomy, gallstone extraction, cholecystectomy and fistula repair. However, most authors recommend a two-stage treatment, resolving first the obstructive disease and then addressing the biliary condition, if necessary. Considering that patients are usually old, with an important comorbidity and poor general conditions that may lead to an emergency, long surgical times are not recommended, therefore, only gastrotomy or enterotomy and gallstone extraction should be performed. 17
Another treatment option is oral endoscopy after performing endoscopic mechanical lithotripsy and the subsequent oral extraction of the fragments. Regarding lithiasis impact in the terminal ileum, cases of extraction by colonoscopy have been described. 18 Lithiasis size is an important factor to consider, since stones >2.5cm are difficult to extract by endoscopy, so there is also risk of impaction in the esophagus. 5
CONCLUSIONS
BS is a rare case of GI caused by gastric obstruction due to the presence of one or more gallstones in the duodenum secondary to a cholecystoduodenal fistula, which occurs more frequently. This is a late diagnosis disease that requires ancillary techniques such as radiography, ultrasound, abdominal CT, magnetic resonance imaging and upper endoscopy. The ideal treatment is to remove the stone endoscopically, but most authors of the analyzed reviews prefer a two-stage intervention, resolving the intestinal obstruction first and then the fistula.














