INTRODUCTION
Hemangiopericytomas are tumours of vascular origin that are rarely seen in the nose and paranasal sinuses. 1 Histological and biological differences may be observed between sinonasal hemangiopericytoma and its soft tissue counterpart. Its designation as 'hemangiopericytoma-like' tumor implies that it is related to, yet distinct from, soft tissue hemangiopericytomas. 2,3
From a therapeutic point of view, the mainstay of treatment is surgical excision with clear resection margins, as these tumors are relatively radioresistant. Nowadays, given the extraordinary development of endoscopic techniques, sinonasal hemangiopericytoma can be managed endonasally, with very few exceptions. 4
CASE REPORT
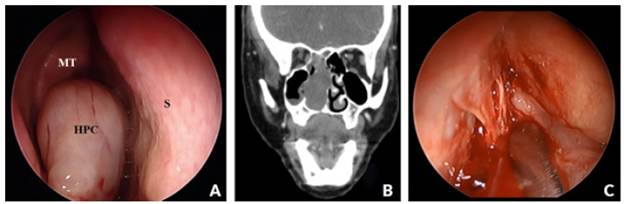
A 43-year old Caucasian female patient, teacher, with no relevant medical history, presented to our hospital with complaints of right nasal obstruction of 6 months of evolution, associated with mucopurulent rhinorrhea and recurrent right side epistaxis. Physical examination showed a right obstructive mass originating from the roof of the nasal fossa (cribriform plate), which caused a deviation of the nasal septum to the left and a lateralization of the middle turbinate to the right (Figure 1A).
Source: Own elaboration based on the data obtained in the study.
Figure 1 (A) Rhinoscopy: Obstructive mass originating from the roof of the right nasal fossa. HPC - Hemangiopericytoma, S -Nasal Septum, MT - Middle Turbinate; (B) CT paranasal sinuses in soft tissue window (coronal); (C) endoscopic surgery.
Computed tomography of the paranasal sinuses (CT-PS) revealed a complete blockage of the right nasal cavity by a homogeneous content, with soft tissue density, without evident contrast enhancement. This neoformation caused bulging with thinning and remodeling of the septum and the wall of the right maxillary sinus. The lesion extended superiorly to the cribriform plate but without intracranial or orbital extension, and posteriorly through the choana to the nasopharynx (Figure 1B). CT scan of the neck and thorax did not identify relevant alterations. A biopsy of the lesion was performed and the histological study revealed an inflammatory polyp with no signs of malignancy.
The patient underwent endoscopic surgery with en bloc resection of the lesion that originated in the cribriform plate of the ethmoid (Figure 1C), without sequelae associated with the procedure.
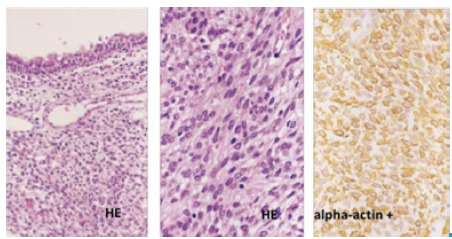
The anatomopathological study of the surgical specimen revealed a tumor with morphological and histochemical characteristics compatible with sinonasal hemangiopericytoma and immunoreactivity to vimentin, CD34 and alpha-actin (Figure 2).
Source: Own elaboration based on the data obtained in the study.
Figure 2 Anatomopathological study: Polyp lined by respiratory epithelium, expanded chorion by proliferation of cells of elongated nuclei, sometimes fusiform in appearance. Immunoreactivity for vimentin, CD34 and alpha-actin. Characteristics suggestive of sinonasal hemangiopericytoma. HE -Hematoxylin-Eosin.
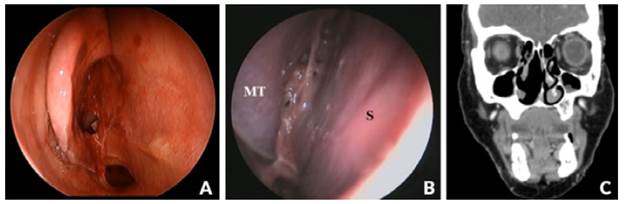
The patient underwent a 3-year follow-up, during which time she remained free of symptoms and showed no signs of local or meta-static recurrence on objective examination and CT-PS imaging (Figure 3).
Source: Own elaboration based on the data obtained in the study.
Figure 3 (A) After removing hemangiopericytoma; (B) Endoscopic examination without evidence of local recurrence (3-year follow-up). MT - Middle Turbinate; S- Nasal Septum; (C) CT paranasal sinuses in soft tissue window (coronal) - 3-year follow-up.
DISCUSSION
Hemangiopericytoma, also known as extrapleural solitary fibrous tumor, is a rare tumor, initially described by Stout and Murray in 1942. Its origin is mesenchymal, originating from capillary pericytes and representing less than 1% of all vascular tumors and only 1 to 2% of soft tissue tumors. 1 It can develop anywhere in the body, being more frequent in the limbs, retroperitone-um and skin. Only 15% of hemangiopericytomas develop in the head and neck region, more frequently in the nasal cavity and para-nasal sinuses. 2 Several etiological factors have been proposed, including hypertension, hormonal or metabolic imbalance and trauma; however, the etiology of sinonasal hemangio-pericytoma is still unknown. 5
Its origin is usually benign but its biological behavior and natural history are still relatively unknown, with a potential risk of malignancy. Sinonasal hemangiopericytoma presents some histological and biological differences with respect to hemangiopericytomas in other places, and is often known as 'hemangiopericytoma-like' sinonasal tumor. Some authors suggest a similarity with glo-mus tumors. 2,3
Sinonasal hemangiopericytoma tends to be immunoreactive with vimentin, α-smooth muscle actin, and muscle specific actin. However, unlike lobular capillary hemangiomas and solitary fibrous tumors, it rarely stains positively for CD34, although staining for CD34 and S100 protein can be focally and weakly positive in a small percentage of tumors. 4,5
These lesions occur mainly between the ages of 40 and 60, affecting both females and males. The most common initial presentation is nasal obstruction and recurrent epistaxis. The lesions are usually painless and the symptoms are originated by their growth and tumor compression. 3
The initial diagnostic assessment must include endoscopic and neuro-radiological evaluation with CT and magnetic resonance imaging (MRI). CT imaging demonstrates tumor involvement of the soft tissue in the nasal cavity and paranasal sinsuses, with bone destruction observed in large tumors. MRI shows sinonasal hemangiopericytoma as a solid mass with isotense signals on contrast-enhanced T1 imaging, which is useful for differentiating it from inflammatory fluid caused by sinus obstruction. 6
Imaging evaluation allows the characterization of tumor extension and its relation with adjacent structures, namely, intracranial and intraorbital components. 5 MRI is superior to CT mainly for the assessment of tumor relation with vascular structures, being important for surgical planning. Chest CT is recommended for assessment of distant metastases that may occur by hematogenic/lymphatic dissemination to the lung. 6 When necessary, additional investigation can be performed through angiography (with preoperative embolization) in larger and strongly vascularized lesions. 7
Biopsy of sinonasal lesions, which are suspected of being vascular tumors, is not routinely performed by our department in the outpatient clinic. Nevertheless, in this case, a biopsy was performed considering that physical examination and CT scan did not present strong evidence of a vascularized lesion. Based on the biopsy results, only sinonasal polyposis was suspected initially, therefore, no preoperative magnetic resonance imaging was performed. Although this is a limitation, it had no influence on the procedure and surgical outcome, since complete resection of the lesion was achieved without associated complications and without recurrence after 3 years of follow-up.
Sinonasal hemangiopericytoma is a benign lesion with a low risk of malignancy (<10%). Malignant lesions have an increased risk of recurrence and are associated with cellular pleomorphism, moderate to severe nuclear atypia, bone invasion, and tumor necrosis. Some authors state that the presentation of hemangiopericytoma at the sinonasal level is less aggressive but locally recurrent. 6,8. The treatment of choice is endoscopic surgical resection with free margins, with positive margins being the main positive predictive factor for recurrence of hemangiopericytoma. High recurrence rates are probably associated with the difficulty of total excision of the tumor at this location. 9
Adjuvant radiotherapy is a second-line treatment, indicated for lesions with malignant characteristics and incomplete surgical re-section/unresectable tumors. The use of chemotherapy is controversial and its efficacy has not been proven. Prognosis is usually good if complete surgical excision of the primary tumor is achieved, with a 5-year survival rate of 89-100%. 1 However, long-term follow-up is necessary given the potential risk of malignancy and tumor recurrence. 4
With less than 200 cases of sinonasal hemangiopericytomas reported in the literature, only limited assumptions can be made about the tumor. 10,11 This is another case of sinonasal hemangiopericytoma to add to the small but growing body of literature on this disease. Historically, open surgical methods for tumor extirpation have been considered as standard treatment, although endoscopic resection has increased in recent decades. 12,13 This clinical case demonstrates that endoscopic resection is a safe, viable and reasonable alternative and is currently the gold standard of treatment.
CONCLUSION
Hemangiopericytoma is a rare tumor in the sinonasal region with usually benign etiology. Adequate surgery with free resection margins is the treatment of choice. Nowadays, with very few exceptions, resection should be conducted endoscopically. Patient outcome is generally good, and the risk of recurrence seems to be related to complete resection.














