INTRODUCTION
Cystic lesions of the neck are rare and difficult to interpret for clinicians, since they can be benign or malignant pathologies. The most common location is the posterior triangle, where inflammatory, metastatic adenopathies or lymphoproliferative diseases can occur. In addition, congenital malformations such as branchial cysts, hemangiomas and lymphangiomas may be observed in this area. 1 Branchial cleft cysts and hemangiomas are easily diagnosed in children under 2 years of age due to their clinical characteristics. These lesions are observed as a mass that usually does not involve inflammatory changes and presents a slow and painless growth or lymphangiomas, which are rare after the third decade of life. 2-5
The current trend to treat lymphangiomas is different; conservative interventions such as sclerotherapy, now performed with new substances, have relegated surgery to the background due to the high rate of relapse or persistence. 4,5 Considering that lymphangiomas are rare in adults 4 and that the patient treated was a 36-year-old woman who underwent a complete surgical resection, a review of the subject is presented with a description of the different treatment options.
CASE PRESENTATION
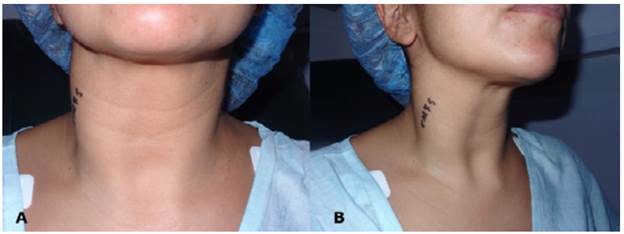
A 36 year-old female patient, Caucasian, from the city, consulted due to a right lateral mass in the neck of 20 days of evolution without associated systemic symptoms, dysphonia, dysphagia or pain. No personal or family history of importance in relation to the current disease and no history of neck trauma or infection of the head and neck area were described. On physical examination, a right lateral soft mass of 6cm was found, which was tender on palpation and with displacement and lateralization of the sternocleidomastoid muscle (Figure 1).
Source: Own elaboration based on the data obtained in the study.
Figure 1 Deformity of the right contour of the neck. A) Anterior aspect of the neck; B) Lateral aspect of the neck.
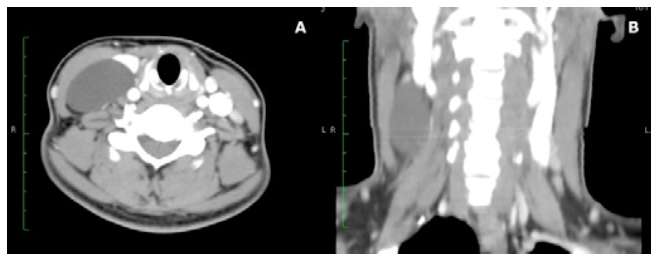
A contrast study of the neck using computed tomography (CT) showed a cystic lesion with thin walls of 55x21x43mm, which compressed the internal jugular vein, occupied the right III and IV levels and was clearly delimited by vascular and muscular structures (Figure 2).
Source: Own elaboration based on the data obtained in the study.
Figure 2 Contrast computed tomography of the neck. A) Thin-walled cyst medial to the sternocleidomastoid muscle; B) Cystic lesion occupying the right III and IV levels.
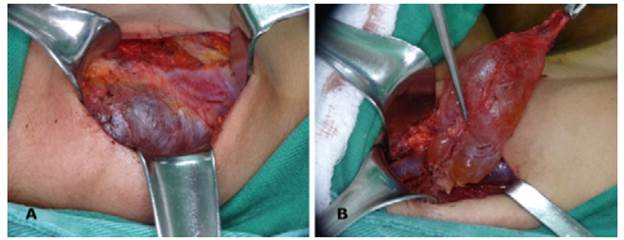
Fine needle aspiration (FNA) helped to diagnose cyst content with lymphoid tissue lining, which could be lymphocele or lymphangioma (cystic hygroma). Due to the lack of diagnostic clarity, a surgery was performed 15 days later. During the procedure, a medial cystic mass was found in the sternocleidomastoid muscle adhered to the internal jugular vein and to the phrenic, hypoglossal, spinal and vagus nerves. Finally, the lesion was completely resected along with the entire capsule (Figure 3).
Source: Own elaboration based on the data obtained in the study.
Figure 3 Intraoperative appearance. A) Transverse incision of the neck. A deep lesion of the sternocleidomastoid muscle was observed along with junctions to the internal jugular vein and accessory nerve. B) Lymphangioma was dissected from the internal jugular vein.
Source: Own elaboration based on the data obtained in the study.
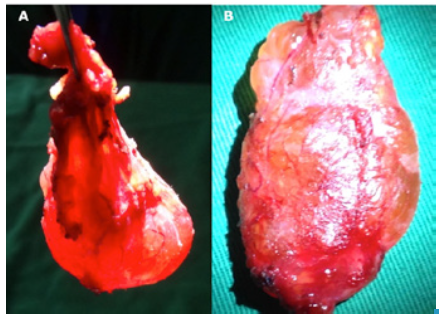
Figure 4 Surgical specimen: transillumination revealed a thin-walled cyst.
Transillumination of the surgical specimen revealed a thin-walled, cystic-like mass with citrine material content, which correlated with the diagnosis of preoperative FNA (Figure 4).
The final pathology reported a cystic mass of 6.9x3.2x3cm, with smooth external surface and a clear liquid content. Additionally, the smooth inner surface was accompanied by an adipose tissue of 2.5x1.8x1cm with another tissue of 1.5x0.6x0.5cm. The final diagnosis of the pathology was lymphangioma and five reactive lymph nodes, negative for tumor infiltration. The patient did not present any complication during the postoperative period, nor motor deficit related to the dissected structures, nor evidence of relapse or persistence of the lesion after 12 months of follow-up. No complaints were made by the patient, who reported excellent functional and cosmetic results.
DISCUSSION
Lymphangiomas, also known as cystic hygromas, are congenital malformations that are usually diagnosed at birth and can cause airway obstruction, thus constituting a medical emergency. 6 These lesions are considered vascular anomalies of the lymphatic system and are classified as hamartomas based on pathology findings. 7 Different etiological and pathogenic factors have been described as causal, including traumatic, infectious and chronic inflammatory factors, as well as alterations in embryological development. The latter includes sequestration of lymphatic tissue, defects in the fusion of the venous system, and lymphatic obstruction that causes its expansion and obstruction. 8 In adults, late proliferation of cellular nests of the lymphatic system may appear due to stimulation caused by trauma or infection. 9,10
Lymphangiomas correspond to 25% of all vascular tumors in children and adolescents; 70% of cases are found in the head and the neck. In 2006, Thompson 11 proposed classifying them into cystic (cystic hygroma), capillary or cavernous, but there are different histological classifications:
Colbert et al.12 classified them into macrocysts, formerly known as cystic hygromas, and in microcysts, which may occur simultaneously in a lesion.
Bhayya et al.13 classified them in lymphangioma simplex, composed of small thin-walled lymphatics; cavernous lymphangioma, comprised of dilated lymphatic vessels with surrounding adventitia, cystic lymphangioma, consisting of a large lesion, with macroscopic lymphatic spaces surrounded by fibrovascular tissue and smooth muscle, and benign lymphangioendothelioma, lymphatic channels that seem to be dissected through dense collagen bundles.
In 1995, de Serres et al.14 proposed a classification according to anatomical location: Stage I, unilateral infrahyoid lesion; Stage II, unilateral suprahyoid lesion; Stage III, unilateral suprahyoid and infrahyoid lesion; Stage IV, bilateral suprahyoid lesion, and Stage V, bilateral suprahyoid and infrahyoid lesion.
Based on the last classification system, the case presented here corresponds to stage I (right lateral extension from a horizontal plane to the hyoid bone and to the superior clavicular ridge). This made dissection and complete resection easier, without evidence of residual tissue on the surgical bed.
The diagnostic studies used to determine cystic tumors of the neck include high resolution ultrasound, which can prove the presence of a cystic lesion with multiple septa and without internal vascular flow that allows differentiating them from mixed vascular lesions. However, CT and magnetic resonance imaging (MRI) determine more precisely the relationship of the mass with the adjacent structures. The T1 and T2 sequences of the MRI facilitate the visualization of cleavage planes with the muscles and can define whether it is a vascular malformation. 12
Fageeh et al.15 proposed observation, percutaneous drainage, carbon dioxide laser (CO2) and Nd-YAG laser, diathermy and surgical resection as management options. Recently, Miceli & Stewart 16 recommended sclerotherapy with doxycycline or radiotherapy as treatment options. Observation may be indicated for patients younger than 3 years who do not have obstruction of the airway and have lesions <4cm, since they could present spontaneous regression. 15,17
Surgical resection has traditionally been advocated as the best treatment option, but in cases where the lesions extend into deep neck spaces, as the floor of the mouth or parapharyngeal space, complete removal may be difficult to achieve without damaging the nervous and vascular structures. This situation has led to seek alternatives such as drainage and sclerotherapy with different substances such as tetracycline, bleomycin and triamcinolone. Radiofrequency ablation is another therapeutic option to treat this entity. 12 Complications and associated morbidity can include infections, tissue necrosis, cranial nerve lesions, vascular thrombosis and even endocrine disorders. 6,15
Ogita et al.18 described the use of a streptococcal preparation OK-432 (Picibanil) as a safe alternative to perform sclerosis in cystic lesions of the neck, considering that this substance produces fibrosis secondary to inflammatory and cicatricial changes with the consequent contraction of the lymphangioma. 18 OK-432 is a lyophilisate made of group A Streptococcus pyogenes incubated with penicillin, which is initially used as immunotherapy for cancer in cases of pleural and peritoneal carcinomatosis. 19
These authors used this preparation in 83 patients with benign cystic lesions of the neck; 12 of them had lymphangiomas, achieving complete reduction in 67% and almost complete in 33% of the cases. Only some patients developed minor complications such as fever between 37.5°C and 38°C for a few days after the injection, which was controlled with antipyretics and without antibiotics. 19
Unilateral lesions composed of microcysts, delimited and extended to one or two compartments of the neck, are candidates for surgical resection, as they may be completely resected. However, the lesions located near the floor of the mouth or the parapharyngeal space are more likely to be partially resected. 6 In this patient, with no family history or genetic alterations, the lymphangioma was secondary to interruption of lymphatic drainage, probably due to previous neck trauma that went unnoticed. Similar to Gow et al.6, for this case, surgical resection of the mass was decided because the CT showed a single cyst circumscribed to the III and IV right levels of the neck (Figure 2).
Although, it extended to level III, IV and Vb, it was possible to remove the mass without breaking the cysts (Figure 3). Macroscopic examination showed that the lesion had a clear content that allowed transillumination, confirming a lymphangioma (Figure 4).
CONCLUSIONS
Radiological images such as neck CT, MRI and neck ultrasound with FNA are of great help for diagnosing and planning the management of lymphangiomas of the neck.
Clinical suspicion of lymphangioma helps to establish the treatment for a patient with soft mass and radiological images suggestive of neck cysts. However, the definitive diagnosis is only obtained with the final pathology.
In adult patients, conservative observation treatment or sclerotherapy with different preparations such as picibanil are management options, especially when dealing with a complex lesion extended to the parapharyngeal space, submandibular space, pterygoid fossa or floor of the mouth.
Surgery is recommended for patients with lymphangioma simplex stage I, with single or multiple cysts that extent to one or two levels of the neck, and radiological planes well defined by images.














