INTRODUCTION
Trauma to the orbital region involving an intraorbital foreign body injury in children under five years of age is usually generated by casual play, being more frequent in males. 1 The symptoms associated with this disorder are varied and depend on the extent of the injury, the composition of the foreign body, its trajectory, the speed of the impact against the orbit, among other factors. 2
The first step to take is the stabilization of the patient to be able to perform a complete ophthalmological examination. It is worth noting that not all periorbital foreign bodies should be removed; therefore, the procedure will depend on the characteristics of the material and its location. 3 Computed tomography (CT) of the orbit and skull is an important tool for identifying the severity of the injuries and making therapeutic decisions.
Foreign bodies usually penetrate the orbit and slide between the orbital wall and the eyeball, without affecting the latter; they rarely cross the orbit to penetrate the paranasal sinuses or the intracranial space, possibly involving neurovascular elements. 2,4,5 This paper presents the case of a foreign body that passed through the orbit and penetrated the skull, reaching the temporal lobe without affecting the eyeball.
CASE PRESENTATION
This is the case of a five-year-old girl, mestizo, student, from Bogotá D.C., of a middle-income household.
The patient was admitted to the pediatric emergency department of the Clínica Universitaria Colombia in Bogotá D.C. due to a clinical picture of an hour of evolution of left penetrating intraorbital injury caused by a lodged foreign body. This occurred after an accident during arts class, where a paint brush penetrated the orbit causing a visible injury without eye pain or loss of visual acuity associated with two emetic episodes; the patient's mother denied bleeding and other associated symptoms. Healthy patient with no relevant history. The student did not receive any treatment at school or from her relatives; prehospital staff monitored her and transferred her to the hospital for assessment.
On physical examination, the patient was conscious, with stable vital signs and left eye with foreign body (brush) in ocular orbit, with eyelid hematoma that did not allow her to open the eye, and without apparent eye involvement or hemorrhage. The paint brush was partially visible inside the eyeball and an approximate surface of 14cm protruded to the outside; the initial ophthalmic exam revealed lateral deviation of the upper rectus muscle. Considering the findings, she was transferred to the pediatric resuscitation room and coagulation times, complete blood count and renal function tests were requested, which yielded normal results. A simple CT scan of the skull study was indicated.
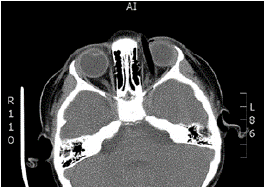
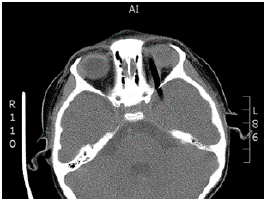
The tomography showed an intraorbital route of the foreign body towards the right side, and above the left eyeball towards the temporal lobe; no intraconal or intraocular lesions were evident, and no intracranial, subdural or epidural hematomas or retroconal bleeding were observed (Figures 1 and 2).
The diagnostic images were evaluated by neurosurgery, which considered removing bone splinters. The operative report of this procedure described the presence of a foreign body above the left eyeball; the foreign body was completely removed by traction.
After the removal, a control CT of the skull and orbits was performed, reporting left eyelid hematoma and in the left upper rectus and lateral rectus muscles. A frontal subdural and temporal left laminar hematoma was observed in the cranial cavity, without compressive effects.
The patient was treated along with the ophthalmology service in the pediatric critical care unit (CCU) without initial evidence of neurological or ophthalmic injury. On physical examination, ophthalmology found mild pro-ptosis, hematoma of the upper eyelid limiting ocular opening, clear cornea, formed anterior chamber, healthy iris, 3mm pupil, photopupillary reflexes and preserved ocular movements.
In the CCU, the child received antibiotic synergy with vancomycin 220mg every 6 hours intravenously, later increased to 250mg every 6 hours, and ceftriaxone 1g every 12 hours intravenously; anti-inflammatory management with intravenous dexamethasone and mechanical ventilation was indicated. The control CT scan of the orbit taken the first post-operative day showed a decrease in the upper subperiosteal hematoma and hematoma adjacent to the lateral rectus muscle; this retroconal hematoma had orbital extension and persisted on site in the three thirds of the orbit, greater in the anterior third and without signs of optic nerve compression or other alterations of intraorbital structures. In addition, control CT scan of the skull showed subarachnoid hemorrhage over the tentorium of the left cerebellum and falx cerebri, as well as acute frontal basal left and temporal left subdural hemorrhage with an extension of 5mm.
On the second day of stay in the CCU, the patient was extubated and an ophthalmology assessment was performed again, reporting a reduction of eyelid edema, clear cornea with a healthy anterior chamber, normal near and distant visual acuity in both eyes, left subconjunctival hemorrhages resolution and left intraocular pressure of 14/15 mmHg. Moreover, dilated fundus examination was made using drops of benoxinate hydrochloride and 0.5% tropicamide with 5% phenylephrine hydrochloride; after pharmacological dilation, disc with excavation of 0.3/0.3, normal retinal vessels and healthy macula were reported for both eyes.
Taking into account the satisfactory evolution the following day, the patient was sent to the pediatric floor, where she evolved satisfactorily without neurological or visual impairment, nor need for new surgical interventions. The last control CT scan of the orbit revealed slight reduction of retroconal hematoma, persistence of left frontal and temporal subdural collection and slight subfalcine hernia of 3mm, without evidence of transtentorial hernia, expansive lesions, cysts or calcifications.
The girl completed a five-day antibiotic and anti-inflammatory scheme, with favorable evolution and no adverse events or reactions to the established treatment; in consequence, she was discharged with control by external consultation with pediatrics, ophthalmology and neuropediatrics. No topical ophthalmic management was indicated during hospitalization. During the control consultations, the patient remained asymptomatic and had an adequate recovery.
It should be noted that considering the trajectory of the penetrating object and its intraorbital accommodation prior to splinterectomy was highly relevant; this case was characterized by the integrity of the central artery and vein of the retina and the optic nerve as the foreign body was at the extraconal space without intraocular involvement. The neurological evolution was satisfactory with a retroconal hemorrhage that was adequately reabsorbed and small laminar subdural hematomas, which demonstrates the importance of timely and interdisciplinary management to reduce the risk of complications in the eyes (cellulite, restrictive or paralytic strabismus, etc.) and the brain (skull base osteomyelitis, brain abscess, etc.)
The differential diagnosis depends on the kinetics of the trauma, the accommodation of the foreign body and, mainly, the findings by orbit and skull imaging. Diagnostic difficulty increases when the foreign body is metallic or has irregular contours, generating artifacts and difficult radiological reading.
For the analysis of the reported case, a non-systematic search of the literature was performed in the databases PubMed, Embase, ClinicalKey and Scopus and in Google Scholar using the keywords "trauma orbitario penetrante" and "cuerpo extraño intraorbitario" and their English equivalents "penetrating eye injuries" and "eye foreign bodies". The information retrieved was filtered by title match and date of publication over the last 10 years (2008-2018). The report and case analysis were presented to the Research Ethics Committee of Fundación Universitaria Sanitas for approval.
DISCUSSION
Eye trauma during childhood is usually caused by bruising or penetrating mechanisms, resulting from games or sports (59%) and accidental bumps or falls (37%). These traumas can cause damage to varying degrees and can involve the patient's vision. This is the main cause of monocular blindness in the pediatric population, and requires immediate care. 6,7
Although ocular trauma by intraorbital foreign body is rare in the pediatric population, it is an emergency when it occurs. From a physio-pathological perspective, there is an increase in orbital pressure and, therefore, in its structures. The clinic includes diplopia, strabismus, pain upon eye movement, nausea and vomiting, which were not observed in the reported case. 1 Action in the emergency department must be precise and accurate, involving pediatrics, ophthalmology and neurosurgery. The diagnostic support of the CT scan is relevant to establish the location of the intraorbital lesion (intraconal, extraconal or intraocular) and the therapeutic plan to follow. 2,3,5
In general, small or sharp objects traveling at high speeds can cause serious injury to different components of the orbit. Flying elements from a pruner, emery or any tool, lances, pencils and missiles can strike the eyes and pierce the eyeball 2,3, causing corneal lesions, hyphema (bleeding between the iris and the cornea), damage to the iris (causing a change in pupil size and shape), uveitis, cataracts, hemovitreous, retinal detachment, endophthalmitis, among others. 2 Their trajectories may also involve intraorbital structures outside the eyeball, such as the optic nerve, the vascular bundle of the retina, and the external muscles of the eye.
The main treatment in patients with intraorbital foreign body trauma is removal of the foreign body, given the risk of involvement of the eyeball and possible complications such as secondary infections, severe orbital inflammation, osteomyelitis and even brain abscess. 8 However, taking into account whether the foreign body is organic or inorganic, it is necessary to assess if it generates clinical manifestations or not, since its extraction can cause complications during surgical exploration because organic objects are associated mostly with inflammatory responses and subsequent abscesses. 8,9
When inorganic foreign bodies are present, the possibility of expectant management should not be ruled out, as long as it does not generate functional involvement in the patient. 9 The type of diagnostic imaging to be used is established depending on its composition, being CT scan of the orbit the one of choice. Magnetic resonance imaging (MRI) of the orbit may be considered as an imaging modality as long the foreign body does not have any metallic component. 10,12 Alternatively, and according to availability, ocular ultrasound can be used, which is especially useful to identify possible associated intraocular damage. 11-14
The treatment plan for intraocular injury varies depending on whether the optic nerve or the neurovascular bundle of the retina are involved and the severity. Thus, repair surgery and medications that generate immediate action at the site of the condition can be provided; in these cases, the use of systemic steroids and decompressive surgery should be considered. 15 The evolution of vision will depend on the response to the treatment and may lead to monocular blindness, in addition to being associated with an increased risk of intracranial injury. 15,16
Different factors 16,17 such as the material and trajectory of the foreign body and, especially, the location and extent of the involvement of the intraorbital lesion must be taken into account when starting the treatment: intraocular, intraconal or extraconal. 12,13
CONCLUSIONS
Foreign body trauma to the eye is relatively rare, with varying incidence rates of approximately 13.2 cases per 100 000 inhabitants of all ages and described in 27.3 cases per 100 000 inhabitants in the United States. 18 When it occurs in children under five years of age, games and sports are precipitating factors, with a slight preponderance in the male sex and an increased risk of monocular blindness 19, of which no exact incidence has been reported.
Associated clinical manifestations, such as diplopia, strabismus, pain upon eye movement, nausea and vomiting, are related to the extent of the injury, the involvement of the transparent tissue and retina, composition, trajectory and velocity of the impact of the foreign body within the orbit. 20 Therefore, diagnostic and therapeutic interventions from the ophthalmology service are essential to ensure the preservation of vision.
CT scan of the skull and orbit is useful to focus management, which in turn requires a multidisciplinary team of professionals properly coordinated. 21 This case was characterized by an intraorbital trajectory of the penetrating object and interdisciplinary management (pediatrics, pediatric neurology, ophthalmology, neurosurgery and neuroradiology) that allowed preserving the patient's vision and extraocular movements, thus avoiding severe ophthalmic and neurological sequelae and evidencing that the adequate and timely treatment of this pathology decreases the risk of complications.