INTRODUCTION
Ameloblastoma is a rare benign intraosseous neoplasm that originates in the odontogenic epithelium. It is of unknown etiology and is characterized by expansive growth with a tendency to recurrence. 1 This pathology represents 10% of maxillary and mandibular tumors, with equal affectation by sex, with average age of onset at 35 years. 2 80% of ameloblastomas originate in the jaw and most often affect the posterior region, followed by the anterior region. The maxilla is the second most common site of presentation, while the involvement of the sinuses and nasal cavity is rare. 3
The clinical picture of this pathology is characterized by a mass of slow growth that is not painful at the beginning, but complications such as dental loss, dental malocclusion, paresthesia, pain, soft tissue invasion, facial deformity, limitation of mouth opening, difficulty chewing and airway obstruction can be observed as size increases. 1 Diagnosis requires imaging studies, such as panoramic radiography and computed tomography (CT), as well as biopsy of the lesion for histopathological studies. 2
Ameloblastoma rarely evolves into malignancy and develops hematogenous spread 3; although the benign histology of ameloblastoma is the same, the malignant histology is characterized by the presence of metastases and is associated with cytologic atypia with or without metastases. 3
The current treatment is wide local excision, which should include adequate resection margins. Radiation and chemotherapy are reserved for palliative purposes only.
CASE PRESENTATION
Male patient of 39 years of age, mestizo, from Zapatoca (Santander, Colombia), high school graduate, freelance trader, non-smoker, with no relevant medical history nor previous ameloblastomas or neoplastic diseases. The subject had a history of 11 years of evolution, which began with the appearance of a mass of progressive growth in the left mandibular region, associated with pain in the mandibular and dental areas with left irradiation to the mastoid. The physical examination revealed an alteration of the facial contour due to the presence of a mass of about 7cm of anteroposterior diameter occupying the maxillary sinus and the left mandibular region.
A contrasted CT scan of the neck and paranasal sinuses was performed, identifying a mass involving the left mandibular region and the pterigopalatine fossa with associated bone destruction; a biopsy with histopathological study report was also performed, showing follicular and plexiform ameloblastoma. Taking into account the findings of the tomography and the reports from the pathologist, ameloblastoma was diagnosed without a doubt. Extension studies were also performed with chest CT and cervical lymph node puncture biopsy, ruling out distant disease. The case was discussed during a multidisciplinary meeting where a left partial mandibulectomy, mandibular condyle reconstruction with plaque and fibula free flap were established as management. The pathology of the surgical specimen showed tumor-free edges and surgical margins of 10mm (Figure 1).
Source: Document obtained during the study.
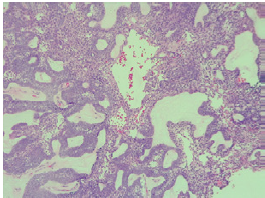
Figure 1 Histopathology of mandibulectomy with evidence of follicular ameloblastoma and odontogenic epithelial islands with peripheral columnar cells.
The patient underwent medical check-ups and contrasted sinus and chest CT every six months during the first year and then every year. After three years of follow-up, in an outpatient control consultation, the patient was found in good general condition, with adequate Weber-Fergusson's approach facial scar, left peripheral facial palsy, adequate mouth opening, island flap of the skin with vital and integrated fibula, left hemifacial induration of soft tissues and scalp lesion in left temporal region that extended to the parietal region with anteroposterior diameter of 7cm, without further pathological findings.
Biopsy was performed on the lesion of the scalp revealing ameloblastoma metastases; the subject was taken to surgery with wide local excision and free flap reconstruction. Surgical specimen pathology confirmed metastatic ameloblastoma and reported tumor-free section borders with margins of 14mm (Figure 2).
Source: Document obtained during the study.
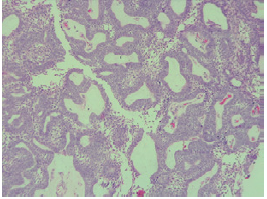
Figure 2 Histopathology study of resection of scalp metastases, follicular ameloblastoma without changes in the cell type of the primary tumor.
The patient assisted to annual medical check-ups with contrasted CT scans; in the sixth year of follow-up, local relapse was observed, so he was taken to partial resection of the left maxilla with extension to infratemporal fossa and reconstruction with anterolateral thigh free flap. The pathology of the surgical specimen confirmed ameloblastoma and reported tumor free section borders with margins of 9mm.
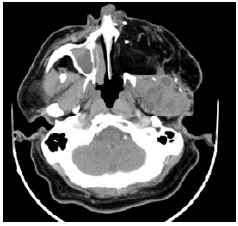
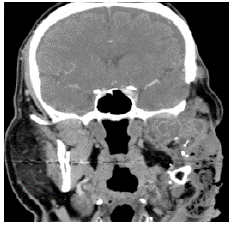
Eleven years after the initial surgery, and after 3 surgeries, a new local relapse was discovered. On physical examination, the patient was found in good condition, with left facial palsy and mass in left masticator space with extension to hard and soft palate, in addition to left submandibular ganglion conglomerate. Contrasted CT showed a mass that involved the left masticator space, lobed, of heterogeneous density with extension towards the skull and average cranial fossa of 36.7x53.6x42mm in anteroposterior section (Figures 3 and 4); biopsy and histopathological study confirmed ameloblastoma.
Source: Document obtained during the study.
Figure 3 Computed tomography of paranasal sinuses with evidence of heterogeneous and hypotensive mass in the left masticator space of lobed contours with dimensions of 36.7x53.6x42.7mm.
Source: Document obtained during the study.
Figure 4 Computed tomography of paranasal sinuses showing heterogeneous mass in left masticator space with extension to the base of the skull and middle cranial fossa.
The patient was assessed by a multidisciplinary team, which concluded that it was not possible to perform new surgical interventions due to the extent of the disease; instead, palliative management with intensity-modulated radiation therapy (IMRT) was ordered. After simulation, planning and delimitation of the area to irradiate, a total of 66 Gray (Gy) in fractionation of 2 Gy was indicated, for a total of 33 sessions during 44 days. During session 12, the patient presented an episode of mucositis treated with a master formula for topical use with appropriate resolution, allowing the radiotherapy to continue without suspending it.
Two months after completing the radiotherapy sessions, the patient was in good general condition but reported xerostomy; the physical examination showed clinical decrease of the mass in the masticator space and palate with changes in the left hemifacial and cervical skin secondary to radiodermatitis. There were no clinical signs of lesion progression.
Follicular cystic ameloblastoma and plexi-form ameloblastoma were identified in all the pathologies analyzed since the initial biopsy and in the different surgical specimens (Figures 3 and 4), both from the local resections and the scalp lesion. No genetic profile of BRAFV600E mutation was performed, since it was not requested during the period when the samples were processed and it is not a routine test performed in the institution.
Although the surgeries performed were useful to completely resect the tumor with negative and proper surgical margins and without failures in the surgical technique or in the choice of the surgical approach, the ability of ameloblastoma to recur was demonstrated.
DISCUSSION
Ameloblastoma is a benign but aggressive intraosseous odontogenic neoplasm with progressive growth, large local expansion, bone destruction, dental resorption and a high tendency to recurrence. 1-3 Although rare, with an annual incidence in the general population of 0.5 cases per 1 000 000 inhabitants, ameloblastoma is the most common odontogenic tumor, excluding odontomas. 4,5 Peak incidence is between the fourth and the fifth decade of life, with an age range of 8 to 92 years and no sex predilection. 4,6,7 For cases associated with BRAFV600E mutation, the mean age of diagnosis is 34, with a more aggressive presentation. 8 80% of all ameloblastomas are found in the mandible, most frequently in the posterior region, followed by the anterior portion of the mandible, the posterior maxillary segment and the anterior maxillary segment 4,6,9-11 as observed in this case, where the entire left mandible was involved with extension to the ipsilateral pterygopalatin fossa, associated with bone destruction.
Ameloblastoma presents as a slow-growing, expansive lesion, which may exhibit late, accelerated growth. 12 As size increases, it is associated with complications such as dental loss, dental malocclusion, paresthesia, pain, invasion of soft tissues, facial deformity, limitation of mouth opening, difficulty chewing and airway obstruction.
Radiologically speaking, it is common to find a multilocular radiolucent image of soap bubble or honeycomb appearance in the cortex, buccal and lingual expansion, and resorption of the involved dental roots. 13,14
The diagnosis of ameloblastoma is achieved based on physical examination, including examination of the head and neck and imaging studies, which in turn include panoramic radiography, contrasted computed tomography and biopsy of the lesion.
The pathological types of this disease can be varied: solid, multicystic, unicystic, desmoplastic and peripheral ameloblastoma. 15,16 Solid and multicystic ameloblastomas have been identified as the most aggressive subtype, with a high rate of recurrence after local excision. 17 The most common histological type is the follicular, followed by the plexiform; other histological types are the acanthomatous, granular and basaloid. 1 The case presented here had a histopathological diagnosis of follicular and plexiform ameloblastoma, which is the most frequently reported. 1
Since 2015, the World Health Organization classification system made a clear distinction between ameloblastoma, malignant ameloblastoma and ameloblastic carcinoma. 1 Malignant ameloblastoma differs from ameloblastoma in the presence of distant metastases, although both have the same benign histology. A metastatic malignant ameloblastoma tumor, by definition, should have the same histological characteristics as a primary mandibular tumor. 18
The histopathological comparison between the different surgical specimens of the reported case, which had the same characteristics between samples, was fundamental for the diagnosis of malignant ameloblastoma. Ameloblastic carcinoma combines some characteristics of ameloblastoma and cytological atypia with or without metastases. 18
Most ameloblastomas have predominantly follicular and acanthomatous patterns and are rarely mistaken for other lesions if adequate tissue is provided for histopathological examination. Desmoplastic ameloblastoma may cause some initial confusion, but knowing about this unusual and particular pattern that occurs in a jaw tumor should not cause diagnostic difficulties as long as adequate material is available for the pathologist to study. 19
Since there is a time gap between the diagnosis of the primary tumor and the occurrence of metastasis, whether regional or distant (10 to 12 years on average), at least one chest x-ray per year is recommended for follow-up because it is the most frequent site of distant metastasis, in addition to clinical progression and imaging studies of the neck and primary site of surgical resection. 20
In the US, the annual incidence of malignant ameloblastoma and ameloblastic carcinoma is 1.79 cases per 10 000 000 inhabitants. 1 In a literature review conducted by the Mayo Clinic of publications made between 1923 and 2009, only 101 possible cases of metastatic ameloblastoma were identified. 21 According to Houston et al. 22, most reported cases of metastatic ameloblastoma suggest hematogenous or lymphatic spread. Another mechanism of metastasis described by Vorzimer & Perla 23 is the aspiration of tumor cells from the primary lesion during surgery, which may contribute to pulmonary, lymphatic, or hematogenous spread. The most common site of ameloblastoma metastasis is the lung (72.7%), followed by cervical lymph nodes, brain, and bone. 23 The scalp is a rare site of metastasis of malignant ameloblastoma: only one case has been reported in the literature. 24
The primary and optimal treatment for ameloblastoma is surgery, in other words, total excision of the lesion with radical resections and margins of 1.5cm to 2.0cm. 25 The surgical options for tumors in the jaw are hemimandibulectomy, segmental mandibulectomy or mandibulectomy; for very small, well-defined lesions that can be resected through the oral cavity, marginal mandibulectomy is indicated, but curettage of the lesion is not useful because lesions always recur; for lesions in the upper jaw, depending on the area involved and the extent of the tumor, infrastructure, medial, partial, subtotal or total maxillectomy are indicated 26; cystic ameloblastomas, which have less aggressive biological behavior and less recurrence compared to multilocular ameloblastomas, can be treated by decompression and subsequent enucleation of the lesion. 27
Treatment of metastatic lesions is not yet uniform, as sometimes surgical resection is not possible due to their anatomical location or extension; furthermore, no clear chemotherapy or radiotherapy protocols have been established for these lesions. 28 So far, surgical treatment is the only one option that increases disease-free survival.
The effectiveness of adjuvant treatment is not clear because few cases have been described. The case reported by Jain et al. 29 showed partial response of an ameloblastoma with pulmonary metastases treated with pazopanib.
In the multivariate analysis of Yang et al. 30, in 87 cases of recurrent craniofacial ameloblastoma, the associated risk factors for recurrence and ameloblastic carcinoma were evaluated. The conclusion was that the most important factors are size and stage of the tumor: stage I, maximum tumor diameter <6cm; stage II, maximum tumor diameter >6cm or tumor invading the maxillary sinus, orbital floor or soft tissues; and stage III, tumor invading the base of the skull or metastatic tumor in the cervical lymph nodes. Tumors >6cm and involving soft tissues and adjacent anatomical structures are associated with early recurrences, regardless of the surgical treatment. 30
Freignani et al. 31 examined the clinical, pathological and histological findings of 121 patients treated in a single institution and diagnosed with ameloblastoma from 1953 to 2003. The study aimed to establish predictors of recurrence, and the results suggested that the presence of a multilocular lesion with rupture of the basal cortical bone and a histological follicular tumor have poor prognosis.
The case reported here allows approaching a pathology that, although rare, has great impact on the health state of the patients who have it due to its tendency to local recurrence and distant involvement, making ameloblastoma a complex entity. For this reason, a clear, accurate and timely diagnosis of ameloblastoma, paying utmost attention to its histopathological characteristics and complete radical surgical resection with oncological resection margins, is considered as the best option for adequate survival in patients presenting with this rare entity. Curettage of the lesion only or multiple resections due to recurrence increase the risk of metastasis.
Surgery is the best alternative for the treatment of metastases; even though chemotherapy and radiotherapy have also been described, they have been recommended for palliative management. For lesions that cannot be treated surgically, radiotherapy and chemotherapy are the only options currently available; however, the recurrence rate with these techniques is high.
Here, in consequence, the treatment currently available for ameloblastoma was used, which consists of extensive surgical resection of the initial tumor, as well as of recurrent tumors and distant lesions. When new resections cannot be done, implantation of radiotherapy with IMR technique is used, which was the case of this patient.
CONCLUSIONS
Malignant ameloblastoma is a rare entity and its timely histopathological diagnosis, associated with radical surgical resection of both the primary tumor and the metastatic tumor, is the only option that can offer disease-free survival with adequate quality of life. Non-surgical alternatives, such as chemotherapy and radiotherapy, are only recommended as a palliative option for lesions that cannot be approached surgically or in unresectable tumor recurrence.
The case of malignant ameloblastoma with scalp metastases presented here, which is one of the few reported in the medical literature, stresses the need for adequate treatment planning, timely and regular follow-up in all patients with this pathology, as well as the implementation of the genetic profile in the histopathological study, which allows predicting a more aggressive behavior of this entity. It is worth noting that multiple surgical interventions or recurrences are a risk factor for malignant or metastatic ameloblastoma.














