INTRODUCTION
Although locally aggressive, unpredictable and rare in bone tissue, giant cell tumors (GCT) are increasingly common today, mostly affecting young adults, especially women, between 20 and 50 years of age, with a higher incidence in the Eastern population. GCTs account for 3-5% of bone tumors and 20% of benign tumors. 13 In Latin America they are more common in women and are more frequently located in the epiphyseal regions of long bones; however, they can also affect small bones of the hands and feet or, rarely, flat bones such as the skull. 4 This type of neoplasm involves mainly femoral condyles, tibial plateau, humerus head and distal radius but it could also be found in the vertebrae. If it manifests, the lumbar and sacral regions are involved. 5
X-rays show eccentric osteolytic metaphyseal lesion, whose edges may be either limited by sclerotic margin or ill-defined with destruction of the cortex and invasion of neighboring structures. GCT do not usually lead to periosteal reaction nor show trabeculation inside.
Other diagnostic methods, such as nuclear magnetic resonance, may be used to assess the tumor and possible soft tissue involvement. 6 Surgical treatment is necessary in all cases due to a possible metastatic disease depending on several risk factors still under study 7, but its high rate of recurrence, influenced both by the expression of certain genes and the neoplastic grading on the Campanacci scale 8, means that there is no consensus about its management. Incomplete resection of the tumor when the cortex is destroyed with invasion of nearby tissues causes recurrence in 2% to 25% of cases. People with GCT rarely develop lung metastases. 9
CASE PRESENTATION
37 year-old female patient, mestizo, from Quevedo (Ecuador) and low socioeconomic level who entered the emergency service after being transferred from another health center of less complexity. Relevant medical history includes a spinal tumor six months earlier.
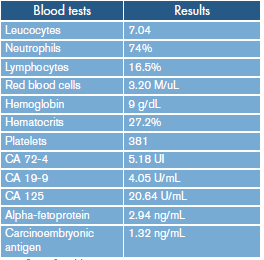
The patient presented with a clinical picture of seven days of evolution characterized by dyspnea during moderate efforts, cough with white expectoration, unquantified fever, loss of sensitivity in lower limbs (paraparesis), loss of sphincter control and weight loss. Physical examination revealed blood pressure of 110/60 mmHg, heart rate of 104 beats per minute, respiratory rate of 20 per minute, temperature of 38°C and oxygen saturation of 95%. Pale fascies, dry mucous membranes, symmetrical thorax, lung fields with abolished sounds in right pulmonary base, rhythmic and tachycardic heart sounds, atrophy of the muscles in the lower limbs, loss of sensitivity and soft, depressible and not painful abdomen on palpation were also observed. Complementary blood tests, tumor markers -considering her six-month history of spine tumor- and diagnostic imaging were requested (Table 1).
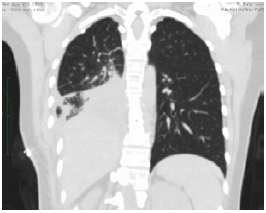
All blood tests were within normal parameters. Diagnostic imaging (Figure 1) showed a right paraspinal tumor in posterior mediastinum at the level of the eighth and ninth thoracic vertebra, with calcifications involving bone structures, posterior arch and expansive osteolytic lesions; a decrease in the vertebral bodies of T8-T9 was observed in bone window.
Source: Document obtained during the study.
Figure 1 High resolution computed tomography (CT) of the thorax in axial, coronal and sagittal planes.
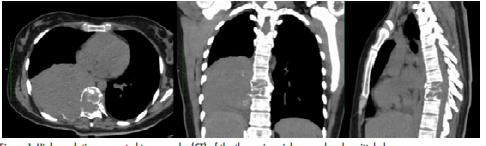
A magnetic resonance (MRI) of the dorsal spine was requested (Figure 2), revealing a right paravertebral mass of 9.9x10x9.4 cm that caused an osteolytic lesion in the vertebral body and lateral antlers of T8 and T9 topography, infiltrating through an intervertebral foramen into the medullary canal, and expansive lytic lesion in the topography of the posterior region of the ninth costal arch diaphysis.
Source: Document obtained during the study.
Figure 2 MRI of the dorsal spine, T2-weighted coronal plane and T1-weighted sagittal plane.
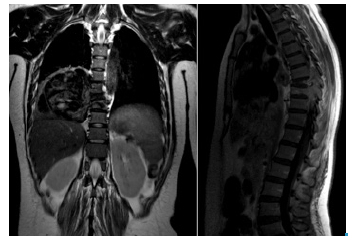
Based on the above data, the patient was scheduled for surgery, and entered the operating room for thoracotomy. During the perioperative period, right posterolateral thoracotomy was performed at the level of the seventh intercostal space; dissection was performed by planes until reaching the pleural space where a tumor was observed in the lower right pulmonary lobe with limited edges that involved the posterior part of the seventh to the tenth rib and T8-T9 vertebral bodies. A right inferior lobectomy plus partial resection of the costal wall, which includes the ribs mentioned above, was performed (Figure 3).
Source: Document obtained during the study.
Figure 3 Resection of the seventh, eighth and ninth rib plus right inferior lobectomy.
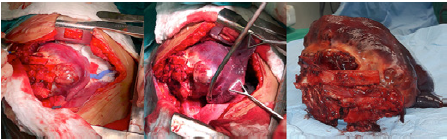
Skeletonization of vertebral bodies T8-T9, lower vertebral endplate of T7 and upper vertebral endplate of T10 was performed, revealing the involvement of the T8-T9 vertebral bodies and disc space. Resection of vertebral bodies T8-T9, disectomy in T7, T8 and T9, mesh placement with bone substitute over corpectomy space, closing of thoracic wall by planes and placement of polypropylene mesh (Figure 4) at the level of wall defect by costal resections were also performed.

Source: Document obtained during the study.
Figure 4 Placement of polypropylene mesh on wall defect after costal resections.
After the procedure, the woman entered the intensive care unit hemodynamically unstable and with vasopressor support, no evidence of bleeding and mechanical ventilation with PaO2/ FiO2 ratio of 350 and metabolic acidosis. On the fourth post-operative day, the patient was extubated; she woke up without vasopressor support, although she did not move actively her limbs and sat with assistance. The histopathology report described neoplastic proliferation characterized by mononuclear stromal cells, some with atypia, low mitotic count in stroma and multinucleated giant cells with 10 to 50 nuclei, reactive metaplastic bone and lymphovascular invasion. Immunostaining was positive for Ki-67 in 5% of stromal cells; CD 68 immunostaining was positive in giant cells. Vimentin was positive in stromal cells and giant cells; the histopathological diagnosis was locally aggressive GCT grade II.
On the tenth post-operative day, the patient was taken to intermediate care, where she remained calm, awake, with symmetrical thorax, surgical wound in good condition, hypoventilated pulmonary fields in right pulmonary base, paraparesis in lower limbs, muscle strength 2/4, and bilateral and hyporeflective anesthesia. A control CT was taken (Figure 5) showing pulmonary expansion and small amounts of pleural fluid with elevation of the right hemidiaphragm.
Source: Document obtained during the study.
Figure 5 Control CT scan that shows lung parenchyma window 10 days after surgery.
Furthermore, 14 days after inpatient surgery, a chest x-ray was performed (Figure 6), showing expanded right lung, small pleura effusion and adequate ossification process in the corpectomy space where the mesh was located. After six months, at the time of this publication, the patient fully recovered her strength, had full sensitivity and performed her daily activities.
DISCUSSION
GCTs of bone are rare and aggressive lesions 10 that mainly affect the metaphysis of long bones; they may involve the lumbar and sacral vertebrae on specific and infrequent occasions. According to sex and regarding the contextual approach in Latin America, this type of tumors affects more frequently women between 30 and 40 years of age. When the cortical bone is involved, it can also affect the soft tissues near the lesion due to continuity 11, and cause possible metastasis in <2% of the cases. 12,13
This was the case of a 37-year-old patient with a tumor mass in the thoracic vertebral bodies 8 and 9 of six month evolution, with invasion to the lower lobe of the right lung and to the diaphysis of the ninth rib. In this case, tumor activity is still under study considering that there is still pain in the area and rare consequences such as alterations in the functional performance of the affected limb. 14 Predominant symptomatology may include pain or neurologic deficit, which were observed in this patient as she suffered from back pain and lower limb paraparesis. However, as stated in other studies, it is evident that pain may last for a long time, even up to a year later. 15 The approaches reported in the literature describe total tumor resections 16, based on the Capanacci system, as the most frequently implemented. It consists of identifying and performing 1) intralesional curettage of intramedullary lesion confined to the bones, 2) wide excision of the cortex and 3) rupture of cortical bone.
This classification is necessary because treatment consists of intralesional excision by curettage plus bone graft and cement at stages I and II, and en bloc resection and reconstruction at stage III. 17 According to Sanerkin, GCTs are classified as follows:
Grade - I. Benign. Normal mitotic count, less than 5 mitoses per field, little or no nuclear atypia, no neoformed or scarce vascular tissue and no sarcomatoid cells are evident.
Grade II. Benign. Some abnormal mitoses, more than 5 mitoses per field of greatest increase, moderate nuclear atypia, moderate vascular-ization and absence of sarcomatoid cells.
Grade III. Malign. Abundant abnormal mitosis and nuclear atypia, great vascularization and presence of sarcomatoid cells.
Finally, the reported patient was diagnosed with GCT grade II according to the histological classification scale, identifying moderate benignity, vascularization and absence of sarcomatoid bodies. 18
For the case described here, based on CT findings, this was a stage III tumor with ruptured cortical cells, so radical corpectomy was performed with complementary stabilizations plus en bloc resection of the tumor. Refai et al.19 published a similar case in which the patient was treated for the first time with arterial embolization of the hypervascular region observed in angiography. Then, the patient underwent a transthoracic corpectomy in T7 in one stage, followed by reconstruction and stabilization of the anterior spine. According to the pathology report, this was a GCT grade II according to the Sanerkin classification, so the decision taken was the best for this case; in addition, radiotherapy was not required because the sample yielded a benign result.
On the other hand, it is worth mentioning that intervention variables were analyzed taking into account a series of GCT in adults treated with surgery plus radiotherapy and surgery alone, showing better prognosis. 20 Complementary radiotherapy should be considered, since the possibility of recurrence is 46% in patients who use this technique compared to 45% with radiotherapy only. There is a report with favorable results in which the lesion was treated with cryosurgery combined with radiotherapy. 21
CONCLUSIONS
GCTs are rare in the dorsal vertebrae. In some cases, when there is cortical involvement, metastasis can develop and complicate the patient's prognosis; therefore, a timely diagnosis is required to improve it.
The treatment for GCT should be determined based on the patient's clinic and the radiological study according to the Campanacci classification and also to the histological study according to the Sanerkin classification. Recommendations are en bloc resection for benign tumors, and resection plus radiotherapy for malignant tumors.