INTRODUCTION
Intussusception occurs when a part of the intestine and its mesentery slide into an adjacent intestinal segment. 1 It is most frequently observed in children, and only 5% to 16% of the cases occur in adults. 2 Currently, this neoplasm represents 1% of all causes of intestinal obstruction. 3,4
Inflammatory myofibroblastic tumor (IMT) is a rare mesenchymal neoplasm caused by the multiplication of spindle cells in variable inflammatory patterns. 5-8
Although the etiology of intussusception is unknown, previous surgeries, infections, trauma, immune reactions, radiation therapy and steroids have been suggested as probable causes. 9-11 The onset of this condition in 52% of cases is associated with malignant tumors and exacerbation of acute abdominal pain; in addition, data on pathological involvement have been obtained in the small intestine and, less frequently, in the colon and the gastroduodenal portion. Imaging studies help to make the diagnosis; however, exploratory laparotomy supports the diagnosis in 68% of cases. 12,13 It is worth mentioning that it can be confused with cancer due to similar clinical and imaging characteristics, causing difficulties in its subsequent treatment. 5,12
IMTs that extend through the gastric wall and into neighboring organs such as the esophagus, duodenum, pancreas, peritoneal cavity, and liver are known as inflammatory infiltrates and simulate malignancy in endoscopy and imaging. 7,13 Regarding management, despite pathological findings, it has been proven that complete resection is possible; this is the treatment of choice and is considered as a cure as symptoms and even recurrences tent to decrease. 6,14-16
CASE PRESENTATION
Female patient of 41 years, of mixed race, from the rural area of Babahoyo (Ecuador), housewife and of a low-income household who consulted for pain and abdominal distension associated with vomiting, constipation and diarrhea of three months of evolution prior to admission.
No relevant medical history was reported. Initial care provided found normal vital signs, and physical examination revealed general abdominal pain with response to deep palpation in mesogastrium and hypogastrium, abdominal distention and increased hydro-aeric sounds, accompanied by nausea that led to vomiting and diarrheic stools. Finally, laboratory results showed anemia and leukocytosis without additional blood tests.
Anteroposterior abdominal x-ray, in standing position and supine decubitus position, showed accentuated distension and dilatation of thin intestinal loops and hydro-aerial levels (Figure 1).

Source: Document obtained during the study.
Figure 1 X-ray of abdomen in standing position showing thin bowel loops with hydro-air levels.
Likewise, abdominal ultrasound reported concentric thickening of the wall of the ascending and transverse colon with preservation of the visualization of its layers (Figure 2).

Source: Document obtained during the study.
Figure 2 Concentric thickening of the colonic wall compatible with endoluminal tumor or intussusception.
Diffuse wall edema of the transverse ascending colon and splenic angle, image of invaginated appearance and space-occupying lesion at this level can be observed in abdomen and pelvis tomography (Figures 3 and 4).
Source: Document obtained during the study.
Figure 3 Crescent in doughnut sign. Imaging of oral phase showing enteroenteric intussusception. The arrow points the external muscularis of intussusception.
Source: Document obtained during the study.
Figura 4 A. Sausage pattern with alternate areas of low and high attenuation. B. Intraluminal lesion as the lead point of intussusception.
Based on the result of the admission examination, a diagnostic exploratory laparoscopy was performed to identify the location, causality and correct procedures of the treatment. During surgery, dilation of the small intestine was observed and the diagnosis of ascending intestinal intussusception was confirmed; due to uncontrollable bleeding, the procedure was converted to laparotomy (Figures 5 and 6).

Source: Document obtained during the study.
Figure 6 Intussusception of ascending bowel to transverse colon.
Resection of the segment of terminal ileum affected by the tumor mass and bowel transit reconstruction were performed by means of termino-terminal ileocolic anastomosis (Figure 7).
When analyzing the sample collected during surgery, a polypoid formation of 6cm of diameter, on a pedicle and ulcerated that occupied of 85% the lumen, with smooth and whitish external surface was observed. A homogeneous and elastic hard consistency was evident after cutting.
Then, histological cutting was performed (Figure 8) and taken to a laboratory where proliferation of spindle cells (which surround the vessels) and abundant inflammatory infiltrate were identified.
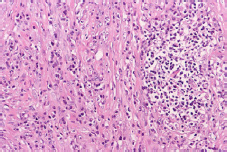
Source: Document obtained during the study.
Figure 8 Microscopy of the tumor segment in sectioned terminal ileum.
The definitive treatment in this case was surgical, that is to say, resecting the segment of intestine that had the tumor and restoring intestinal transit with termino-terminal ileocolic anastomosis. The patient had a good post-operative evolution and no adverse reaction; she was discharged six days after surgery, with favorable prognosis and without complications.
DISCUSSION
Intussusception in adults occurs after an aggression in the intestinal wall causes alteration of peristalsis, in turn leading to a proximal segment sliding into a distal segment. If the mesentery is involved, it causes vascular compression, wall edema and necrosis of the intestinal loop. Its etiology in 70-90% of cases is an organic lesion of malignant origin, frequently in the colon and small intestine. 17 57% of tumors that cause intussusception are benign, including myofibroblastic tumor, also known as granuloma; 30% of cases are malignant. The most common malignant tumor is melanoma and its metastases 18. Other less frequent causes are Meckel's diverticulum, adhesions or hematoma of the wall. 19
Nevertheless, adhesions are the most common extraluminal lesions; they originate after being pulled into an intestinal segment, which causes a fold and invagination into the segment that produces the pulsation due to the intestinal movement. 20 According to the location of the adhesions, and of intussusception in general, the lesions are classified into four categories: 1) enteroenteric (75% and with greater recurrence), 2) colocolic (14% recurrence), 3) ileocecal (8% recurrence) and 4) ileocolic (5% recurrence). 17,21
If the alteration is caused by the colon, the most common cause of intussusception is adenocarcinoma, followed by leiomyosarcoma, liposarcomas, reticular cell sarcoma and metastases. 22
It is important to assess symptoms and signs; those related to intestinal obstruction, according to frequency, are: colicky abdominal pain (75%-85%), nausea (50%), vomiting (30%) and constipation. Other less common symptoms include diarrhea, weight loss, melena, fever, and palpable abdominal mass. 17 The case reported here presented with abdominal pain and bloating. Because of these symptoms, diagnosis is made preoperatively only in a third of the cases, of which 50% are diagnosed as intestinal obstruction, 11% as abdominal tumor and 2-5% as bleeding in the digestive tract. 17
This correlates well with the ultrasound studies of the abdomen performed worldwide; target sign imaging have shown that it is possible to identify multiple thin, parallel, hypo-echoic and ecogenic layers in longitudinal planes. 23
Pathognomonic findings in tomography include bowel thinning, space-occupying lesion and an area of fat and vessel hyperdensity. The computed tomography (CT) performed on the reported patient showed diffuse edema of the transverse ascending colon wall and splenic angle, image of invaginated aspect and space-occupying lesion. 24 Nuclear Magnetic Resonance Morphology is similar to CT and consistent with other studies. 25
It is worth noting that surgical exploration is the main means of diagnosis and that, despite other simpler methods, it is the only one that allows providing a definitive treatment by intestinal resection and primary anastomosis with restoration of the intestinal transit. This is mostly curative and to some extent coincides with the literature and the surgical treatment provided to this patient, which was resection of the affected ileal segment and termino-terminal ileocolic anastomosis. 26
CONCLUSIONS
This case corresponds to a very rare cause of intussusception due to the specificity of the clinical presentation, the diagnosis and the immediate need for resection. It should be noted that the definitive diagnosis is made through a histopathological study. The pathophysiology of this disease is not correctly established yet, so this neoplasm is still under study.
















