INTRODUCTION
Hypofibrinogenemia is a congenital disorder consisting of low levels of fibrinogen, a key glycoprotein for the hemostasis system and inflammatory response. 1,2 This abnormality occurs as a result of a heterozygous mutation in one of the three genes encoding for the fibrinogen protein chains and autosomal recessive inheritance. There is no exact data on its incidence, since most patients are asymptomatic or do not have clinically significant bleeding. When severe hemorrhagic manifestations, such as gastrointestinal bleeding with unknown etiology, are observed, the corresponding studies should be carried out to look for the cause. 1,3-6
The severe form of hypofibrinogenemia is similar to afibrinogenemia 1, and also manifests itself mainly in the neonatal period, in 85% of cases through umbilical cord bleeding. Its presentation in older individuals is rare, and its hemorrhagic manifestations may be gastrointestinal, genitourinary, cutaneous, by spontaneous splenic rupture and central nervous system; the latter is the main cause of death in these patients. 2,3,5
To diagnose hypofibrinogenemia, immunoreactive fibrinogen levels are evaluated, obtaining results that show very low values that should be associated with prolonged clotting times. 1,2,7 Treatment in symptomatic individuals consists mainly of fibrinogen replacement therapy and strict daily follow-up of fibrinogen levels in plasma in order to ensure adequate hemostasis. 2,6 This is the report of an unusual hemorrhagic presentation (spontaneous vulvar hematoma) in an adult patient with a history of congenital hypofibrinogenemia.
CASE PRESENTATION
19-year-old female patient, from Bogotá (Colombia), housewife and of a low-income socioeconomic status household, with history of congenital hypofibrinogenemia diagnosed during the neonatal period in a hemorrhagic context (without information on a specific event), compatible genetic study confirmed in anamnesis (not available in clinical history), without hemorrhagic manifestations subsequent to diagnosis nor pharmacological treatment. The young woman consulted the emergency department due to clinical symptoms of six hours of evolution and spontaneous appearance of expansive genital hematoma at the level of the right labium majus with hemorrhage associated with dissection of superficial tissues and altered state of consciousness. The physical examination showed hemodynamic instability and signs of low expenditure, presence of hematoma of approximately 20cm in diameter at the level of the right labium majus and active hemorrhage in its medial and inferior portion (Figure 1).
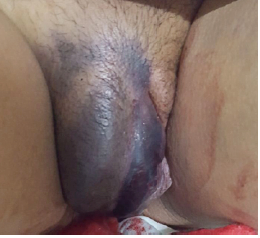
Source: Document obtained during the study.
Figure 1 Vulvar hematoma at the level of the right labium majus with active inferomedial hemorrhage.
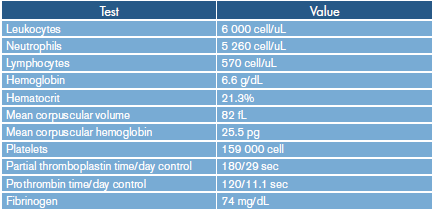
A hypovolemic shock secondary to major hemorrhage was considered, for which Ringer's lactate infusion 3 000mL for 2 hours was prescribed, as well as intravenous tranexamic acid 1g and compression at bleeding site. Laboratory tests on admission showed complete blood count with hemoglobin of 6.6 g/dL and no other alterations. Due to her history of hypofibrinogenemia, fibrinogen activity test was requested, which reported 74 mg/ dL associated with prolonged clotting times (Table 1); based on the results, the patient received a transfusion of six units of cryoprecipitates and two units of packaged red blood cells.
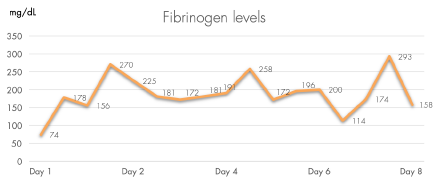
The patient was assessed by the gynecology service, which considered the benefit of immediate surgical management. The hematoma was drained with intra-surgical size estimated at 17x7cm without complications. The hematology service assessed her again, confirming menstrual cycles without alterations and absence of family history of coagulopathies, bleeding or complications during invasive procedures (no surgical history) and episodes of involuntary pregnancy loss. In the immediate post-operative period, fibrinogen supplementation was initiated with doses adjusted according to weight; the dose were subsequently adjusted based on the fibrinogen values in plasma obtained every 8 hours, with an average daily dose of approximately 1.5 to 2 grams, administered for 8 days (Figure 2).
The patient did not have any side effects to the administration of fibrinogen, and the treatment by intravenous administration was adequately tolerated without changes between doses until discharge from hospital.
DISCUSSION
Fibrinogen is a glycoprotein essential for hemostasis, and it is the soluble precursor of fibrin, which is required for clot formation; it also plays a key role on platelet aggregation and fibrinolysis. It is synthesized in the liver and circulates in plasma at concentrations of 2-4 g/L. 8-10
Hypofibrinogenemia is a rare hematologic disorder that has no established incidence due to the absence of symptoms in most affected patients; it has a recessive inheritance pattern as does afibrinogenemia. In patients with hemorrhages of unknown etiology, studies should look for coagulation disorders. 1,2 The hereditary abnormalities of fibrinogen are divided into two: type 1 or quantitative, and type 2 or qualitative. 11
The most frequent clinical manifestations of hypofibrinogenemia are umbilical cord hemorrhage, intracranial hemorrhage and mucosal hemorrhage; other less frequent manifestations are skeletal muscle hemorrhage, joint bleeds, paradoxical arterial and venous thrombotic events 9, ruptured spleen 3,12 and hepatic hematoma. 13 There are no reported cases describing spontaneous vulvar hematoma as a clinical manifestation.
For the case described here, the clinical history of the patient allowed guiding the diagnostic and treatment approach. However, it is important to highlight that an individual without a history of coagulopathy who presents unusual thrombotic or hemorrhagic events -which in some cases compromise life- must be a candidate for studies that include the evaluation of fibrinogen. Moreover, vulvar hematoma is a rare clinical finding in medicine, occurring mainly in obstetrics with an incidence of 1to 2 per 1 000 births 14, and even more rare in non-obstetric population with an incidence of 3.7%. 15 Although in both cases it is usually associated with perineal trauma, vulvovaginal hematomas can rarely be triggered by spontaneous injury to a blood vessel or result from a hematological disorder. 16 In this case, a hematological disorder caused an expansive vulvar hematoma in a patient with a history of congenital fibrinogen disorder.
First-line treatment for a vulvovaginal hematoma is usually conservative, especially when the hematoma has a small to moderate size; however, if the hematoma has expansive behavior 16,17 or is >12cm, it is usually associated with decreased hematocrit, hemodynamic disorders, and transfusion requirement, suggesting the need for surgical management. Still, there is no clear scientific evidence to support this approach and the optimal timing for surgical management remains controversial.
On the other hand, it has been suggested that if the size of the hematoma is sufficient to trigger urological or neurological symptoms 16 or if its behavior is clearly expansive, surgical management should be urgent. 16,17 This was the approach determined for the patient described, achieving early hemostasis and stabilization, and avoiding complications derived from the procedure. Hemostasis can be achieved by ligation of the bleeding vessels, but another hematoma may occur as a complication, and in this context, embolization of the compromised blood vessels should be chosen as the second line of treatment. 17
In the present case, transfusion of red blood cells concomitant to surgical management was necessary given the significant decrease in hemoglobin levels associated with hemodynamic instability.
The treatment of severe hemorrhages secondary to hypofibrinogenemia and afibrinogenemia is based on fibrinogen replacement, either with fresh frozen plasma, cryoprecipitate or concentrated fibrinogen, the latter being the treatment of choice due to its greater clinical safety. 8 Regarding fibrinogen concentrates replacement therapy as the mainstay of treatment for afibrinogenemia, it is recommended to individualize the clinical hemorrhagic context and the fibrinogen levels in plasma, aiming at a level not less than 75 mg/dL. 2,6,7 For the case described here, a dynamic dose of fibrinogen was indicated according to weight and with adjustment according to the plasmatic levels of fibrinogen evaluated every 8 hours during the entire hospital stay. This, along with surgical management and transfusion, allowed achieving a rapid and adequate clinical evolution, with discharge after 8 days of hospitalization without hemorrhagic recurrence, hemodynamic and hematological stability, and normal fibrinogen levels.
Given the impossibility of conducting large-scale studies on the treatment of fibrinogen disorders and their hemorrhagic manifestations, the best level of evidence available should be used for an early and appropriate approach; case reports are the main scientific contribution, and that is precisely the relevance of the information provided in this article.
The strengths of the current case report include the diagnostic and therapeutic approach of an unusual hemorrhagic presentation of hypofibrinogenemia that compromises life, highlighting the need, in this type of cases, for surgical management, transfusion and dynamic replacement of fibrinogen to prevent complications and seek the rapid improvement of the symptomatology. This is the first case of hypofibrinogenemia reported in Colombia, and the first in the world describing vulvar hematoma as a severe spontaneous hemorrhagic manifestation that compromises life.
The limitations of the study are the unavailability of the clinical history of the neonatal hemorrhagic event -which was useful to suspect the diagnosis- and the genetic studies carried out to confirm the diagnosis. Nevertheless, the lack of these data from the clinical history does not diminish the importance of what has been reported here, as this is the background anamnesis of the current clinical history described, with clarity and certainty, by the patient and her family, as is commonly observed during the evaluations made every day in the medical assistance field.
CONCLUSIONS
Afibrinogenemia is a rare disease that usually manifests itself with hemorrhagic events. Local control of such events includes supportive therapy, and fibrinogen replacement is the mainstay of therapy. It is important to suspect coagulation disorders in patients with bleeding at unusual sites, severe spontaneous bleeding, and unexpected thrombotic, obstetric, or adverse surgical events.
Having an adequate record of patients' clinical histories and their background information is essential to achieve a better diagnostic and therapeutic approach; in turn, this brings greater strength to the research and generates new knowledge, as all reported data could be relevant, this being one of the main lessons of the case report described here.