INTRODUCTION
Helminths are multicellular, eukaryotic invertebrates that may have tube-like or flattened bodies. They are divided into two major groups: Nematohelmynths and Platylhelmynths. 1 The latter is subdivided into other subgroups, of which the most medically relevant is the Cestoda class with species such as: Taenia solium, Taenia saginata, Taenia asiatica, Taenia multiceps, Hymenolepis nana, Diphyllobotrium latum and species of Echinococcus.2
In general, human infection and disease, known as cestodiasis, is asymptomatic or has unspecific symptomatology. 2,3 However, some reported signs, symptoms and sequelae include weight loss, abdominal pain 4,5, distress secondary to observing proglottids in feces 6, expulsion of proglottids through the nose 7, decreased school performance, student dropout 8, pernicious anemia 3, gallbladder perforation 9, appendicitis 10 and bowel obstruction. 11 Moreover, the most important clinical aspect, and the greatest clinical burden, is derived from the consumption of T. solium eggs, which can cause the subsequent infection and aberrant encystment of the larval stage in various areas of the human body including muscles, eyes and central nervous system; the latter, especially in cases of neurocysticercosis, produces the largest associated morbidity. 12 Infections can be acquired in two general modes; the first one is secondary to the ingestion of cysts from badly prepared meat such as pork (T. solium, T. asiatica) or beef (T. saginata) 13, and the second is associated with the ingestion of T. solium eggs that can produce cysticercosis. 12
Human taeniasis is one of the most important food-borne parasitic diseases, but it is preventable and treatable. 12 The Global Burden of Disease estimated that human cysticercosis by T. solium caused 503 000 disability-adjusted life years (DALYs) 14, although extrapolations based on these estimations suggest that they can be as high as 2.7 million. 15 On the other hand, in Colombia, the National Survey of Intestinal Parasitism found a prevalence of taeniasis of 0.08% in children (7-10 years old). 16 Additionally, estimates in intestinal parasitism indicate that more than 800 million children require treatment for these parasites. 17
Due to its association to poverty, lack of sanitation and poor hygienic practices, prevention includes good hygiene and improvement in sanitation, health education and life conditions. 17 A recent national study, which evaluated the residual incidence of taeniasis and cysticercosis through different methods, found that 3 626 cases were reported from 2009-2013, for a national crude rate of 7.7 cases per 100 000 inhabitants: 58.2% were males, 57% were over 40 years of age, and neurocysticercosis was found in 57.6% of the reported cases. 18
Diagnosis relies upon direct microscopy of expelled eggs or proglottids in feces. In this context, parasite-specific secretory antigens can be used for detection (Copro-Ag). 12 Treatment includes: niclosamide (2 g/person as a single dose) 19, praziquantel (5-10 mg/kg as a single dose) 20, tribendimidine (200mg <15 years or 400 mg per adult, single oral dose) 21, nitozoxanide (15 mg/kg/day for 3 days or 1.2g in a single dose) 22 and albendazole (3x400 mg/person for 3 consecutive days). 23
This paper presents a case of persistent taeniasis in a woman who reported having received multiple therapies without success, and aggravated by the fact that the primary therapy was not available in the country.
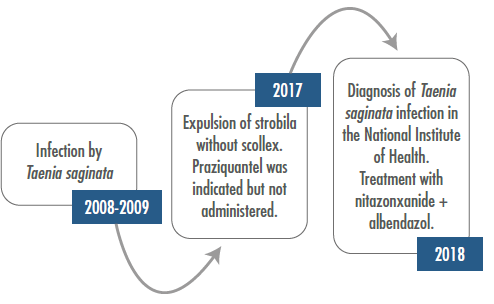
CASE REPORT
This is the case of a 31-year-old woman, mestizo, street-food seller, with incomplete high school studies, born and currently living in Bogotá. She reported a clinical history of 10 years of evolution, consisting of abdominal pain associated with flatulence, alteration of intestinal behavior, irritability, bruxism, weight loss and expulsion of what she described as small parasites. In August 2018, parasitological diagnosis revealed Taenia spp. after finding proglottids in fecal samples; proglottids were described as T. saginata with 12 or more branches.
Direct wet mounts and formol-ether concentration technique were performed. Following the standard routine, proglottids were washed with distilled water, fixed in 10% neutral buffered formalin, and stored at room temperature until histological processing; then uterine branches were counted under a light microscope at a magnification of 40x. Upon examination, proglottids were found and later identified as T. saginata (Figures 1 and 2). Proglottid morphology was of approximately 11mm in length and 8mm wide, and the received segment had around 18 uterine branches. Eggs were roughly 33 micrometers in diameter.
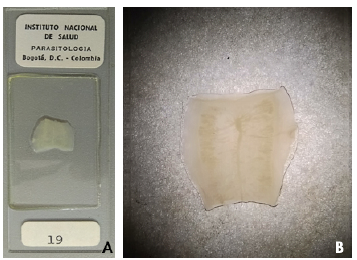
Source: Image obtained while conducting the study.
Figure 1 Proglottid found in the patient feces. A) Proglottid of Taenia saginata-; B) Proglottid of Taenia saginata.
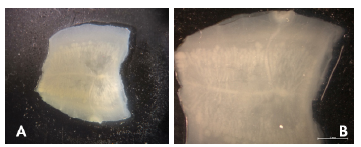
Source: Image obtained while conducting the study.
Figure 2 Proglottid found in the patient's feces. A) Proglottid of Taenia saginata 1X (stereoscope); B) Proglottid of Taenia saginata2x.
Her epidemiological history included the consumption of raw beef; the patient sells food in the street which has been prepared by her for several years. Physical examination revealed generalized mucocutaneous pallor, mild pain in the mesogastrium, presence of fragmented proglottids in the anus, and signs of excoriation in the perianal area. Laboratory blood exams showed only eosinophilia.
In spite of going repeatedly to medical consultation and having received multiple antiparasitic therapies -such as albendazole, secnidazole, pyrantel palmoate and several metronidazole schemes-, the symptomatology persisted. Due to the lack of improvement, she started to have alterations in her mood. In June 2017, she consulted for expulsion of an almost complete strobila (about 1m long) without scolex, later identified as T. saginata; management with praziquantel was indicated, although it is not available in Colombia. Symptomatology persisted despite the expulsion of the parasite.
During the medical appointment, the treating physician reviewed the anamnesis, which revealed multiple antiparasitic schemes, made a scientific literature review and checked the national availability of medications considering that the patient continued describing the expulsion of proglottids. In August 2018, the patient received an alternative treatment of nitazoxanide 500mg, twice a day, for 3 days in combination with albendazole 400mg per day, for 3 days. There were neither side effects nor abnormalities in laboratory parameters. After receiving this treatment, follow-up was performed at 1, 4, and 8 weeks in fecal samples to look for proglottids and to check the presence, number, and viability of Taenia eggs. Successful treatment was achieved because the patient expelled the worms and the eggs were not found in subsequent control stool cultures. General recommendations for hygiene and adequate cooking of meats were given.
DISCUSSION
This case report exposes two important clinical aspects. The first one is the difficulty of following and treating taeniasis in some cases. The second is the possibility of persistent or recurrent taeniasis in some people. This clinical situation can arise from two situations: 1) a possible increase in resistance to anti-parasitic drugs, and 2) the possibility of reinfection due to poor hygienic practices, which may be related to parasite species different from the one found in this patient. In this particular case, poor hygienic practices could have had dire consequences considering that the patient serves and manipulates food; this means that she could have been the node of secondary and self-limited infections, thus revealing the importance of adequate personal and food manipulation habits.
As human taeniasis is a zoonotic threat, with significant global prevalence and a large and underestimated impact on economy, agriculture and public health 24, more studies are required to estimate its real burden. Nevertheless, some epidemiological studies estimate a prevalence of taeniasis in Latin America between 0.24% and 17.25%. 12 This prevalence tends to vary according to the population and its economic, infrastructure, education, culture and hygiene conditions, as well as to the presence of farmed pigs and livestock. 12 Therefore, environmental health, animal health and human health must be addressed simultaneously, perhaps using the One Health approach. 25 In Colombia, specifically, one of the departments with the highest seroprevalence rates is Tolima, with an estimated prevalence of 17% for porcine cysticercosis and 43.4% for human taeniasis. 26 Likewise, seroprevalences as high as 40.19% have been estimated in other departments such as Vaupes, and others as low as 0.53% in Caldas. 27 It is worth mentioning that in Colombia no department is free of porcine cysticercosis due to poor livestock practices. 26
The majority of patients with taeniasis do not present symptoms or pathognomonic findings; occasionally, they have slight abdominal discomfort or alterations of intestinal habits, as well as peripheral eosinophilia. T. saginata infection may present more symptoms, compared with other species, due to its larger size and length. 28 Even as this is the case, the importance of differentiation between species lies in warning and preventing the serious complications that T. solium can cause, such as neurocysticercosis. 12
Regarding antiparasitic treatment, praziquantel 5-10 mg/kg or niclosamide 2g administered as a single dose, in association with the administration of a laxative, have become the drugs of choice. 13 These two drugs have shown effectiveness of 96% and 85%, respectively 29, and seem to be the most cost-effective treatments to manage taeniasis. 12 Praziquantel is, according to the literature, a better alternative than niclosamide in terms of cost, efficacy, availability and safety. 29 The literature reports only a few cases of unsuccessful treatment of T. saginata with praziquantel, although they have been effectively managed with nitazoxanide 30, which has shown to be effective and have a wide spectrum of action against parasites resistant to other medications. 22,30,31 Despite of the available evidence, there are few studies in vivo, because they were approved by the FDA only until 2002. 30 Although nitazoxanide is not considered the drug of choice due to a higher prevalence of mild side effects compared to praziquantel 22,32, it is a viable alternative. 22,32 On the other hand, albendazole is also an alternative, especially with a dose of 400mg for 3 consecutive days in adults, obtaining a success rate close to 100%. 23 Unfortunately, in several countries of Central and South America, where this disease could be considered endemic 27, praziquantel and niclosamide are not available. 33
In conclusion, this case draws attention to the great therapeutic support that is required to treat human taeniasis, as well as the alternatives for treatment when the drug of choice is not available. Other medications can be excellent alternatives for the community and the patient. However, there are still great challenges regarding prevention, education and control. The strengths of this case include the follow-up and adequate treatment of the patient, the literature search for therapeutic alternatives and the comprehensive clinical assessment of the patient. The weaknesses include the unavailability of the drug of choice and additional laboratory studies that could have contributed to better understanding this case.
CONCLUSION
This case draws attention to the difficulties in the follow-up and adequate treatment of patients with taeniasis. Furthermore it presents possible therapeutic alternatives when the drug of choice is not available. In terms of treatment solutions, multiple options of secondary, tertiary and combination drugs are available, which are effective and safe for treating taeniasis.
However, there is a need to increase diagnosis, prevention, education, control and treatment.
PATIENT'S PERSPECTIVE
The patient reports that she feels emotionally better and is hopeful that her symptoms will not recur. She says that she will follow the recommendations given to her, especially considering her work with food.